The Role of ERCP in the diagnosis of Postcholecystectomy Cholangitis
Shaniah Holder1,*, Jordan Fondots2, Marie Wisa Beauge3, Melyssa James3 and Frederick Tiesenga4
1American University of Barbados School of Medicine, Barbados
2Saint James School of Medicine, Anguilla
3Saint George’s University School of Medicine, Grenada
4Department of Surgery, Community First Hospital, USA
Received Date: 17/03/2023; Published Date: 07/06/2023
*Corresponding author: Shaniah Holder, 1Department of Medicine, American University of Barbados School of Medicine, Barbados
Abstract
Cholangitis arises due to blockage and subsequent infection of the biliary ducts. It is normally a sequela of cholelithiasis and warrants laparoscopic cholecystectomy due to the risk of mortality. Cholangitis may also occur in patients after cholecystectomy and the etiologies vary from intrahepatic to extrahepatic causes. Normally, when presented with symptoms indicating gallbladder pathology, ultrasound is the initial and confirmatory diagnostic test. However, when the gallbladder is absent, Endoscopic Retrograde Cholangiopancreatography (ERCP) is the gold standard diagnostic test of choice. It is a minimally invasive procedure that allows the visualization of the biliary ducts to find the disorder's underlying cause. Certain criteria must be met before considering ERCP in a patient, and many limitations and contraindications prevent persons from undergoing this procedure. This report aims to describe the various etiologies and features of postcholecystectomy cholangitis and explore the gold standard diagnostic test, ERCP.
Keywords: Cholecystectomy; Cholangitis; Postcholecystectomy syndrome; ERCP; Primary stones; Pancreatic mass
Introduction
Approximately 20 million Americans suffer from gallstone disease [1]. There are three major types of stones: (i) Black Pigment stones, (ii) Brown pigment stones, and (iii) Cholesterol stones, which are the most common and form due to increased cholesterol levels in the blood [2]. Cholelithiasis is normally asymptomatic, however, if a stone becomes trapped in the biliary ducts, this can lead to many complications, including symptomatic cholelithiasis, cholecystitis, cholangitis, and pancreatitis [3].
Cholangitis is a life-threatening condition caused by an ascending bacterial infection of the biliary tree [4]. It can either arise due to autoimmune or infectious etiologies. Some autoimmune variants include Primary Biliary Cholangitis, IgG4-related Autoimmune Cholangitis, and Primary Sclerosing Cholangitis [4]. The most common nonimmunologic type is Acute Bacterial Cholangitis, which is usually caused by a partial or complete obstruction of the biliary system by a stone allowing infection and inflammation of the bile ducts [4]. The gold standard management of this condition is cholecystectomy [5].
In some cases, cholangitis may arise after cholecystectomy. This is known as Post-Cholecystectomy Syndrome and is caused by biliary stasis due to primary stone formation in the liver [3]. When the stone travels into the common bile duct and becomes stuck, this can obstruct biliary flow, allowing bacterial accumulation and infection [3]. Cholangitis affects 200,000 people annually in the United States and develops in individuals in their 5th and 6th decades of life [3]. Approximately 6% to 9% of hospitalized patients with gallstone disease have acute cholangitis [3]. 10% of patients who undergo laparoscopic cholecystectomy develop post-cholecystectomy complications like cholangitis [6]. Symptoms can present days to years after the procedure and resemble biliary colic [6].
In these cases, a high index of clinical suspicion is required and the diagnosis is usually made by considering the clinical presentation, laboratory results, and imaging studies [3,4]. Endoscopic Retrograde Cholangiopancreatography (ERCP) is a definitive diagnostic tool useful in differentiating the possible causes of post-cholecystectomy cholangitis [3]. Although this minimally invasive procedure may allow timely diagnosis and swift treatment, risks, complications, and contraindications limit its use. We present the case of a 70-year-old female who presented to the Emergency Department (ED) with Reynold’s Pentad, suspicious for cholangitis where the use of ERCP was warranted.
Case Presentation
We present the case of a 70-year-old female who presented to the ED following a syncopal episode. She had a Past Medical History (PMHx) significant for End-Stage Renal Disease (ESRD) requiring hemodialysis, Congestive Heart Failure (CHF), and Diabetes Mellitus, (DM) with a past surgical history remarkable for cholecystectomy. The patient stated that a few days before the fall, she had subjective fevers, abdominal pain, nausea, and loss of appetite. She denied vomiting, chest pain, or shortness of breath but endorsed generalized weakness. Vital signs were remarkable for hypotension with a blood pressure of 74/45 mmHg and tachycardia with a heart rate of 105 beats per minute; other vitals were within normal range. During the physical examination, the patient had jaundice and tenderness to palpation in the epigastric and right upper quadrant regions of the abdomen with mild guarding. Laboratory results showed hyperbilirubinemia, transaminitis, and leukocytosis. (Table 1) below shows the values of the liver enzymes, bilirubin, and blood cell counts.
