The Utilization of Single Photon Emission Computed Tomography/Computed Tomography (SPECT/Ct) for Detecting Early-Phase Diffuse Idiopathic Skeletal Hyperostosis
Danielle Anne G Tee1, Tsan-Yu Huang1, Chia-Ying Lai2 and Shin-Tsu Chang2,3,*
1Department of Medicine, National Defense Medical Center, Taipei, Taiwan
2Department of Physical Medicine and Rehabilitation, School of Medicine, Tri-Service General Hospital, National Defense Medical Center, Taipei, Taiwan
3Department of Physical Medicine and Rehabilitation, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
Received Date: 12/03/2023; Published Date: 24/05/2023
*Corresponding author: Dr. Shin-Tsu Chang, MD, MS, PhD, Department of Physical Medicine and Rehabilitation, Kaohsiung Veterans General Hospital, Department of Physical Medicine and Rehabilitation, School of Medicine, Tri-Service General Hospital National Defense Medical Center, Taiwan
Abstract
Diffuse Idiopathic Skeletal Hyperostosis (DISH), also called Forestier disease, is a noninflammatory, systemic, rheumatologic condition of unknown etiology, characterized by the formation of osteophytes in the spinal entheses. Because DISH tends to be asymptomatic, it is usually diagnosed during middle to late adulthood, making DISH among early adulthood extremely rare. Diagnosis of DISH is typically evaluated through plain radiography and/or CT scan. We report a 24-year-old man who presented with back pain over two years and was confirmed to have early-phase DISH through the use of SPECT/CT imaging. We discuss the symptoms, radiological features in conjunction with review of literature. To date, this is the first reported case of DISH below the typical age of onset of 40-50 years old diagnosed through SPECT/CT.
Keywords: Diffuse idiopathic skeletal hyperostosis; Forestier disease; Single photon emission computed tomography/computed tomography
Introduction
Diffuse Idiopathic Skeletal Hyperostosis (DISH) has known as a non-inflammatory and systemic situation, exemplified by abnormal calcification of the spinal entheses and ligaments [1]. It often remains undetected as patients may not experience any symptoms in the early stages until it progresses to later stages, most commonly causing stiffness, pain, and restricted range of motion in the neck or back [2]. The prevalence of DISH was reported to be higher in male populations and in patients over 50 years old, while it is extremely rare for individuals under the age of 40 to have the said condition [3]. Until the present, consensus in the medical field regarding the diagnostic criteria of the disease has not yet been achieved.
Radiographic evaluation is necessary to confirm diagnosis of DISH [4]. However, the common disadvantage among these imaging techniques (e.g., plain radiography [X-ray], computed tomography [CT] scan, or magnetic resonance imaging [MRI]) is their inability to simultaneously track both the morphological and physiological changes in the spine [5].
To date, we only found one study that discussed the use of SPECT/CT for diagnosing DISH in a 62-year-old male [6]. Moreover, we only found one case of DISH in a patient belonging to the 20–29-year age group [7] and the other the 30–39-year age group [3]. Our case features an extremely rare case of early-stage thoracic DISH in a 24-year-old male, an age that is far below the expected age of onset for DISH symptoms. This case highlights the utilization of SPECT/CT as a primary tool for detecting early signs of the condition.
Case Report
- Patient Description
Patient is a 24-year-old male who came to our outpatient department for a consultation regarding upper and lower back pain. The onset of his symptoms occurred two to three years ago (i.e., 2019 to 2020). However, due to schedule conflicts, the patient was not able to seek medical advice immediately until he experienced a sudden sharp pain on his back last September 14, 2022 after joining the military. His back pain was frequently triggered when participating in high-impact activities such as lifting heavy objects, jogging, and playing basketball intensely. He also experienced pain when sitting without support, which forced him to place a back support (e.g., pillow) or lean on the chair to ease the pain. Aside from receiving a formal diagnosis of scoliosis at another hospital previously, no other physical conditions were reported.
