Spontaneous Regression of Hepatocellular Cancer
Mohamed Omara Ibrahim Hussien*, Muhammad Farooq Latif, Yahia Labib ElDoky and Syed Hammad Tirmazy
Department of Oncology, Dubai Hospital, Dubai, UAE
Received Date: 13/03/2023; Published Date: 02/06/2023
*Corresponding author: Dr. Mohamed Omara Ibrahim Hussien, Department of Oncology, Dubai Hospital, Al Khaleej st, Al Baraha, Dubai, UAE
Abstract
We present a case of Spontaneous regression of advanced Hepatocellular Carcinoma (HCC) 15 x 16 cm associated with partial portal vein thrombosis in addition to multiple small para-cardiac Lymph Nodes. Baseline AFP levels above 50,000.0 IU/ML.
Post Exploratory laparotomy for extended hepatectomy in May 2022 however the surgery was abandoned due to extensive disease. Patient was not deemed suitable for any local intervention including TACE. Hence, he was offered systemic treatment with Atezolizumab and bevacizumab.
Surprisingly the Pre-treatment laboratory investigations revealed significant drop of AFP level to 70.2 IU/ML. Repeat CT scans showed a remarkable reduction of liver mass to 8 x 6.3 x 6 cm with complete resolution of the para-cardiac Lymph Nodes and the portal vein thrombosis. Hence the patient declined any systemic treatment however agreed for close monitoring. Last CT scan in September 2022 showed further regression in the liver mass to 5.7 x 4.5 cm.
Keywords: Case Report; Spontaneous Regression; Hepatocellular Cancer
Introduction
Hepatocellular Carcinoma (HCC) is the most common primary liver tumor and is the third most common cause of cancer related mortality worldwide. Many patients are diagnosed at an advanced stage and carry poor prognosis despite the advances in recent treatment modalities. The 5-year survival unfortunately remains poor [1].
Spontaneous Regression (SR) of malignancy refers to the partial or complete disappearance of primary or secondary tumors in the absence of any active oncological treatment. It is a rare phenomenon, however many case reports and case series reported SR in various malignancies including Breast cancer, kidney, cancer and thoracic malignancies. Spontaneous regression of HCC is extremely rare. Etiology is often unknown but several theories have been postulated including hypoxia, immunological reactions or both [2,3]. We report a case of spontaneous regression of HCC which was deemed unresectable and carried a very poor outcome.
Case Report
A 57-year-old male patient, presented to the Emergency Department in April, 2022 with 3 months history of worsening right hypochondrial pain and swelling. He reported a lack of appetite and weight loss of around 15 kg over this period. There was no history of fever or chills, altered bowel or bladder habits. Past medical history included type 2 Diabetes Mellitus and hypertension controlled on oral hypoglycemics and antihypertensive medications. He denied smoking and alcohol consumption. He was diagnosed to have Hepatitis-C Virus (HCV) infection in 2011 however no evidence of advanced fibrosis and sustained virologic response.
Initial investigations reported elevated levels of aspartate aminotransferase (Doubled) 81 IU/l (Normal range, 0-40 IU/l) and alkaline phosphatase level of 150 IU/l (normal range, 40–129 IU/l). The level of Alpha-fetoprotein (AFP) was significantly elevated, with values of more than 50,000.0 IU/ML (normal level, less than 5.8 IU/ML). Hepatitis C Antibodies were reactive; however, Hepatitis C Monitor (Quantitative PCR) was Negative (Undetectable) confirming the history of treated HCV. Child-Pugh score was Classified as “A”.
Contrast-enhanced computed tomography (CT) of the chest, abdomen and pelvis showed left lobe bulky heterogeneous enhancement with central hypodense lesions measures 15 x 16 x 16 cm suggesting HCC with loss of fat planes between the mass and the stomach (Figure 1), Scans also showed portal vein intraluminal partial filling defect indicating partial thrombosis in addition to multiple small paracardiac Lymph Nodes suggestive of metastatic disease.
