Caecal Mixed Adenoneuroendocrine Carcinoma (MANEC) with Hepatic Metastasis –a Rare Case of Neoplasia of Colo-rectal
Fizzah Arif*, Muhammad Arsalan Khan, Shah Muhammad, Syed Haider Mehdi and Abdaal Waseem Khan
Department of General Surgery, Sindh Institute of Urology and Transplantation, Karachi, Sindh, Pakistan
Received Date: 21/03/2023; Published Date: 20/06/2023
*Corresponding author: Fizzah Arif, MBBS, Department of General Surgery, Sindh Institute of Urology and Transplantation, Karachi, Sindh, Pakistan
Abstract
Mixed Aden Neuro Endocrine Carcinoma (MANEC) is a rare tumor of cecum with prevalence of 3.2%. MANEC contains at least 30% neuroendocrine cells and 30% Aden carcinomatous cells. This tumor is aggressive with high potential of metastasis and has been reported at various locations like esophagus, colon, rectum, gallbladder, pancreas etc.
We present a case of high-grade MANEC of the cecum that presented as intestinal perforation with metastasis in 3/10 lymph nodes followed by development of hepatic metastasis.
Keywords: Ileocecal valve; Neuroendocrine tumor; Mixed adeno-neuroendocrine tumor; Metastasis; Adenocarcinoma; Oncology
Introduction
Mixed Aden Neuroendocrine Carcinoma (MANEC) of cecum is a rare type of carcinoma of the digestive tract which was first described by Cardier in 1924. MANECs constitute 3-9.6% of colorectal carcinomas [1] and has also been reported in various other organs like gallbladder, pancreas and esophagus. This tumor consists of dual components of adenocarcinoma and neuroendocrine carcinoma, with at least 30% of cells of each type present. Diagnosis of this tumor is based on histopathology and immunohistochemistry analysis due to its unique architecture [2]. In 2010, World Health Organization classified it as neoplasia with Aden neuroendocrine characters excluding other tumors from MANEC like Goblet Cell Carcinoid (GCC), mixed endocrine-exocrine tumor [3]. According to one of the histogenesis theory, these tumors are believed to arise from multi-potent stem cells that differentiates into two different cell lineages [4]. Treatment lacks standardization due to variable clinical and histological presentation.
This is a case of a high-grade mixed adenocarcinoma/neuroendocrine tumor of the cecum that presented as cecal perforation with no prior symptoms and later the patient developed hepatic metastasis within 2 months of initial presentation of disease.
Case Presentation
A 38-years-old female with no known co-morbids presented to the Emergency Room (ER) with complaints of severe right iliac fossa pain, nausea and vomiting. On physical examination, patient was tachycardic and abdomen was distended, and mild tenderness was present, gut sounds were inaudible. Ultrasound abdomen showed thick wall, non-motile blind ended bowel segment in right iliac fossa with surrounding moderate amount of free fluid and adjacent distended non motile bowel segments. Computed Tomography (CT) abdomen/pelvis (Figure 1) showed pneumoperitoneum along with dilated small bowel loops due to small bowel obstruction with caecal perforation. Thickened ileocaecal region with maximum wall thickness 10 mm. Liver normal with no focal intrahepatic lesion. Minimal ascitic fluid.

Figure 1: CT scan abdomen showing dilated small bowel loops with pneumoperitoneum. Liver is normal with no metastatic deposit.
Patient underwent exploratory laparotomy and right hemicolectomy and diversion ileostomy formation. Histopathology of surgical specimen showed large cell, high grade Mixed adenoneuroendocrine carcinoma (MANEC) of Caecum (tumor size = 2.5 x 2.5 x 2 cm) with no lymph vascular or perineural invasion identified however, mesoappendix shows lymph vascular invasion. Proximal resection margin was 12 cm, Distal resection margin was 3 cm and circumferential margins were 3 cm. The pathological TNM classification was pT3b, N1b with metastasis in 3/15 lymph nodes. Microscopic analysis revealed collision pattern of glandular component and eosinophilic cells (Figure 2). Immunohistochemistry markers were positive for CK7, CK20, synaptophysin and chromogranin. Ki-67 was positive in 90% of tumor cells (Figure 3). CEA and CA19-9 were sent post-surgery which were within normal limits.

Figure 2: A. Low magnification view shows a collision pattern, of an infiltrating neoplastic lesion. B. High magnification view: Glandular component of the tumor with intra luminal mucin and scattered sheets of round blue cells with atypical glands. C. High magnification view: Tumor is invading the muscularis propria and reaching upto subserosal fat. D. At high magnification, the neuroendocrine component is eosinophilic cells with hyperchromatic, pleomorphic nuclei and prominent nucleoli arranged in sheets and cords.

