Extra-Palpebral Lichen Sclerosus and Corneal Refractive Surgery
Kyle Margulies1, Majid Moshirfar2,*, Brianna Ply2, Yasmyne C. Ronquillo2 and Phillip Hoopes2
1Medical Student, Department of Ophthalmology/Visual Sciences, A T Still University of Health Sciences, USA
2Department of Ophthalmology/Visual Sciences, University of Utah Hospital, USA
Received Date: 24/03/2023; Published Date: 27/06/2023
*Corresponding author: Majid Moshirfar, Department of Ophthalmology/Visual Sciences, University of Utah Hospital, USA
Abstract
Lichen Sclerosus (LS) is a complex chronic inflammatory disease characterized by hypopigmentation and atrophy of the skin. The disease commonly involves the anogenital region of males and females but is known to be found in extragenital regions such as the neck, shoulders, trunk, wrists, oral mucosa, and legs.
A literature search of PubMed, EBSCO, and Cochrane Library yielded 10 case reports of extra-palpebral LS. These patients presented with well-demarcated white plaques most commonly located on the patient’s right lower eyelid. Two cases were distinct in that they presented with ocular complications. One presented with acquired Brown syndrome and the other with keratoconjunctivitis sicca. Treatment consisted of either corticosteroids, tacrolimus, or skin graft, with outcomes ranging from no improvement to complete resolution.
This report is the first case of a patient with extra-palpebral LS undergoing a LASIK procedure. The patient presented with a hypopigmented lesion of the left lower eyelid. Like previous presentations, the patient's extra-palpebral LS had no clinical symptoms involving the eye and presented with no complications in surgery and had an excellent outcome three months post-op.
Keywords: Lichen; Sclerosus; Ocular; Refractive; Surgery; Extra-palpebral; Lasik
Introduction
Lichen Sclerosus (LS) is a complex chronic inflammatory disease characterized by hypopigmentation and atrophy of the skin. While the exact etiology and pathophysiology of the disease remain unclear, it is generally accepted as a T-cell mediated autoimmune disorder influenced by genetic, environmental, and physiological factors. LS is commonly associated with other auto-immune diseases such as vitiligo, autoimmune thyroiditis, alopecia areata, and pernicious anemia [1]. It is estimated that the prevalence of LS is between 1:300 and 1:1000, preferentially affecting women in the fifth or sixth decade of life [23]. The disease commonly involves the anogenital region of males and females but is known to be found in extragenital regions such as the neck, shoulders, trunk, wrists, oral mucosa, and legs [3]. Anogenital lesions typically produce painful pruritic lesions while extragenital lesions generally present as asymptomatic pale macules with a “cigarette paper” appearance and occasional pruritus [3]. One of the rarer manifestations of the disease involves the adnexa of the eye. This paper aims to determine the impact of adnexal LS on ocular surgeries such as LASIK, PRK, and cataract surgery.
Literature Search Method
A literature search of PubMed, EBSCO, and Cochrane Library was done using the terms lichen sclerosus, eye, orbital, and facial yielded 2286 results from 1968 to 2022, 10 of which were relevant. Articles with no ocular or orbital manifestation of lichen sclerosus were excluded. The literature review and associated references yielded 10 case reports. All articles were written in English.
Reported Cases in the Literature
In the ten reported cases of extra-palpebral LS, patients presented with well-demarcated white plaques most commonly located on the patient’s right lower eyelid. The average age of presentation was 40.60 +/- 16.58 years old, with a higher prevalence of females than males.