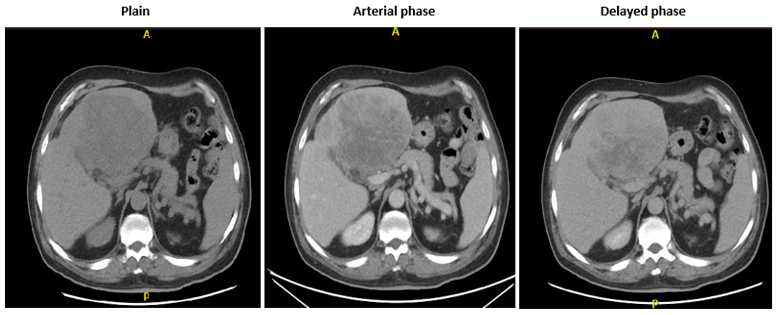
Figure 1: Contrast-enhanced Computed Tomography (CT) of the chest, abdomen and pelvis. It revealed left lobe bulky heterogenous enhancement with central hypodense lesions measures 15 x 16 x 16 cm suggesting HCC.
The upper Gastro intestinal endoscopy showed antral gastritis but did not show any evidence of varices or tumor infiltration in the stomach or the Duodenum. Colonoscopy was unremarkable.
Patient underwent Exploratory laparotomy for extended hepatectomy in Mid- May 2022 and the intraoperative findings revealed; Cirrhotic appearance of the liver with large tumor involving both left and right lobes with exophytic growth from the liver infiltrating the Pylorus, the Duodenum as well as the hepatic flexure of the Colon. Surgery was abandoned in view of extensive disease.
Patient was not deemed suitable for any local intervention including TACE. After post-operative recovery the patient was discharged home with outpatient Oncology clinic appointment for consideration of palliative systemic therapy. However, on his first oncology clinic assessment he reported a significant improvement in his right hypochondrial pain. He was offered first line systemic treatment with Atezolizumab and bevacizumab.
Pre-treatment laboratory investigations surprisingly revealed: Significant drop of AFP level to 70.2 IU/ML (normal level, less than 5.8 IU/ML); from more than 50,000.0 IU/ML – 7 weeks earlier. Alkaline phosphatase and aspartate aminotransferase were normalized as well.
Repeat Contrast-enhanced CT of the chest, abdomen and pelvis showed a remarkable reduction of liver mass size that became 8 x 6.3 x 6 cm from 15 x 16 x 16 cm previously. The loss of fat planes between the mass and the stomach showed no remarkable difference (Figure 2). The previously reported partial vein thrombosis as well as the multiple small paracardiac Lymph Nodes have completely resolved.

Figure 2: Contrast-enhanced CT of the chest, abdomen and pelvis after 2 months interval revealed: Remarkable reduction of liver mass size with query postoperative changes in the form of outline irregularities and anterior abdominal wall surgical marks.
In view of above findings, the patient declined any systemic treatment however agreed for close monitoring. The patient was kept on regular follow up on a monthly basis with clinical and laboratory assessment and follow up CT scans every 2 months.
Four weeks later, AFP dropped down to normal level 2.4 IU/ML (normal level, less than 5.8 IU/ML) and the patient reported disappearance of the right Hypochondrial pain and started to gain weight as well.
Subsequent AFP level remained in the normal range with further reduction to 1.7 IU/ML and his liver function test remained normal as well.
Repeat Contrast-enhanced CT of the chest, abdomen and pelvis in September 2022 showed further regression in the size of the previously seen ill-defined lesion involving the left lobe of the liver became 5.7 x 4.5 x 4 cm, the portal vein thrombosis and the paracardiac Lymph Nodes remained non-visible.
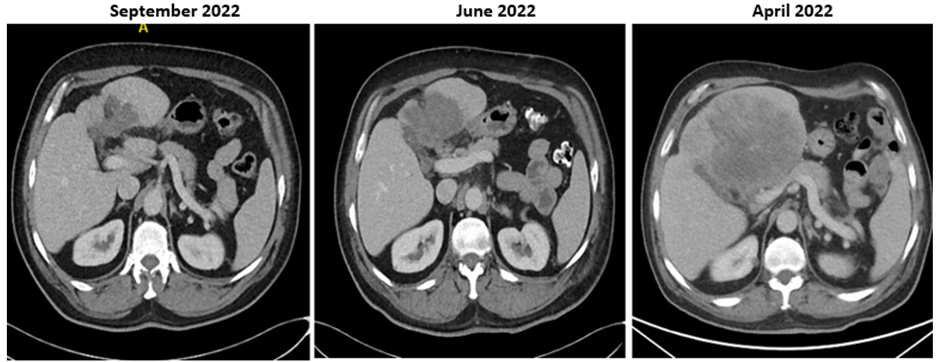
Figure 3: Serial of Contrast-enhanced CT of the chest, abdomen and pelvis showing remarkable regression of HCC.