Figure 3: Lymph node involvement by tumor can be seen. Immunohistochemistry markers applied showed CK20- Patchy positive, Ki-67%- Strong positive in 90% cells, CK 7 – focal positive, Synaptophysin – Patchy positive, Chromogranin -Positive.
Patient was discharged with follow up plan, however she was lost to follow up. She presented in outpatient department, 2 months after surgery with abdominal pain and decrease appetite and significant weight loss. Repeat CT CAP was performed that showed multiple hepatic metastatic deposits (Figure 4). Positron emission tomography-computed tomography (PET-CT) showed enlarged liver with multiple non enhancing radiotracer avid focal lesion largest one in segment VIII measuring 1.8 cm. Case was discussed in multidisciplinary tumor board meeting and decision for palliative chemotherapy for patient was made considering the multifocality of liver metastasis. She was referred to medical oncology department where she was started on Cisplatin and Etoposide.
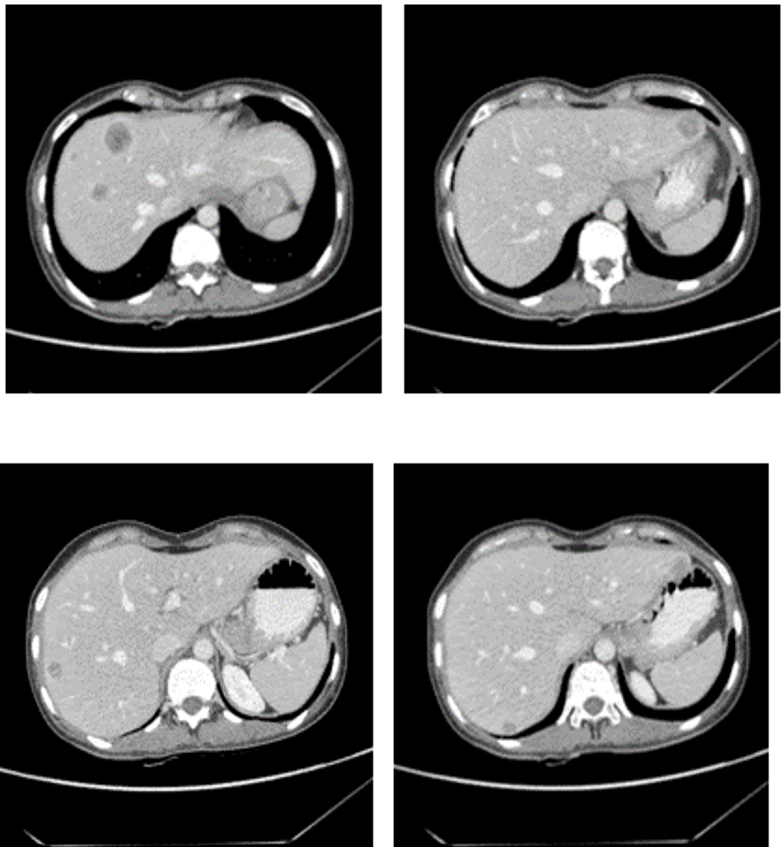
Figure 4: CT scan performed on follow up visit after 2 months showing multiple hepatic metastatic deposits in different segments.
Discussion
MANECs originating from caecum are extremely rare and only eight cases have been reported in literature. Caecum MANEC were commonly seen in sixth decade of life in females in all previously reported cases [2].
Mixed adenoneuroendocrine carcinomas were previously referred as ‘argentaffin cells tumor’ [5], ‘amphicrine tumors’, ‘collision tumors’, ‘exocrine neuroendocrine carcinomas’ and ‘combined tumors’ [2].
In 2010, World Health Organization (WHO) identified it as a separate pathology with neuroendocrine and gland-forming epithelial features eliminating all prior confusing nomenclature [3]. Most of the endocrine cell carcinomas of colorectal comprise of MANEC, [5] with a prevalence of 3.2 % [6]. These tumors are clinically occult and usually present as acute abdomen secondary to intestinal obstruction or perforation [1]. There are no specific tumor markers and CEA, CA19-9, and CA125 levels are all within normal limits [1,2].
Two morphological patterns of MANEC that are seen include: collision and composite types. ‘Collision variant’ are those in which both component of tumor is in close contact whereas in ‘composite or mixed variant’, endocrine and exocrine components are intermixed. This is believed to be either due to multi directional transformation of a single neoplasm in or origination from two separate adjacent neoplasms [1]. Prolong inflammatory bowel disease is a risk factor for this cancer, as the underlying pathophysiology involves differentiation of multipotent stem cells [2].