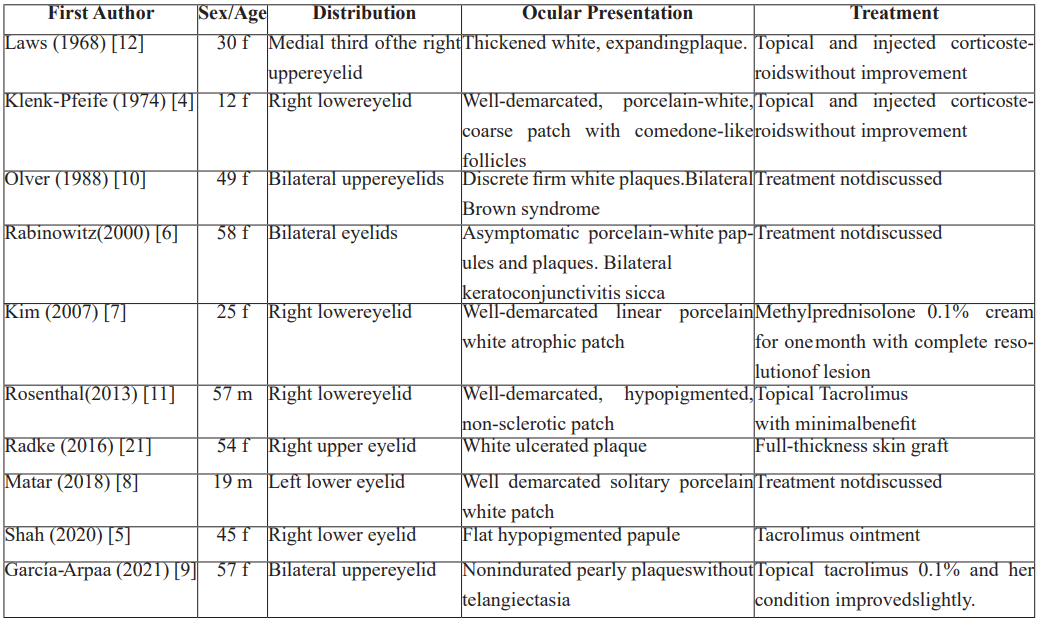
Table 1 outlines age, distribution, presentation, and treatment for all cases. Two cases were distinct in that they presented with ocular complications. One presented with acquired Brown syndrome and the other with keratoconjunctivitis sicca [4-12].
Rabinowitz et. al, reported a 58-year-old female patient who presented with decreased tear production and tear break-up time caused by meibomitis and meibomian gland inspissation. The meibomitis and inspissation were attributed to plaques with atrophic epidermis with keratotic plugging and histology deemed consistent with LS [6].
In a report by Olver, a 49-year-old female with a history of LS and morphea presented with the onset of diplopia and hypopigmented plaques on the upper eyelids the month following. The diplopia was diagnosed as Brown syndrome and the plaques as LS. The diplopia developed due to the overlaying fibrosis extending into the peri-sheath region around the trochlea, limiting passive movement of the superior oblique tendon in elevation in adduction. However, the dysfunction of the superior oblique muscle was attributed to her diagnosis of morphea, not LS [10].
The patients were treated with either corticosteroids, tacrolimus, or skin graft with outcomes ranging from no improvement to complete resolution (Table 1).
Case Report
A 38-year-old Caucasian female presented to an ophthalmologist for simultaneous bilateral LASIK surgery. The patient presented with uncorrected visual acuity of 20/200 OD and 20/300 OS. Upon inspection, a hypopigmented lesion involving the left lower lid and cheek was noted. The patient reported a long-standing history of lichen sclerosus, which involved her eyelid, trunk, and groin areas. The patient reported that the adnexal eye lesion was asymptomatic and was treated with Tacrolimus (Protopic) ointment as needed. The patient underwent uncomplicated bilateral femtosecond assisted LASIK for myopia and astigmatism correction.
Outcomes of the LASIK procedure included a best-corrected visual acuity of 20/15 OU and mild ocular dryness. At the three-month follow-up, the patient reported no adverse effects involving the extra-palpebral LS lesion and was counseled to use preservative-free artificial tears as needed for ocular dryness.
