Abnormal Insertion of the Cystic Duct in the Duodenum
El Bakouri Abdelilah1,2,*, Ahmed Elmi Abdirahim1,2, Bouali Mounir1,2, Bensardi Fatima-zahra1,2, El Hattabi Khalid1,2 and Fadil Abdelaziz1,2
1Visceral emergency service, Department of general surgery, University hospital centre Ibn Rochd, Casablanca, Morocco
2Faculty of Medecine and Pharmacy, Hassan II University, Casablanca, Morocco
Received Date: 22/03/2023; Published Date: 21/06/2023
*Corresponding author: El Bakouri Abdelilah, Visceral emergency service, Department of general surgery, University hospital centre Ibn Rochd, Faculty of Medecine and Pharmacy, Hassan II University Casablanca, Morocco
Abstract
Anatomical variations of the cystic duct are common and frequently encountered. Different variations of the cystic duct are reported in the literature depending on its length, path and site of insertion. Failure to recognise some of these variations can lead to complications during surgery. All this requires anatomical knowledge and good intraoperative exploration to avoid traumatizing a noble organ.
We report on a 48-year-old female patient who was admitted with clinical cholestasis syndrome. On general examination, the patient was conscious 15/15 and hemodynamically and respiratory stable. On abdominal examination, a slightly tender abdomen was found with an unremarkable rectal exam. The hepatic balance was disturbed. On radiological examination, the thoracic-abdominal-pelvic CT scan showed a locally advanced pancreatic head process, responsible for a bi-canal dilatation. The patient underwent retrograde cholecystectomy, latero-lateral choledochodenal diversion with segment III liver biopsy and subhepatic drainage with a delbet blade. On investigation, there was moderate ascites, a liver with metastases (segment III biopsy done and positive for invasive adenocarcinoma), a tumor mass opposite the head of the pancreas fixed to the deep plane and locally advanced measuring 5cm in length, the main bile duct dilated to about 2cm and an undistended gallbladder with an abnormal cystic duct outlet at the duodenum.
We would like to share a very difficult clinical case and our experience with the support of the literature.
Keywords: Cystic duct; Duodenum; Anatomical; Surgery
Introduction
Anatomical variations of the cystic ducts are common and frequently encountered. Different variations of the cystic duct are reported in the literature as a function of its length, course and site of insertion. Failure to recognise some of these variants can lead to complications during surgery [1].
We report on a 48-year-old female patient who was admitted with clinical cholestasis syndrome. On general examination, the patient was conscious 15/15 and hemodynamically and respiratory stable. On abdominal examination, a slightly tender abdomen was found with an unremarkable rectal exam. The hepatic balance was disturbed. On radiological examination, the thoracic-abdominal-pelvic CT scan showed a locally advanced pancreatic head process, responsible for a bi-canal dilatation. The patient underwent retrograde cholecystectomy, latero-lateral choledochodenal diversion with segment III liver biopsy and subhepatic drainage with a delbet blade. On investigation, there was moderate ascites, a liver with metastases (segment III biopsy done and positive for invasive adenocarcinoma), a tumor mass opposite the head of the pancreas fixed to the deep plane and locally advanced measuring 5cm in length, the main bile duct dilated to about 2cm and an undistended gallbladder with an abnormal cystic duct outlet at the duodenum.
Case Report
The patient was 48 years old and had no previous medical history. She was admitted with a clinical cholestasis syndrome consisting of jaundice, dark urine and discoloured stools without other associated signs. The whole evolving in a context of fever and alteration of general state. The patient was conscious 15/15, hemodynamically and respiratminal examination, there was mild epigastric tenderness with scratchy lesions. On rectal examination, the finger pad came back soiled with discoloured stool. The rest of the somatic examination was unremarkable. On biological examination, the haemoglobin was 13.3 g/dl, the leucocyte count 8740/mm3, the platelet count 308,000/mm3 and the CRP was negative at 2.2 mg/l. On liver function tests, total bilirubin was above 250 mg/l, conjugated bilirubin above 150 mg/l and free bilirubin above 100 mg/l. On radiological examination, the thoracic-abdominal-pelvic CT scan (Figure 1) showed a locally advanced pancreatic head process, measuring 38x36 mm extended to 39 mm, responsible for a bi-canal dilatation from which the main bile duct measures 18 mm in diameter and the main pancreatic duct 6 mm in diameter.
The patient underwent retrograde cholecystectomy, latero-lateral choledochodenal diversion with segment III liver biopsy and subhepatic drainage with a delbet blade. On exploration, we found a moderate amount of ascites, a liver full of metastases (segment III biopsy done and positive for invasive adenocarcinoma), a tumour mass opposite the head of the pancreas fixed to the deep plane and locally advanced measuring 5cm in long axis, the main bile duct dilated to about 2cm and an undistended gallbladder with an abnormal cystic duct outlet at the level of the duodenum (Figure 2).