- Examination
Physical examination confirmed local tenderness in the upper and lower back region. X-ray imaging revealed typical spinal structures except for possible lesions in the thoracic spine (i.e., T5) (Figure 1). Based on the patient’s SPECT/CT results (Figures 2A-2D), we identified formation of a complete bone bridge along three or more segments in the patient’s thoracic vertebrae, preserved intervertebral disc space without disc or vertebral degeneration, and the absence of apophyseal joint ankylosis and sacroiliac joint erosion. Increased heterogeneous uptake of radiotracers along the anterior segment of the thoracic vertebrae indicate flowing ossifications, confirming our diagnosis of early-phase DISH, which may have been causing the patient’s back pain.
- Treatment and Follow-up
The patient was prescribed Befon/Baclafan and Lefenine/Flurbiprofen as muscle relaxants.
Discussion
DISH is considered as one of the most common etiologies of atypical bony formations (i.e., osteophytes; [8]). Based on Kim and colleagues (2018) [9], the presence of spinal calcifications was most commonly found in the middle part of thoracic spine (90.0%) and the lower part of thoracic spine (87.5%), followed by the cervical spine (43%). Most common symptoms of DISH include back pain, neck and/or back stiffness, and decreased range of spinal motion, but it may also result in more severe complications such as dysphagia, airway obstruction, and hoarseness, and vulnerability to spinal fractures [1]. Quintero-Gonzalez, Arbelaez-Cortez, and Rueda (2019) [10] stated that symptoms of DISH are typically based on the localization of the calcifications with spinal changes (e.g., axial pain, reduced axial range of motion, nerve root symptoms) being the most common manifestations related to the disease.
While the cause and pathogenesis of the disease are still poorly understood, researchers from different parts of the world had attempted to describe the prevalence of DISH in relation to various factors such as age, gender, and presence of metabolic diseases. In Italy, the prevalence of DISH among 1012 individuals was found to be 12.8% with the male participants having a higher preponderance (16.8%) than the female (10.3%). Additionally, the researchers found a significant relationship between DISH and age, BMI, and/or the presence of chronic diseases such as metabolic syndrome (Ciaffi et al, 2022). In another study conducted by Ahmed and colleagues (2022), the researchers found 19.1% of overall prevalence of DISH among 1815 participants, which increased with age. No participants among the 20-29 age group were diagnosed with DISH; the 30–39-year-old group showed the lowest DISH prevalence of 1.1%, while individuals aged 70-79 and older than 80 years old showed highest prevalence of the condition with 45.2% and 45.5% respectively (Ahmed et al, 2022). A cross-sectional study in Japan also reported similar results, particularly the presence of thoracic DISH after 40 years old and the highest preponderance of DISH in the thoracic vertebrae among the 70 years age group [11]. Therefore, the presence of DISH in the 20-29 and 30-39 age groups are extremely rare.
One of the most frequently adopted diagnostic criteria for DISH described by Resnick and Niwayma in 1976, is calcification and ossification along at least four adjacent vertebral bodies, the relative preservation of disc height accompanied with the lack of evidence for extensive radiographic changes of disc degeneration, and the absence of apophyseal joint bony ankylosis and sacroiliac joint erosion, sclerosis or intra articular bony fusion. The criteria was later modified (Table 1) to improve interobserver agreement for diagnosing DISH based on CT results [12]. The Reznickand Niwayma criteria has recently faced several challenges due to its limitations to more advanced and severe stages of DISH. Considering this, Kruper and colleagues (2019) [13] provided another set of criteria that is more suitable for confirming early-phase DISH, as follows: “a segment with a complete bone bridge with an adjacent segment of at least a near-complete bone bridge AND another adjacent segment with at least the presence of newly formed bone; OR when at least three adjacent segments were recorded as showing a near-complete bone bridge.)”
The most common imaging modality for confirming DISH at present is the use of plain radiography. Meanwhile, CT scan has recently been reported to possess higher sensitivity in detecting DISH and evaluating the structural changes associated with condition, while MRI is more sensitive in capturing the soft tissues of the spine, proving it to be a useful instrument in the differential diagnosis of DISH and Ankylosing Spondylitis (AS) since MRI is capable of detecting inflammation that is typical in AS [5,14,15]. Recently, bone scintigraphy with hybrid images of single photon emission computed tomography- computed tomography (SPECT-CT) has been introduced to provide accurate anatomical and functional imaging and precise localization of the spinal lesion by determining the location with increased radiotracer uptake [5]. To date, various researchers had attempted to explore the utilization of SPECT-CT in different rheumatologic and orthopedic lesions.