Table 1: Laboratory results showed acute hyperbilirubinemia, elevated liver function enzymes, and leukocytosis.

After ruling out cranial trauma with a head computed tomography (CT), a right upper quadrant ultrasound (U/S) was conducted to assess her abdominal pain. Results showed hepatomegaly with evidence of prior cholecystectomy. The biliary ducts were not dilated, however, due to the elevated ALP, it was suggested by the gastroenterology team to conduct an ERCP to rule out any primary stones in the ducts or malignancy. (Figure 1) below highlights the U/S findings.
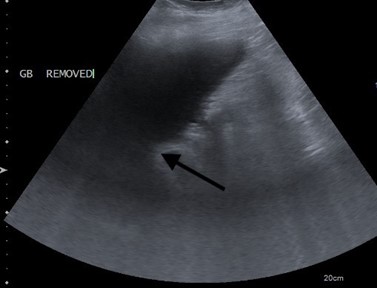
Figure 1: Enlarged liver with a right hepatic lobe measuring 20 centimeters and space signifying an absent gallbladder.
The patient was admitted for septic shock due to suspected cholangitis and began a regimen of prophylactic piperacillin-tazobactam, metronidazole, and vancomycin. On the day the patient was scheduled to undergo the ERCP, the laboratory test found an elevated international normalized ratio (INR) of 3.9, elevated prothrombin time of 34.9 seconds, and rising leukocytosis (white blood cells = 31.2 μK/L). It was suspected that acute hepatic failure was the cause of this change in values, therefore, a hepatitis panel and doppler of the hepatic and portal veins were ordered. However, before the tests and medical optimization could be conducted, the patient’s condition deteriorated with a new onset of altered mental status, slurred speech, and unequal pupils. The patient subsequently coded and ultimately expired despite resuscitative efforts.
Discussion
The primary etiology of ascending cholangitis is the obstruction of the biliary and pancreatic ducts allowing biliary stasis and microbial overgrowth [7]. The possible causes of post-cholecystectomy cholangitis range from pancreatic and biliary neoplasms, primary biliary stones from the liver, postoperative or autoimmune strictures, choledochal cysts, and biliary manipulation with ERCP or Percutaneous Transhepatic Cholangiogram (PTC) [7]. Charcot's triad encompasses the clinical features associated with cholangitis and consists of Right Upper Quadrant (RUQ) abdominal pain, jaundice, and fever [8]. The presence of symptoms of shock such as hypotension and tachycardia, and Altered Mental Status (AMS) make up Reynolds’ Pentad [8].
The initial diagnostic steps to diagnose cholangitis include RUQ ultrasound, and laboratory tests with a focus on leukocyte levels, serum transaminases, and bilirubin concentration [9]. The clinical picture formed by these results also acts as the alternative method of the diagnosis of acute cholangitis, whereas ERCP, PTC, and CT scans are then confirmatory [10]. In the setting of classical symptomatic presentation and lab results remarkable for obstruction and infection, the confirmatory tests, ERCP or PTC can be used to assess the underlying cause of obstruction [9]. ERCP is the initial test of choice due to its minimal invasiveness and decreased risk of hemoperitoneum and bile peritonitis when compared with PTC [11].
ERCP is characterized by advancing an endoscope orally into the duodenum [9]. After the endoscope has reached the duodenal papillae, cannulation, and fluoroscopy with contrast dye are conducted to allow radiographic visualization of the biliary and pancreatic tree structures for possible stones, strictures, or visceral masses that may cause extra ductal obstruction [9]. This tool is not only diagnostic but also therapeutic. Interventions are determined by the indications and include tissue sampling, removal of stones, fluid collection drainage, and tract repair via stent placement to restore ductal integrity [9]. Indications for ERCP include obstructive jaundice, neoplasms, stones, strictures, cysts, and ductal leakage [8]. In this case, the patient had obstructive jaundice characterized by elevated ALP and jaundice warranting ERCP. Although ERCP is therapeutic for acute obstructive cholangitis, in some cases, it increases the risk of acute cholangitis, making it the most common infectious adverse effect, and pancreatitis which is the most common noninfectious adverse event [12].