The patient was last seen in the clinic in December 2022 and he remained asymptomatic. His liver function test remained normal as well as AFP which was 1.2 IU/ML. Repeat CT scan revealed: further regression of the size of the hepatic focal lesion that became 2.6 x 4.5x 4 cm.
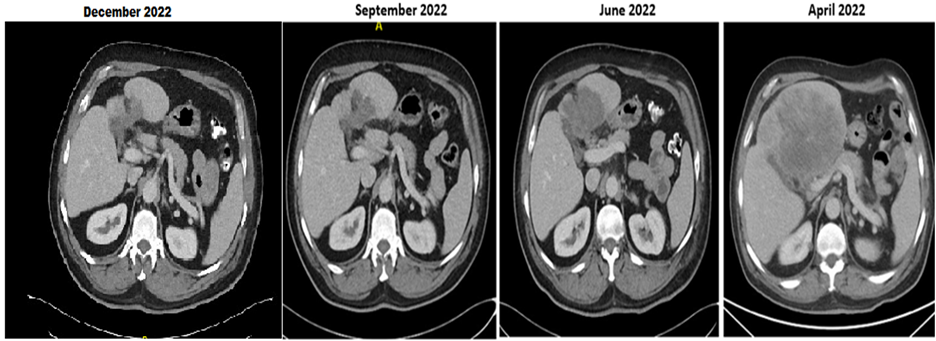
Figure 4: Further regression of the size of the hepatic focal lesion that became 2.6 x 4.5 x 4 cm in 12/2022 from 15 x 16 x 16 cm in 04/2022.
Discussion
Hepatobiliary cancers are the 6th most frequently diagnosed cancers worldwide. Approximately 75 percent of primary liver tumors are Hepatocellular Carcinoma (HCC). It is also the third most common cause of cancer-related mortality worldwide. Male to female ratio is 4 or 5:1 [1].
Major risk factors for development of HCC include chronic alcohol consumption. hepatitis B, hepatitis C and nonalcoholic fatty liver disease.
There is global variation in the incidence of HCC due to the incidence of risk factors. Serum Alpha-Fetoprotein (AFP) and ultrasound scan of the Liver are the most commonly used screening tools however serum level of AFP may not always correlate to tumor growth and can be normal in many cases. Generally, values over 400 ng/mL are highly suspicious of HCC in 20% patients [4].
Contrary to most solid tumors, the diagnosis of HCC can be made on imaging in patients with cirrhosis and biopsy is frequently not indicated to confirm the diagnosis prior to treatment. The imaging findings suggestive of HCC include non-rim arterial phase hyperenhancement, washout on portal venous and/or delayed phases, and capsule appearance in a lesion ≥1 cm [4].
Spontaneous Regression (SR) of malignant neoplasms is a rare, but well-documented phenomenon. It is defined as a partial or complete disappearance of malignant tumors without use of definitive treatment that aim for prevention / inhibition of tumor growth [5]. The theory of indirect induction of Spontaneous regression as a treatment strategy was documented thousands of years back in the Ebers Papyrus of 1550 BCE, one of the oldest Egyptian medical documents written during 1550 BCE that describes cures for various diseases. An Egyptian physician, Imhotep, recommended the application of poultice on tumor followed by an incision to induce an infection at the affected area [6]. The infection could promote tumor regression.
In 1959, Everson and Cole first described the Spontaneous regression of cancer as ’the partial or complete disappearance of a malignant tumor in the absence of any treatment, or in the presence of therapy which is considered to be adequate to have any significant treatment effect [5]. Spontaneous regression is well documented in certain malignancies such as renal cell carcinoma, neuroblastoma and choriocarcinoma. However, spontaneous regression of HCC is extremely rare and the true incidence is unknown. It is estimated in some reports to be less than 0.5% of patients. In 1972, Johnson and colleagues first reported spontaneous regression of biopsy proven HCC in a 3-year-old girl [7].
Etiology of spontaneous regression of HCC is largely unknown. Several theories have been suggested to explain this phenomenon including; use of certain herbal treatment, or the withdrawal of a potential causative factor like Alcohol or tobacco [2,3]. Tumor hypoxia and systemic inflammatory response have also been postulated as potential mechanisms [8].