Kim and colleagues (2015) [16] studied the usefulness of bone SPECT/CT imaging in early axial spondyloarthritis as compared to conventional imaging techniques such as plain radiography and CT alone. The researchers found more advantages of using SPECT/CT because of its higher sensitivity (80.0%) and specificity (84.6%) in terms of detecting SIS ratio [16]. On the other hand, a report on the applications of SPECT/CT in musculoskeletal radiology also described the advantages of the said imaging technique with other tools (e.g., MRI, CT alone, SPECT alone) in evaluating both malignant and benign diseases in the axial skeleton. SPECT/CT was also beneficial in localizing chronic lower back pain for target-specific pain management by combining functional imaging with SPECT, which cannot be achieved by planar imaging or anatomical imaging alone [17,18]. Therefore, SPECT/CT proves to be a potential tool in achieving an accurate diagnosis for spinal lesions, cervical facet joint arthritis [19], sternoclavicular joint arthritis [20] and meniscus tear of knee joint [21]. Obtaining information on the functional changes before structural calcifications in DISH is important for early detection and intervention of DISH, preventing possible life-threatening complications. However, the impact and significance of SPECT/CT on DISH diagnosis across all age groups have not yet been studied at present.
Assogba and colleagues (2014) [7] described an extremely rare case of early-stage DISH in a 20-year-old male, which was the only study on DISH in the 20-29 years age group to date. Chitten and James (2019) [3] also presented a unique study of DISH, which involved a 33-year-old woman with polycystic ovarian syndrome (PCOS). Both reports merely used plain radiography and/or CT scan and MRI to confirm DISH, while the use of SPECT/CT was not mentioned. Morales, Ornilla, Sancho, and Guillen (2019) published a case that primarily focused on SPECT/CT as the primary diagnostic tool of DISH, but the patient of their study belonged to the 60–69-year-old age group, which was one of the populations with highest DISH prevalence.
Therefore, our case is the first to report an extremely rare case of a patient with DISH, whose symptoms began at 21-22 years old, which was far below the typical age of onset of the disease (i.e., 45-40 years old; the patient is currently 24 years old), and was primarily diagnosed through the use of SPECT-CT. Our study provides an interesting perspective on using SPECT-CT as a potential primary diagnostic tool for early-phrase DISH. Studies from Japan, Taiwan, and Netherlands showed a significantly higher incidence of cerebral infarction with a 55-68% increased rate of ischemic stroke (22-24). We also suggest that the onset of DISH may have started several years before symptoms become apparent and more severe. Hence, further research in exploring SPECT-CT to diagnose early signs of DISH or other spinal pathologies is strongly recommended.

Figure 1: Radiograph of the thoracic spine showing possible lesion in T5.
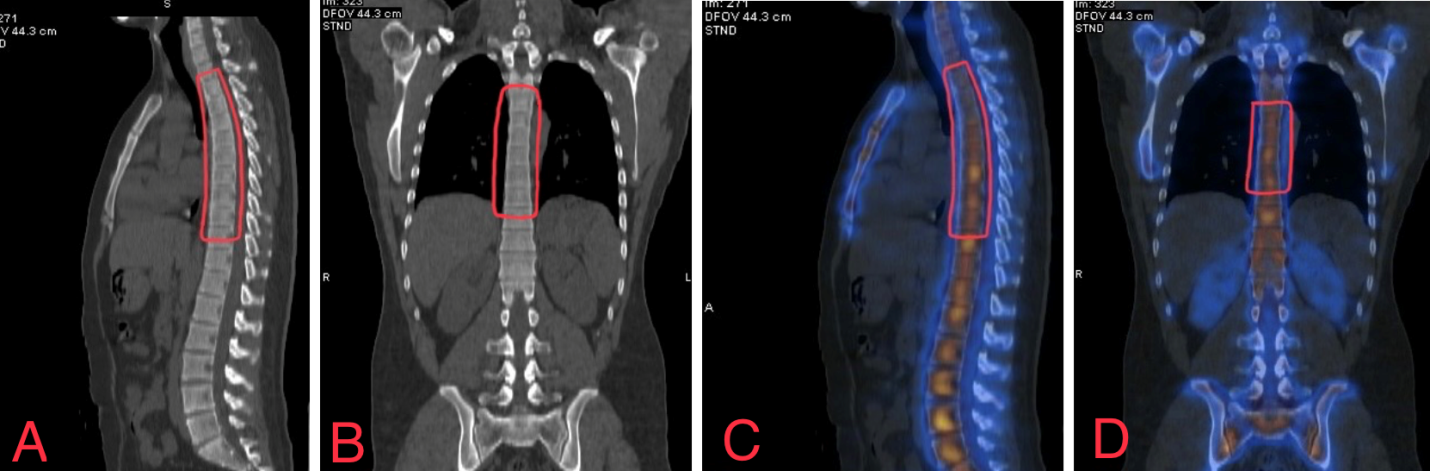
Figure 2: A case of DISH that involved continuous bone bridging in the thoracic spine (T2-9) taken through SPECT/CT in sagittal view (A and C) and coronal view (B and D).
