Pregnancy-Associated Necrotizing Vulvar Edema: A Rare but Severe Complication
Gali Gordon1,, Ayal Hassidim2, Roie Alter1 and Doron Kabiri1
1Department of Obstetrics and Gynecology, Hadassah Medical Organization and Faculty of Medicine, Hebrew University of Jerusalem, Israel
2Department of Plastic and Aesthetic Surgery, Hadassah Medical Organization and Faculty of Medicine, Hebrew University of Jerusalem, Israel
Received Date: 26/02/2023; Published Date: 03/05/2023
*Corresponding author: Gali Gordon M.D., Department of Obstetrics and Gynecology, Hadassah Hebrew University Medical Center, Ein-Kerem, P.O. Box 12000, Zip code 9112001, Jerusalem, Israel
Abstract
Vulvar edema is a rare occurrence in pregnancy. When it appears, it is often associated with an underlying condition. Edema leading to tissue necrosis in pregnancy is an extremely uncommon complication and has yet to have been described in literature. This case presents a patient who suffered from vulvar edema and signs of necrosis with no identifiable cause other than the compression of the Inferior Vena Cava shown on Computed Tomography scans. The patient did not respond to conservative management, therefore, a Cesarean Section at 33 weeks’ gestation was inevitably performed, thus emphasizing the severity of such complication.
Abbreviations: Computed tomography -CT; Inferior Vena Cava- IVC; Deep vein thrombosis -DVT
Introduction
Pregnancy is a physiological state that is accompanied by several physiological changes in a woman's body, including an increase in blood volume, cardiac output, and changes in the vascular system. These changes can sometimes lead to various complications, including edema. Edema, or the accumulation of fluid in the body's tissues, is a common occurrence during pregnancy, particularly in the lower limbs. However, edema can also occur in other parts of the body, including the vulva. Vulvar edema is a rare but potentially serious complication that can occur during pregnancy and is characterized by the accumulation of fluid in the tissues of the vulva at the external female genitalia. Vulvar edema is of concern during pregnancy since it may be accompanied by serious discomfort, as well as interfere with vaginal birth and may result in increased blood loss or poor wound healing. In extreme cases, it may even lead to necrosis of the affected region.
The etiology of vulvar edema during pregnancy is not well understood. It has been suggested that it may be due to increased blood flow to the pelvic region, increased venous pressure, or hormonal changes. Vulvar edema has also been associated with various medical conditions, such as preeclampsia, significant proteinuria followed by hypoalbuminemia, diabetes, infection, trauma, neoplasms or multiple gestations [1-4]. It has also been reported to be caused by tocolytic therapy [5]. Obstruction of the Inferior Vena Cava (IVC) has been reported due to extrinsic pressure mostly attributed to neoplasms, thrombotic events or tumor invasion. To date no cases of symptomatic chronic IVC obstruction solely by pregnancy without any additional underlying cause have been described to cause such severe edema leading to necrosis.
We present a 27-year-old patient who developed massive vulvar edema leading to necrosis during her second pregnancy at the third trimester. This case illustrates the importance of timely diagnosis and management of vulvar edema in pregnancy to prevent serious complications. It also highlights the need for further research to better understand the etiology and risk factors for vulvar edema during pregnancy.
Case Description
A 27-year-old patient, 32+2 weeks of gestation in her second pregnancy, presented with worsening vulvar edema. Physical exam was unremarkable apart from significant bilateral pitting edema of the lower limbs and massive vulvar edema. Laboratory findings, including complete blood count, electrolytes, kidney function tests, and liver function tests, were within the normal range. Urine protein-creatinine ratio was slightly elevated yet blood albumin levels were normal, as were thyroid function tests.
A Computed Tomography (CT) scan was performed to evaluate the cause of the patient's symptoms. The CT scan demonstrated significant compression of the Inferior Vena Cava (IVC), causing critical stricture and near obliteration of the IVC (Figure 1). Extensive further investigation, including Doppler ultrasound and venography, revealed no other possible causes for the condition.
The patient was treated conservatively with bed rest, leg elevation, and compression stockings, as well as furosemide and Deep Vein Thrombosis (DVT) prophylaxis. However, no significant improvement was noted, and at 33+2 weeks of gestation, signs of necrosis appeared on the right labia (Figure 2A). A cesarean delivery was performed, after which an almost immediate resolution was noted (Figure 2B). The newborn was healthy and had no complications.