There are some contraindications to ERCP. These include i) bowel perforation, ii) unstable cardiac, pulmonary, or neurologic status, iii) altered gastrointestinal anatomy following gastric bypass procedure, and iv) severe uncorrected coagulopathy with an INR of >1.5 [13]. In this case, the patient’s INR was 3.9 and remained elevated despite numerous plasma transfusions. The presence of these contraindications may delay treatment and lead to complications ranging from worsening biliary symptoms to severe organ dysfunction involving the cardiovascular, nervous, respiratory, renal, hepatic, or hematological systems [14]. Some diagnostic alternatives to ERCP include endoscopic ultrasound (EUS) percutaneous cholangiography and Magnetic Resonance Cholangiopancreatography (MRCP) [15]. PTC, T-tube placement via laparotomy, and supportive management with antibiotics and fluids are notable alternative treatment options for ERCP [7]. In addition to medicinal therapy with antibiotics, ERCP remains the premier diagnostic and therapeutic mode of management of post-cholecystectomy cholangitis. Although the patient’s history and presentation and laboratory findings indicated that the best next step was ERCP, there were too many contraindications in this patient such as heart failure and increased PT and INR due to possible hepatic failure. It is important to implement medical optimization quickly to stabilize the patient and find alternatives for swift diagnosis and timely treatment in the management of post-cholecystectomy cholangitis.
Conclusion
Cholangitis is a life-threatening condition with many fatal consequences. It is normally treated with cholecystectomy and in some cases, may recur after the procedure. Primary stone formation, malignancy, and strictures are common causes of post-cholecystectomy cholangitis and can be differentiated using the diagnostic tool ERCP. ERCP is also therapeutic when managing acute obstructive cholangitis caused by stones or strictures. In the cases of high INR, bowel perforation, and cardiopulmonary instability, ERCP is contraindicated. In these cases, alternatives such as MRCP may be used. A high index of clinical suspicion is required when a postcholecystectomy patient presents with RUQ pain, fever, jaundice, altered mental status, and hypotension. Physicians must evaluate swiftly with the appropriate laboratory and imaging tests to assess if the patient would make a suitable candidate for ERCP. It is also paramount to know the alternative diagnostic and therapeutic modes of management if ERCP cannot be conducted. This will prevent a decline in health and improve the patient’s quality of life.
Author Contributions
Shaniah Holder: Concept and Design of study, Acquisition of data, drafting article, revising article. Guarantor Author
Jordan Fondots: Acquisition of data, drafting article, revising article
Marie Wisa Beauge: Concept and Design of study, intellectual content, revising article
Melyssa James: Acquisition of data, drafting article, revising article
Frederick Tiesenga: Final Approval, Intellectual Content, revising article
Informed Consent: A signed statement of informed consent was obtained for publication of the details of this case.
Competing Interests: None
Grant Information: None
References
- World Gastroenterology Organisation (WGO). World Gastroenterology Organisation (WGO), 2023.
- Everhart JE, Khare M, Hill M, Maurer KR. Prevalence and ethnic differences in gallbladder disease in the United States. Gastroenterology, 1999; 117(3): 632-639.
- Tanaja J, Lopez RA, Meer JM. Cholelithiasis. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2022.
- Virgile J, Marathi R. Cholangitis. [Updated 2022 Jul 4]. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2022.
- Soper NJ, Stockmann PT, Dunnegan DL, Ashley SW. Laparoscopic cholecystectomy. The new 'gold standard'? Arch Surg, 1992; 127(8): 917-921
- Zackria R, Lopez RA. Postcholecystectomy Syndrome. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing, 2022.
- Ganti L. Step-Up to USMLE Step 2 CK. Lippincott Williams & Wilkins, 2019.
- Frossard JL, Bonvin F. Charcot’s triad. International Journal of Emergency Medicine, 2011; 4.
- Meseeha M, Attia M. Endoscopic Retrograde Cholangiopancreatography. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2022.
- Girometti R, Brondani G, Cereser L, Como G, Del Pin M, Bazzocchi M, et al. post-cholecystectomy syndrome: spectrum of biliary findings at magnetic resonance cholangiopancreatography. Br J Radiol, 2010; 83(988): 351-361.
- Dawood A. Percutaneous Transhepatic Cholangiography: Background, Indications, Contraindications. Medscape, 2023.
- Andrea Tringali, PhDSilvano Loperfido, Guido Costamagna. Infectious adverse events related to endoscopic retrograde cholangiopancreatography (ERCP), 2023.
- Mukherjee J. Endoscopic Retrograde Cholangiopancreatography (ERCP): Indications, Patient Preparation and Complications. Gastro Flash, 2016; 2(3).
- Wada K, Takada T, Kawarada Y, et al. Diagnostic criteria and severity assessment of acute cholangitis: Tokyo Guidelines. J Hepatobiliary Pancreat Surg, 2007;14(1): 52-58.
- ERCP Information: Failed ERCP. (2013), 2023.