Declarations
Ethical approval and consent to participate: Not required for this case report.
Consent for publication: Not applicable.
Competing interests: The authors declare that the case report was written in the absence of any potential conflicts of interest.
Funding: No specific funding was received by this study.
Acknowledgments: The authors would like to express our heartfelt gratitude to Dr. Chia-Ying Lai for providing copies of the radiographs and imaging results.
References
- Luo TD, Varacallo M. Diffuse Idiopathic Skeletal Hyperostosis. In StatPearls. StatPearls Publishing, 2022.
- Nascimento FA, Gatto LA, Lages RO, Neto HM, Demartini Z, Koppe GL. Diffuse idiopathic skeletal hyperostosis: A review. Surgical Neurology International, 2014; 5(Suppl 3): S122–S125. https://doi.org/10.4103/2152-7806.130675
- Chitten JJ, James B. Diffuse idiopathic skeletal hyperostosis in a 33-year-old woman with PCOS and metabolic syndrome: a rare scenario. BMJ Case Reports, 2019; 12(10): e223740. https://doi.org/10.1136/bcr-2017-223740
- Cammisa M, De Serio A, Guglielmi G. Diffuse idiopathic skeletal hyperostosis. European Journal of Radiology, 1998; 27(1): S7–S11. https://doi.org/10.1016/s0720-048x(98)00036-9
- Kim GU, Chang MC, Kim TU, Lee GW. Diagnostic modality in spine disease: A review. Asian Spine Journal, 2020; 14(6): 910–920. https://doi.org/10.31616/asj.2020.0593
- Lozano MI, Ornilla E, Sancho L, Guillén EF. Single-photon emission computed tomography in the diagnosis of a case of Forestier's disease. Reumatologia Clinica, 2019; 15(5): 307–308. https://doi.org/10.1016/j.reuma.2017.03.014
- Assogba K, Apetsè KM, Kombaté D, Oniankitan I, Balogou KA A. Forestier’s Disease in a young student: A genetic origin? Journal of Neurology and Epidemiology, 2014; 2(2): 76-78. https://doi.org/10.12974/2309- 2014.02.02.4
- De Jesus-Monge WE, Cruz-Cuevas EI. Dysphagia and lung aspiration secondary to anterior cervical osteophytes: a case report and review of the literature. Ethnicity & Disease, 2008; 18(2 Suppl 2): S2–140.
- Kim BS, Moon MS, Yoon MG, Kim ST, Kim SJ, Kim MS, et al. Prevalence of Diffuse Idiopathic Skeletal Hyperostosis Diagnosed by whole spine computed tomography: A preliminary study. Clinics in Orthopedic Surgery, 2018; 10(1): 41–46. https://doi.org/10.4055/cios.2018.10
- Diana C Quintero-González, Álvaro Arbeláez-Cortés, Jorge M Rueda. Clinical and radiological characteristics of diffuse idiopathic skeletal hyperostosis in two medical centers in Cali, Colombia: Report of 24 cases. Revista Colombiana de Reumatología (English Edition), 2020; 27(2): 80-87. https://doi.org/10.1016/j.rcreue.2020.01.005.