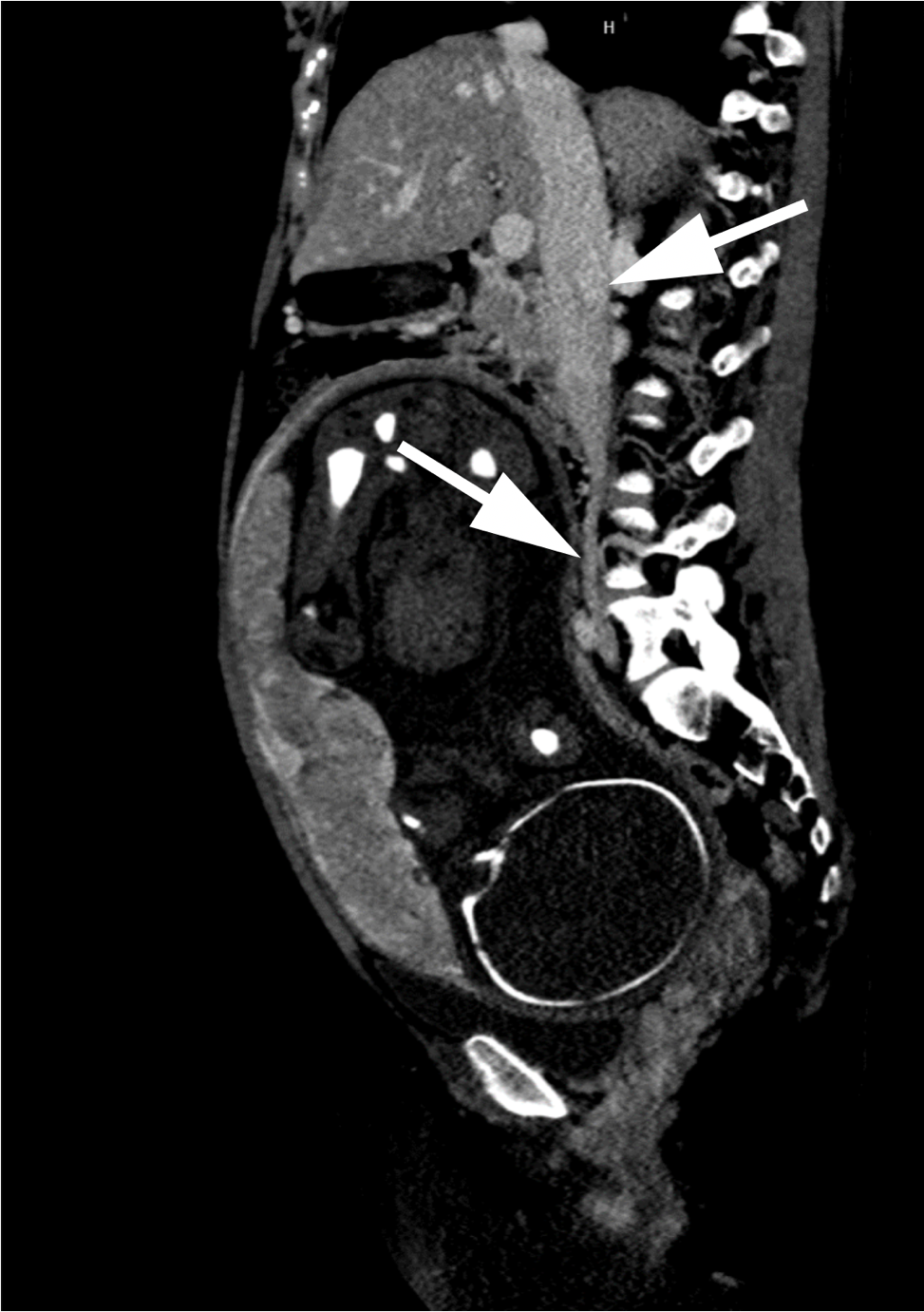
Figure 1: Abdominal computed tomography scan with IV contrast demonstrating significant compression of the Inferior Vena Cava; Upper arrow – normal vena cava, lower arrow – compressed vena cava.
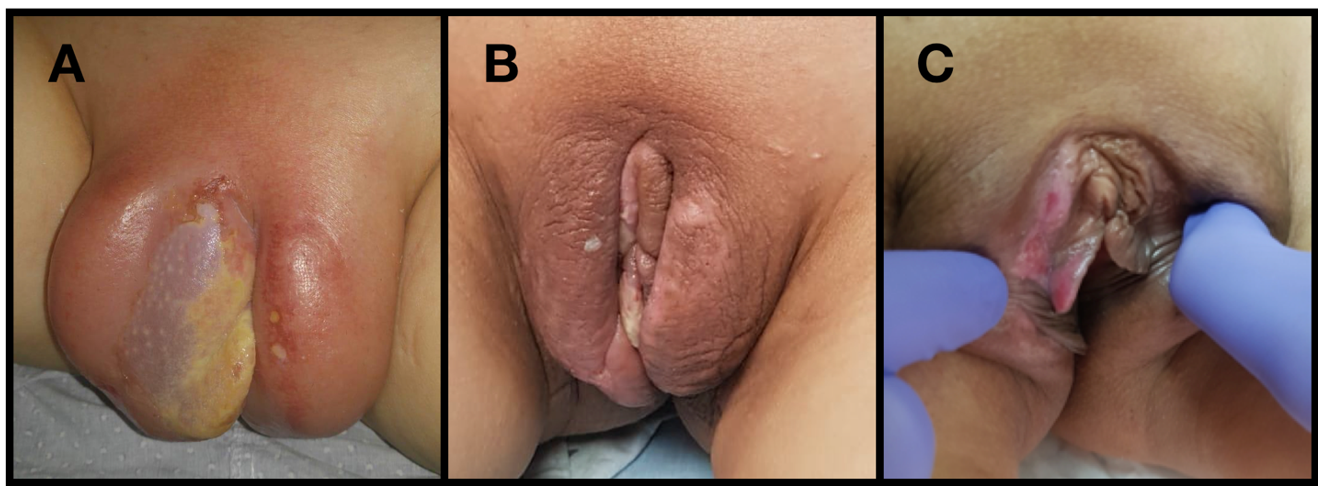
Figure 2: Figure 2: patient’s vulva with extensive edema and initial signs of necrosis on the right labia, prior to delivery (A); patient’s vulva four days (B) and six weeks (C) after cesarean delivery, presenting a significant improvement in vulvar edema.