The postoperative course was simple. The patient was declared discharged after removal of the delbet blade with a letter to the oncology department and with a 6-month follow-up.

Figure 1: shows us the process of the locally advanced pancreatic head.
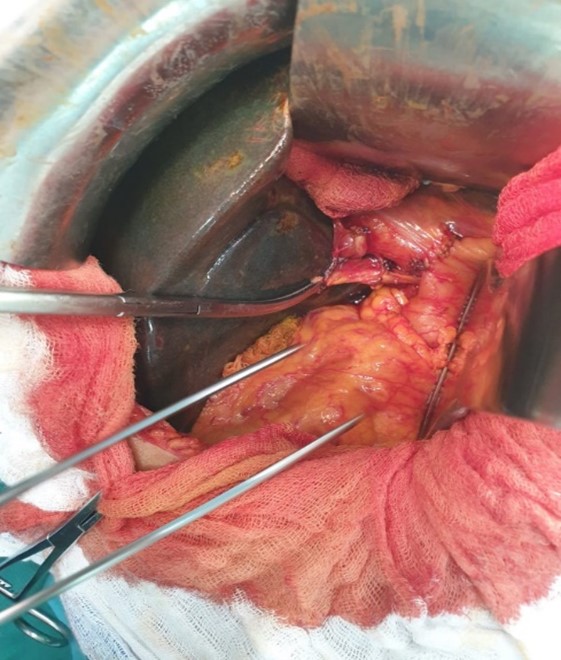
Figure 2: Also shows the abnormal termination of the cystic duct into the duodenum after cholecystectomy.
Discussion
Variations in the anatomy of the cystic duct are common findings in imaging studies and cholecystectomy reports, occurring in 18%-23% of individuals [2].
Bile duct injury is a serious complication during cholecystectomy, more commonly seen in laparoscopic cholecystectomy. One of the major causes of bile duct injury is failure to identify the ductal anatomy, articularly in the presence of anatomical variants [1].
There may be variable length of cystic duct, variable course, and variable insertion. Any failure to recognize these variations may lead to ductal ligation, biliary leaks or strictures after laparoscopic cholecystectomy [3].
Awareness of this anomaly will enable radiologists to avoid misinterpretation of images and surgeons to reduce complications [4].
But the diagnosis of this anomaly depends on correct intraoperative exploration for exact confirmation [5].
Because of the aberrant anatomy, double cystic duct cases predispose patients to higher risks of complications and converting laparotomy [6].
Prior knowledge of the presence of such a variation would not only prevent accidental injury to the accessory canal during surgery, but would also be helpful in managing postoperative wound drainage in such cases [7].
Conclusion
Cystic duct variations are not uncommon and it is important to recognize the anatomical variations [1].
Surgeons need to be aware of the variations in length of the cystic duct and the different ways in which the cystic duct travels and is inserted when performing high risk operations [3].
I hope this study would give meticulous and comprehensive information to the surgeons about the variations of cystic duct for doing cholecystectomy successfully.
Conflicts of interest: The authors declare no conflict of interest.
Acknowledgements: I thank my lord first of all. I also thank my teachers and my patients who gave me confidence. All authors contributed to the conduct of this work. All authors also declare that they have read and approved the final version of the manuscript.
Author contribution: All the authors have contributed to this work in a serious way and a big thank you for everyone.
Ethical approval: None required.
Funding: Nothing to declare.
References
- Sarawagi R, Sundar S, Gupta SK, Raghuwanshi S. Anatomical Variations of Cystic Ducts in Magnetic Resonance Cholangiopancreatography and Clinical Implications. Radiology Research and Practice, 7.
- Ojo AS, Pollard A. Risk of Gallstone Formation in Aberrant Extrahepatic Biliary Tract Anatomy: A Review of Literature, 2020.
- Sangameswaran K. Variations of Cystic Duct and Its Clinical Significance. IJAR, 2021; 9(4): 8120‑8126.
- Nayak SB, Shetty SD, Surendran S, Jetti R, Kumar N, Sirasanagandla SR. Double gallbladder completely enclosed in a cystogastric fold of peritoneum. Anat Cell Biol, 2014; 47(2): 132.
- Zhang J, Hu Z, Lin X, Zhang D, Wang H, Chen B. Case Report: Isolated Cystic Dilatation of the Cystic Duct: A Misdiagnosed Case Preoperatively. Front Surg, 2021; 8: 686629.
- Otaibi W, Quach G, Burke B. Double Cystic Duct in a Septated Gallbladder. Journal of Investigative Medicine High Impact Case Reports, 2015; 3(2): 232470961557910.
- Aristotle S, Jebakani CF. A duplication of the cystic duct - case report, 4.

