Lung cancer in a young patient with HIV
Claribel Plain Pazos1,*, Anel Pérez de Alejo Alemán2, Damila Valladares Pérez3, Naidy Rojo Quintero4, Brian Raciel Hernéndez Pérez5, Carmen Rosa Carmona Pentón1 and Nubia Blanco Balbeito6
1Specialist of I and II Degree in Comprehensive General Medicine, Assistant Professor, Faculty of Medical Sciences of Sagua la Grande, Cuba
2Department of Internal Medicine. Provincial General University Hospital “Mártires del 9 de abril”, Sagua la Grande, Villa Clara, Cuba
3Specialist in Imaging. Clinical Surgical Teaching Hospital "Abel Santamaría Cuadrado". Pinar del Rio, Cuba
4Department of Pathological Anatomy. Assistant Professor, University Hospital “Manuel Ascunce Domenech”, Camagüey, Cuba
53rd Year Student of Medicine, Faculty of Medical Sciences of Sagua la Grande. Villa Clara, Cuba
6Department of Pedagogical Sciences, Faculty of Medical Sciences of Sagua la Grande, Villa Clara, Cuba
Received Date: 28/02/2023; Published Date: 17/05/2023
*Corresponding author: Claribel Plain Pazos, Specialist of I and II Degree in Comprehensive General Medicine, Assistant Professor, Faculty of Medical Sciences of Sagua la Grande, Cuba
Abstract
Pulmonary infections and neoplasms are the most common chest manifestations in patients infected with the human immunodeficiency virus. A case of a young patient with a history of being a smoker and drug addict is presented, who presented with a wet cough, yellowish sputum, hemoptysis, easy fatigue, loss of appetite and weight loss, who was referred with a possible diagnosis of tuberculosis but after admission. he was diagnosed with HIV and advanced lung cancer. The diagnosis was made by fine needle puncture after which he presented a hemothorax as a complication, which caused his death.
Keywords: lung cancer, tuberculosis, HIV
Introduction
Lung cancer is the most common malignant tumor worldwide, affecting more than 3 million people [1], it is the leading cause of cancer death [2], possibly because 70% of cases are diagnosed at an early stage. advanced, unresectable [1,3].
Some lifestyle habits such as alcohol consumption, tobacco use, physical inactivity and unhealthy eating; are major risk factors for cancer worldwide [3].
Every day 4,000 people become infected with HIV [4]. During the year 2020, it was estimated that there were 37.3 million people in the world living with this disease [5]. If current trends continue, 1.2 million people will become infected with HIV by 2025[4]. In 2021, 650,000 people died of AIDS-related causes, one every minute [3].
Lung infections and neoplasms are the most common chest manifestations in patients infected with the human immunodeficiency virus (HIV) [6]. Bacterial lung diseases are the leading cause of lung pathology in patients with HIV [7] and within neoplasms, Kaposi's sarcoma (SK) and Non-Hodgkin Lymphomas (NHL) are the most frequent lung neoplasms [6].
The clinical manifestations caused by lung cancer and pulmonary infections can be similar, so the diagnosis is based on the definitive result of the pathology, since although the tomographic findings can be highly suggestive of malignancy, there are reports of diseases they can be mimics, which can lead to inappropriate treatments and adverse events [2].
Such is the case that is presented below, which was a young man, referred for a possible pulmonary tuberculosis, who was diagnosed with lung cancer.
Case Presentation
A 42-year-old male patient with a history of being a smoker since he was 17 years old and of intravenous heroin use, who was referred to rule out pulmonary tuberculosis since for a month he has been presenting with a wet cough, with yellowish sputum, sometimes with blood streaks, easy tiredness, loss of appetite, loss of 10 kilograms of weight in that period, evening fever of 37.5°C and 38°C. On physical examination, mucosal skin pallor was observed, on respiratory auscultation, decreased vesicular murmur in the right hemithorax, with crackling rales in that hemithorax.
Complementary Exams:
HGB 9 g/dl
Leukogram: 11x109/l Gram 78% Lymph 34%
LDH 480 U/l
CPR 240 mg/l
Liver function: normal
Kidney function: normal
HIV: Positive
Spit for Tuberculosis: Negative
Torax X Ray: A relatively homogeneous mass observed in the upper lobe of the right lung causing the attraction of mediastinal structures, associated with a small amount oh right pleural effusion (Figure 1).