On histopathological basis, MANECs are further classified into high, intermediate and low grade. ‘High grade carcinomas’ are composed of adenoma/ carcinoma with poorly differentiated neuroendocrine tumor (small, intermediate or large cell type). ‘Intermediate grade’ MANECs include mixed adenocarcinoma neuroendocrine tumor and amphicrine carcinoma. ‘Low grade’ MANECs include mixed adenocarcinoma neuroendocrine tumor (MANETs) [2]. Grossly, these tumors can range from polyps, ulcers, stenotic lesions. Neuroendocrine component of it resembles small or large cell neuroendocrine tumors of the lungs [1].
European society of neuroendocrine tumors recommends application of two immunohistochemical markers while analysis for MANEC: Chromogranin (CgA) and Synaptophysin (Syn). Chromogranin (CgA) is found to be positive in 52.4 % tumors and Synaptophysin (Syn) is positive in 84% tumors. Presence of CD117 is a poor prognostic marker [6]. For adenocarcinomatous component, CD 133 positivity is seen in 47% cases and is associated with tumor aggressiveness [4]
No practice guidelines have been established for management of MANEC due to rarity of the condition. MANECs with higher adenocarcinoma component have good prognosis compared to the tumors with low adenocarcinoma component [5]. Considering neuroendocrine component, well differentiated variant should be managed on lines of colorectal adenocarcinomas and poorly differentiated variant needs to be managed as neuroendocrine carcinoma [7]. Surgical resection is the recommended therapeutic strategy for both primary tumor as well as metastases. In case of distant metastases, resection should be planned post neoadjuvant chemotherapy [2]. Adjuvant chemotherapy plays an important role in survival [6]. The National Comprehensive Cancer Network recommends cisplatin/carboplatin and etoposide [7]. These are associated with 67% response rate [2]. Due to similar histology to small cell carcinoma of lungs, platinum-based adjuvant chemotherapy is also used in treatment of these cancers [2].
Overall, the prognosis remains poor as it is often metastatic at the time of diagnosis and the median survival time is 7-10 months [7].
Conclusion
Mixed Aden Neuroendocrine Carcinoma (MANEC) is a neoplasm rarely seen in general population and is diagnosed when it has already metastasized, making neoadjuvant chemotherapy, an important component in management of this highly aggressive tumor.
Funding Sources: This research did not receive any specific grant from funding agencies in the public, commercial, or not for- profit sectors.
Conflict of Interest: None
Acknowledgements: None
Ethical approval: This study is exempted from any ethical approval by SIUT-Ethical Review Committee (SIUT-ERC)
Author’s contribution:
FA: Conceived and designed the study, conducted research, provided research materials, and collected and organized data and analyzed and interpreted data.
MAK: Conceived and designed the study, and organized data and analyzed and interpreted data. Wrote initial and final draft of article.
SM: Conceived and designed the study, conducted research. Provided research materials.
SHM: Conceived and designed the study, conducted research and provided research materials.
AWK: Conceived and designed the study, conducted research and provided research materials.
All authors have critically reviewed and approved the final draft and are responsible for the content and similarity index of the manuscript.
References
- Jain Aditi, et al. “Mixed adenoneuroendocrine carcinoma of cecum: a rare entity.” Journal of clinical imaging science, 2013; 3(10).
- Gonzalez Hector H, et al. “A Rare Case of Mixed Adenoneuroendocrine Carcinoma of the Ileocecal Valve.” Cureus, 2019; 11(1): e3942.
- Tanaka Toshiaki, et al. “Diagnosis, Assessment, and Therapeutic Strategy for Colorectal Mixed Adenoneuroendocrine Carcinoma.” Karger Publishers, 2017.
- Gurzu Simona, et al. “Mixed adenoneuroendocrine carcinoma of gastrointestinal tract: report of two cases.” World journal of gastroenterology, 2015; 21(4): 1329-1333.
- Shin SH, Kim SH, Jung SH, et al. High-Grade Mixed Adenoneuroendocrine Carcinoma in the Cecum: A Case Report. Ann Coloproctol, 2017; 33(1): 39–42.
- Paspala, Anna et al. “Management of MANEC of the colon and rectum: A comprehensive review of the literature.” Molecular and clinical oncology, 2018; 9(2): 219-222.
- Cherbanyk F, Gassend JL, Dimitrief M, Andrejevic-Blant S, Martinet O, Pezzetta E. A Rare Type of Colorectal Cancer: Mixed Adeno-Neuroendocrine Carcinoma (MANEC), 2017.