Tumor ischemia possibly occurs due to interruption of the blood supply feeding the tumor which can be caused by portal vein thrombosis, disruption of the hepatic artery or hemorrhagic shock. This potential mechanism can be supported by the tumor regression response that could be achieved with some treatment modalities like Trans Arterial Chemoembolization (TACE) and antiangiogenic therapies [8]. Another proposed mechanism is the activation of the systemic inflammatory response that can potentiate the production of interferon (IFN)-gamma and natural killer cells leading to development of a cytotoxicity in the cancer cells [9].
Ricci et al also postulated several factors associated with spontaneous regression of malignant tumors including apoptosis, the immune system and tumor microenvironment for example presence of inhibitors of metalloproteinases and angiogenesis [10].
Diagnosis of our patient was confirmed in Multidisciplinary Team meeting (MDT) given the patient's history of hepatitis C, Cirrhosis, radiological features highly suggestive of HCC and AFP levels above 50,000.0 IU/ML. We do not routinely perform biopsies to confirm the diagnosis of HCC as recommended by the major international guidelines.
Our patient developed spontaneous regression of large HCC soon after exploratory laparotomy with complete resolution of the previously seen partial portal vein thrombosis and the paracardiac Lymph Nodes. There is Significant clinical, biochemical and radiological improvement. No attempt at embolization of the tumor was made during the surgery. There was no evidence of infection or any inflammatory process. He has not received any active oncological intervention or treatment during this period. However, he dose report significant changes in his dietary habits with more focus on fresh fruits and vegetables.
Tumor ischemia, systemic inflammatory response and immune mediated regression are reported as possible etiology. Although no etiology is obvious in spontaneous regression of this very large HCC in our patient, immune mediated regression is plausible. We plan to monitor the patient very closely with monthly clinical assessment and radiological surveillance. He has declined any oncological or surgical intervention till date.
Funding: this is a case report did not have any source of fund.
References
- https://gco.iarc.fr/today/data/factsheets/cancers/11-Liver-fact-sheet.pdf
- Chien RN, Chen TJ, Liaw YF. Spontaneous regression of hepatocellular carcinoma. Am J Gastroenterol, 1992; 87: 903–905.
- Sakamaki A, Kamimura K, Abe S, Tsuchiya A, Takamura M, Kawai H, et al. Spontaneous regression of hepatocellular carcinoma: A mini-review. World J Gastroenterol, 2017; 23(21): 3797-3804. doi: 10.3748/wjg.v23.i21.3797.
- Janevska D, Chaloska-Ivanova V, Janevski V. Hepatocellular Carcinoma: Risk Factors, Diagnosis and Treatment. Open Access Maced J Med Sci, 2015; 3(4): 732-736. doi: 10.3889/oamjms.2015.111.
- Everson TC, Cole WH. Spontaneous regression of cancer: preliminary report. Ann Surg, 1956; 144: 366–380.
- Dawson WR, Ebbell B. The papyrus ebers; the greatest egyptian medical document, J. Egypt Archaeol, 1938; 24(1): 250–251.
- Johnson FL, Lerner KG, Siegel M, Feagler JR, Majerus PW, Hartmann JR, et al. Association of androgenic-anabolic steroid therapy with development of hepatocellular carcinoma. Lancet, 1972; 2: 1273–1276.
- Huz JI, Melis M, Sarpel U. Spontaneous regression of hepatocellular carcinoma is most often associated with tumor hypoxia or a systemic inflammatory response. HPB (Oxford), 2012.
- Abiru S, Kato Y, Hamasaki K, Nakao K, Nakata K, et al. Spontaneous regression of hepatocellular carcinoma associated with elevated levels of interleukin 18. Am J Gastroenterol, 2002; 97: 774-775.
- Ricci SB, Cerchiari U. Spontaneous regression of malignant tumors: Importance of the immune system and other factors (Review). Oncol Lett, 2010; 1(6): 941-945. doi: 10.3892/ol.2010.176. Epub 2010 Sep 23. PMID: 22870091; PMCID: PMC3412538. Aug;14(8): 500-5 doi: 10.1111/j.1477-2574.2012.00478.x. Epub 2012 May 15. PMID: 22762397; PMCID: PMC3406346.