Figure 1: Torax X Ray: A relatively homogeneous mass in upper right lung.
MDCT scans were performed before and after intravenous contrast administration
Mass lesion is seen in the right lung, obliterating the right upper lobe bronchus. The lesion measures about 17 x 12 x 12 cm. The mass lesion extends to the mediastinum, causing encasement of the right pulmonary artery, and the right superior pulmonary vein. Patchy opacities in the right lung upper lobe, surrounding the tumors, may be due to pulmonary consolidation, or congestion due to lymphatic obstruction. Pleural effusion is seen in the right. The mediastinum is centered and of normal width. There are multiple mass lesions in the superior and middle mediastinum compatible with lymph nodes. The largest is in the subcarinal region, measuring about 25 mm, compatible with lymph nodes metastases. Lung bullae are seenat both sites. Poorly enhancing nodular lesions are seen in the left lobe of the liver, compatible with hepatic metastases. Bony structures appear normal. No evidence of bone metastases seen. Features suggestive of bronchogenic tumor in the right hemothorax, with associated pleural effusion, Mediastinal lymph nodal and hepatic metastases likely (Figure 2A-2F).

Figure 2(A;B;C;D;E;F): MDCT scans.
A puncture biopsy was decided to confirm the diagnosis. (Figure 3)
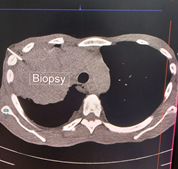
Figure 3: Puncture biopsy.
Puncture biopsy: Moderately differentiated squamous cell carcinoma.
Diagnosis: Lung cancer with lymph node and liver metastases.
HIV patient: Two days after the punch biopsy, the patient began with severe respiratory distress and collapsed in the hospital bathroom. A Pulmonary MD CT scan angiogram was performed and he was admitted to the Intensive Care Unit (IUC).
Pulmonary MD CT scan angiogram: No evidence of pulmonary embolism bilaterally. No pneumothorax is detected. Bilateral apical bullous emphysema. Right lower lobe pneumonic opacification probably due to alveolar oedema, intra pulmonary hemorrhage (?) As described Figure 4.
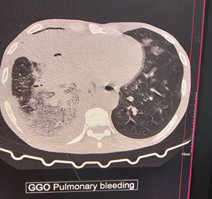
Figure 4: Pulmonary MD CT scan angiogram.
Two days later the patient died with pulmonary hemorrhage.
Discussion
Approximately 5 to 10% of patients with HIV require hospitalization in an intensive care unit (ICU), of which approximately 40% are unaware that they are infected with this virus and it is estimated that 50% do not receive retroviral treatment. upon your admission [8]. The patient described above was unaware that he had HIV, never received retroviral treatment and while hospitalized his symptoms worsened requiring admission to the ICU.
Bacterial pneumonia, especially that caused by pneumococcus, followed by pneumonia by Pneumocystis jiroveci and tuberculosis, is the most frequent cause of admission to health facilities in patients with HIV, with a higher incidence in the young male population [9]. In pulmonary tuberculosis, symptoms such as cough and expectoration are described, which can be accompanied by mild hemoptysis [10], in lung cancer, persistent cough, chest pain, hemoptysis, dyspnea, rhonchi are also described as the most common symptoms. and wheezing, fatigue and dysphonia [11]. In this case, the patient was diagnosed with lung cancer, a pathology that is not very common in a young patient, who was initially mistaken for pulmonary tuberculosis, due to presenting symptoms compatible with this disease, such as wet cough, hemoptysis, and weight loss, together with a history of drug addiction.
Although of varied etiology, smoking is recognized as the main cause of lung cancer, accounting for 90% of all cases [11]. This patient had a history of being a smoker since he was 17 years old, so he had been smoking for around 25 years, a factor that could have contributed to the development of his disease.
Lymphoma and Kaposi's sarcoma are the most frequent lung cancers in patients with HIV [6], however, in this patient a moderately differentiated Squamous Cell Carcinoma was diagnosed, a pathology that is not very frequent in this type of patient.