Discussion
Lichen sclerosus (LS) is a complex chronic inflammatory disease that commonly presents in women in their fifth or sixth decades. The disease commonly involves the anogenital region of males and females, but approximately 15% of LS patients present with extragenital lesions of the neck, shoulders, trunk, wrists, oral mucosa, and legs [3]. One rare manifestation of LS is the involvement of the eyelids which has been reported in ten cases. All reported cases were treated with either corticosteroids or tacrolimus, with outcomes ranging from no improvement to complete resolution.
This report is the first case of a patient with extra-palpebral LS undergoing a LASIK procedure. The patient presented with a hypopigmented lesion of the left lower eyelid. Like previous presentations, the patient's extra-palpebral LS had no clinical symptoms involving the eye and presented with no complications in surgery and had an excellent outcome three months post-op.
When assessing patients’ candidacy for ocular surgery (i.e., LASIK, PRK or Cataract surgery), it is imperative to identify possible contraindications or risk factors. It is important to note that in the ten reported cases of extra-palpebral LS, none of the presentations manifested with histological changes involving the conjunctiva, cornea, retina, or chambers of the eye. Although one patient presented with LS-induced keratoconjunctivitis sicca, severe cases of dry eye are only a relative contraindication for surgeries such as LASIK, PRK, or Cataract surgery. An evaluation for adequate tear production via the Schirmer tear test may be necessary for patients with eyelid-associated LS and a history of dry eye [13-15]. Management of dry eye should be undertaken even prior to corneal refractive surgery. Additionally, LS is associated with an increased risk of developing Squamous Cell Carcinoma (SCC). While there has only been one case of extragenital LS associated with SCC manifestation, none of the presentations reported transformation to SCC of the eyelid [16].
Differentiating extra-palpebral LS from other similarly presenting pathologies is critical in reducing ocular surgery morbidities. No ocular manifestations of LS have been reported to date;
However, many other pathologies presenting with a hypopigmented eyelid lesion may cause ocular complications. The differential diagnosis for hypopigmented lesions of the eyelid includes leprosy, morphea, sarcoidosis, systemic scleroderma, vitiligo, tinea versicolor, and lichen planus [4,10,17-19]. Some autoimmune diseases such as sarcoidosis are associated with impaired immune functions and are at greater risk for infection, dry eye, and other adverse side effects associated with ocular surgery [18]. Others, such as morphea (localized scleroderma), can have significant ocular involvement and cause anterior segment inflammation and anterior uveitis [20]. Patients with lichen planus can result in complications ranging from conjunctival scarring to blepharitis [19].
Utilizing a multidisciplinary approach including specialists in internal medicine, dermatology, and pathology is advised to appropriately diagnose unknown lesions and assess any risk factors that may affect ocular surgery outcomes.
Conclusion
Hypopigmented extragenital lesions are a rare complication of LS but are generally benign. With no serious ocular complications associated with previous cases, patients with extra-palpebral LS may undergo procedures such as LASIK after a comprehensive physical examination and history.
References
- Fistarol SK, Itin PH. Diagnosis and treatment of lichen sclerosus: an update. Am J Clin Dermatol. 2013;14(1):27-47. doi:10.1007/S40257-012-0006-4.
- Fergus KB, Lee AW, Baradaran N, et al. Pathophysiology, Clinical Manifestations, and Treatment of Lichen Sclerosus: A Systematic Review. Urology. 2020;135:11-19. doi:10.1016/J.UROLOGY.2019.09.034
- Murphy R. Lichen Sclerosus. Dermatol Clin. 2010;28(4):707-715. doi:10.1016/J.DET.2010.07.006
- Klenk-Pfeifer E. Lichen sclerosus et atrophicus of face in a 12-year-old girl. Z Hautkr. 1974;49:841.