Further Considerations
The management of vulvar edema during pregnancy requires consideration of several factors:
Underlying medical conditions: It is important to consider the potential underlying medical conditions that may be contributing to the vulvar edema, such as venous insufficiency, DVT, or preeclampsia, as mentioned above. In this case, no underlying medical conditions were identified as contributing factors
Diagnosis and evaluation: It is important to promptly diagnose and evaluate the cause of the vulvar edema. In this case, a Computed Tomography (CT) scan demonstrated significant compression of the Inferior Vena Cava (IVC), which was presumed to be the only cause of the patient's symptoms. Other imaging modalities, such as Doppler ultrasound and venography, can also be useful in evaluating the underlying cause of the vulvar edema.
Gestational age: The gestational age of the patient should be considered when managing vulvar edema during pregnancy in order to treat maternal discomfort whilst avoiding complications of prematurity. In this case, the patient was at 33+2 weeks of gestation and had already presented signs of necrosis on the right labia. A cesarean delivery was performed to minimize the risk of further complications for both the mother and the baby.
Treatment options: The potential impact of treatment on the mother and the baby should be carefully considered. Treatment should be directed at the cause of edema when an underlying cause is identified. Symptomatic relief includes bed rest trendelenburg positioning, and application of ice bags, hypertonic saline bags and local antibiotics. Heparin therapy may be considered as well since DVT may be the cause [6]. In case of no response to non-invasive methods, some authors suggest mechanical drainage as an alternative [2,7]. However, in this case, conservative measures were not effective, and a cesarean delivery was ultimately necessary. It is important to weigh the potential benefits and risks of different treatment options in order to ensure the best possible outcome for both the mother and the baby.
Conclusion
Vulvar edema is a rare complication that can occur during pregnancy and can lead to serious complications if not promptly diagnosed and managed. In this case, a patient developed vulvar edema and necrosis at 32+2 weeks of gestation, which was found to be caused by significant compression of the Inferior Vena Cava on CT scan. Despite conservative treatment, no improvement was noted and a cesarean delivery was ultimately performed. This case emphasizes the importance of timely diagnosis and management of vulvar edema in pregnancy to prevent serious complications and the need for further research to better understand the etiology and risk factors for this condition.
The authors report no conflict of interest, including any financial, personal, or other relationships that might inappropriately influence the work.
References
- Abdullahi HM, Suleiman MM, Abdullahi MM. Huge vulvar edema in a primigravida with severe preeclampsia – Emergency caesarean section and spontaneous resorption: A case report. Niger J Basic Clin Sci, 2019; 16: 75-78.
- Deren O, Bildirici I, Al A. Massive vulvar edema complicating a diabetic pregnancy. Eur J Obstet Gynecol Reprod Biol, 2000; 93(2): 209-211.
- Massinde AN, Ngwalida N, Gumodoka B. Massive vulval oedema in multiple pregnancies at Bugando Medical Centre: case reports. Tanzan J Health Res, 2011; 13(2): 142-144.
- Jakobi P, Friedman M, Goldstein I, Zaidise I, Itskovitz-Eldor J. Massive vulvar edema in pregnancy. A case reports. J Reprod Med, 1995; 40(6): 479-481.
- Mulisya O, Mastaki M, Gertrude T, Tasi K, Mathe JK. Spontaneous Massive Vulvar Edema in Pregnancy: A Case Report. Case Rep Obstet Gynecol, 2018; 2018: 7651254.
- Guven ES, Guven S, Durukan T, Onderoglu L. Massive vulval oedema complicating pregnancy. J Obstet Gynaecol, 2005; 25(2): 216-218. doi: 10.1080/01443610500051080. PMID: 15814419.
- Radomański T, Sikorski R, Baszak E. Obrzek sromu w ciazy [Vulvar edema in pregnancy. Ginekol Pol, 1998; 69(12): 1067-1070. Polish. PMID: 10224778.