Different modalities are available for the diagnosis of this disease: radiology, bronchoscopy, bronchial biopsy, sputum cytology, bronchial brushing, bronchial lavage, and fine needle aspiration cytology [12]. In this case, the positive diagnosis was made by fine needle biopsy.
Only 20% of cases have localized disease, 25% have it spread to regional lymph nodes, and 55% already suffer from distant metastases. Once diagnosed, they have a very poor prognosis, since only 15% of cases can be cured [13]. This patient came in an advanced stage of his disease, presenting lymph node and liver metastases. After the diagnosis was made, he suffered a hemorrhagic complication (hemothorax) that ended the patient's life.
Conclusion
Lung cancer is a diagnosis to be taken into account when faced with a patient with suggestive manifestations and a history of being a smoker, even if he is young. Although fine needle aspiration biopsy is one of the procedures indicated for the accurate diagnosis of the disease, the possibility of complications in advanced stages of the disease should be assessed, especially in patients with comorbidities.
References
- Salvador Montejano R, Sáenz de Navarrete Corella R, Barbero Tienda P, Abances Ibarra MT, Amores González AB. Plan de cuidados general para el postoperatorio de pacientes intervenidos de cáncer de pulmón. Revista Sanitaria de Investigación, 2023; 4(1): 30.
- Peinado Acevedo JS, Cáceres Galvis C, Cardona Palacio A, Arango Viana JC, Roldán Pérez M, Atencia Flórez C. Criptococosis diseminada en paciente inmunocompetente imitando un cáncer de pulmón metastásico. Medicina & Laboratorio, 2022; 26(1): 81-89.
- Galindo Ángel I. Análisis comparativo de la utilidad diagnóstica de marcadores relacionados con la placa desmosomal en biopsias de carcinomas de pulmón de células no pequeñas. Tesis doctoral. Universidad de Granada, 2023.
- Actualización mundial sobre el Sida, 2022.
- Pérez Araujo JI. Factores asociados a mortalidad en pacientes con infección por VIH en TARV, en el Hogar-Clínica “San Camilo”, 2012-2021. [Tesis de pregrado, Universidad Nacional Federico Villarreal],
- Esteban JJ, Marco JA, Fernández EV, Sánchez LC. Cancer de pulmon en pacientes con infeccion por el virus de la inmunodeficiencia humana (vih) y sindrome de inmunodeficiencia adquirida (sida). Neumosur: rev de la asociación de neumólogos del sur, 1998; 10(3): 48-50.
- Choinier P, Parrot A, Cadranel J. Anomalías respiratorias en la persona infectada por el virus de la inmunodeficiencia humana. EMC-Tratado de Medicina, 2023; 27(1): 1-7.
- Leon Alonso JK, Mendosa Moreira RD, Bajaila Aguilar GP, Soriano Panchana OR, Escobar Segovia KF. Morbilidad en pacientes infectados por VIH/SIDA en una Unidad de Cuidados Intensivos. Revista Científica y Tecnológica UPSE, 2022; 9(1): 18-24.
- Hidalgo Jaitia SL, Sánchez Ortiz DM, Gómez Martínez N. Cuidado enfermero en paciente portador de VIH con bronconeumonía Nursing care in HIV-positive patients with bronchopneumonia. Revista Arbitrada Interdisciplinaria de Ciencias de la Salud. SALUD Y VIDA, 2022; 6(1): 63-69.
- Hinojos Gallardo LC. 14 Tuberculosis. Enfermedades del aparato respiratorio, 249-263.
- Plain Pazos C, Pérez de Alejo Alemán A, González Hernández ID, Carmona Pentón CR, Pérez de Alejo Plain A. Treatment-Resistant Bronchopneumonia as a Form of Presentation of Lung Cancer: A Case Report. J Clin Case Stu 2020; 5(4): 1-5.
- Vera Agreda MMM. Índice de inmunidad-inflamación sistémica elevado como predictor de sobrevida quinquenal en pacientes con cáncer pulmonar. Tesis en internet, 2022.
- Plain Pazos C, Carmona Pentón CR, Pérez de Alejo Plain A, Caraballo Moya A, Jiménez Aguiar A. Lung cancer: prevent or treat? Biomedical Research and Clinical Reviews, 2021; 4(4): 1-2.