- Shah CT, Mandell JW, Kirzhner M. Lichen sclerosus of the eyelid. Cutis. 2020;106(3):E16-E17. doi:10.12788/CUTIS.0097
- Rabinowitz R, Rosenthal G, Yerushalmy J, Lifshitz T. Keratoconjunctivitis sicca associated with lichen sclerosus at atrophicus. Eye (Lond). 2000;14 ( Pt 1)(1):103-104. doi:10.1038/EYE.2000.25
- Kim YJ, Lee ES. Case of sequentially occurring lesions of facial lichen sclerosus following the lines of Blaschko. Journal of Dermatology. 2007;34(3):201-204. doi:10.1111/J.1346-8138.2007.00250.X
- Matar A, Zu Elfakkar N, Abdallah M, el Husseiny R. Infraorbital lichen sclerosus et QJM. 2018;111(1):16-17.
- García-Arpa M, Franco-Muñoz M, Ramos-Rodríguez C, Sánchez-Caminero MP. Lichen Sclerosus on the Eyelids. Actas Dermo-Sifiliográficas (English Edition). 2021;112(2):179. doi:10.1016/J.ADENGL.2020.12.018
- Olver J, And ’, Laidler2 P. Acquired Brown’s syndrome in a patient with combined lichen sclerosus et atrophicus and morphoea. British Journal of Ophthalmology. 1988;72:552- doi:10.1136/bjo.72.7.552
- Rosenthal IM, Taube JM, Nelson DL, Erdag A case of infraorbital lichen sclerosus. Dermatol Online J. 2013;19(10). doi:10.5070/D31910020021
- Laws HW, Kalz F. Lichen Sclerosus et Atrophicus of the Eyelid. Can J Ophthalmol, 39-42 (1968).
- Zhao PF, Zhou YH, Hu Y bin, et al. Evaluation of preoperative dry eye in people undergoing corneal refractive surgery to correct myopia. Int J Ophthalmol. 2021;14(7):1047. doi:10.18240/IJO.2021.07.13
- Labetoulle M, Rousseau A, Baudouin C. Management of dry eye disease to optimize cataract surgery outcomes: Two tables for a daily clinical practice. J Fr Ophtalmol. 2019;42(8):907-912. doi:10.1016/J.JFO.2019.03.032
- Rabina G, Boguslavsky II, Mimouni M, Kaiserman I. The Association between Preoperative Dry Eye Symptoms and Postoperative Discomfort in Patients Underwent Photorefractive J Ophthalmol. 2019;2019. doi:10.1155/2019/7029858
- Sergeant A, Vernall N, MacKintosh LJ, McHenry P, Leman JA. Squamous cell carcinoma arising in extragenital lichen sclerosus. Clin Exp Dermatol. 2009;34(7):e278-e279. doi:10.1111/J.1365-2230.2008.03195.X
- Fett N. Scleroderma: nomenclature, etiology, pathogenesis, prognosis, and treatments: facts and controversies. Clin Dermatol. 2013;31(4):432-437. doi:10.1016/J.CLINDERMATOL.2013.01.010
- Danza A, Ruiz-Irastorza G. Infection risk in systemic lupus erythematosus patients: susceptibility factors and preventive strategies. Lupus. 2013;22(12):1286-1294. doi:10.1177/0961203313493032
- Journal O, Moshirfar M, Liu HY, et al. Special Care in Lichen Planus Patients Undergoing LASIK: A Review Article. Medical Hypothesis, Discovery and Innovation in Ophthalmology. 2019;8(3):134. Accessed May 17, /pmc/articles/PMC6778465/
- Fett N. Scleroderma: nomenclature, etiology, pathogenesis, prognosis, and treatments: facts and controversies. Clin Dermatol. 2013;31(4):432-437. doi:10.1016/J.CLINDERMATOL.2013.01.010
- Radke PM, Maltry AC, Mokhtarzadeh A, Harrison AR. A Unique Ocular Presentation of Extragenital Lichen Sclerosus. Ophthalmic Plast Reconstr Surg. 2017;33(3S):S56-S58. doi:10.1097/IOP.0000000000000662