- Mori K, Kasahara T, Mimura T, Nishizawa K, Nakamura A, Imai S. Prevalence of thoracic diffuse idiopathic skeletal hyperostosis (DISH) in Japanese: Results of chest CT-based cross-sectional study. Journal of Orthopaedic Science: official journal of the Japanese Orthopaedic Association, 2017; 22(1): 38–42. https://doi.org/10.1016/j.jos.2016.09 .003
- Kuperus JS, Oudkerk SF, Foppen W, Mohamed Hoesein FA, Gielis WP, Waalwijk J, et al. Criteria for early-phase diffuse idiopathic skeletal hyperostosis: Development and validation. Radiology, 2019; 291(2): 420–426. https://doi.org/10.1148/radiol.2019181695
- Oudkerk SF, de Jong PA, Attrach M, et al. Diagnosis of diffuse idiopathic skeletal hyperostosis with chest computed tomography: inter-observer agreement. Eur Radiol, 2017; 27: 188–194. https://doi.org/10.1007/s00330-016-4355-x
- Mader R, Verlaan JJ, Eshed I, Bruges-Armas J, Puttini PS, Atzeni F, et al. Diffuse idiopathic skeletal hyperostosis (DISH): where we are now and where to go next. RMD open, 2017; 3(1), e000472. https://doi.org/10.1136/rmdopen-2017-000472.
- Slonimsky E, Leibushor N, Aharoni D, Lidar M, Eshed I. Pelvic enthesopathy on CT is significantly more prevalent in patients with diffuse idiopathic skeletal hyperostosis (DISH) compared with matched control patients. Clinical Rheumatology, 2016; 35(7): 1823–1827. https://doi.org/10.1007/s10067-015-3151-3
- Kim YI, Suh M, Kim YK, Lee HY, Shin K. The usefulness of bone SPECT/CT imaging with volume of interest analysis in early axial spondyloarthritis. BMC Musculoskeletal Disorders, 2015; 16(1): 9. https://doi.org/10.1186/s12891-015-0465-x
- Lee I, Budiawan H, Moon JY, Cheon GJ, Kim YC, Paeng JC, et al. The value of SPECT/CT in localizing pain site and prediction of treatment response in patients with chronic low back pain. Journal of Korean medical science, 2014; 29(12): 1711–1716. https://doi.org/10.3346/jkms.2014.29.12.1711
- Saha S, Burke C, Desai A, Vijayanathan S, Gnanasegaran G. SPECT-CT: applications in musculoskeletal radiology. The British journal of radiology, 2013; 86(1031), 20120519. https://doi.org/10.1259/bjr.20120519
- Chang ST, Liu CC, Yang WH. Single-photon emission computed tomography/computed tomography (hybrid imaging) in the diagnosis of unilateral facet joint arthritis after internal fixation for atlas fracture. HSOA Journal of Medicine: Study & Research, 2019; 2: 010.
- Chang ST, Tsai WY. Abrupt swollen bump of the shoulder girdle joint as the first presentation of flare-up in a case of axial spondyloarthritis. Canadian Journal of Biomedical Research and Technology, 2020; 3(5): 1-5.
- Su CL, Tsai YL, Cheng YY, Chang ST. Meniscus tear presented as bone marrow edema manifested in hybrid images in skeletal scintigraphy: a case report. Archives of Rheumatology & Arthritis Research, 2021;1(3):2021. ARAR.MS.ID.000513. DOI: 10.33552/ARAR.2021.01.000513.
- Miyazawa N, Akiyama I. Diffuse idiopathic skeletal hyperostosis associate with risk factors for stroke: a case-control study. Spine (Phila Pa 1976), 2006;31(8):E225-9; discussion E230. doi: 10.1097/01.brs.0000214949.75361.f4.
- Cheng YY, Lin CH, Tsai PY, Chen YH, Lin SY, Chang ST. Increased risk of stroke in patients with diffuse idiopathic skeletal hyperostosis: a nationwide population-based cohort study. Sci Rep, 2021;11(1):21349. doi: 10.1038/s41598-021-00798-2.
- Harlianto NI, Oosterhof N, Foppen W, Hol ME, Wittenberg R, van der Veen PH, et al. UCC-SMART-Studygroup. Diffuse idiopathic skeletal hyperostosis is associated with incident stroke in patients with increased cardiovascular risk. Rheumatology (Oxford), 2022; 61(7): 2867-2874.doi: 10.1093/rheumatology/keab835.

