Periarticular Injection vs Peripheral Nerve Blockade in Bilateral Total Hip Arthroplasty
Carolyn Sivco1,*, Dahlia Townsend2, Michael Leslie3 and Jinlei Li4
1Resident of Anesthesiology, Department of Anesthesiology, Yale School of Medicine, USA
2Assistant Professor, Mount Sinai West & Morningside Hospitals, USA
3Associate Professor and Vice Chair of Quality & Safety, Yale School of Medicine, Department of Orthopaedics & Rehabilitation, USA
4Associate Professor; Director of Regional Anesthesia at Yale New Haven Hospital; Program Director of Acute Pain Medicine Fellowship; Director of Anesthesia and Acute Pain Medicine Service, Yale School of Medicine, Department of Anesthesiology, USA
Received Date: 22/02/2023; Published Date: 20/04/2023
*Corresponding author: Carolyn Sivco, MD Resident of Anesthesiology, Yale School of Medicine, Department of Anesthesiology 20 York Street, New Haven, CT 06510, US
Abstract
Pain control after total hip arthroplasty is associated with patient satisfaction, early discharge, and improved surgical outcome. Two commonly utilized opioid-reducing analgesic modalities are Periarticular Injection (PAI) by surgeons and motor-sparing Peripheral Nerve Block (PNB) by anesthesiologists. We present a case contrasting PAI and PNB in a single patient undergoing bilateral total hip arthroplasty. For the left hip, the patient received preoperative transmuscular quadratus lumborum, femoral nerve, and lateral femoral cutaneous nerve blocks using a combination of low concentration local anesthetic and glucocorticoids. For the right hip, the patient received an intraoperative PAI with liposomal bupivacaine. The patient’s pain scores and recovery were evaluated for three months postoperatively. The patient’s pain scores on Postoperative Day (POD) 0-5 were consistently lower in the left hip than in the right hip. For this patient undergoing bilateral hip replacement, preoperative PNBs were superior to PAI for postoperative pain control.
Keywords: Hip arthroplasty; Pain management; Periarticular injection; Peripheral nerve blockade
Introduction
Current pain control modalities following total hip arthroplasty include systemic analgesia, neuraxial analgesia, Peripheral Nerve Blocks (PNBs), and Periarticular Injection (PAI) [1]. PNBs are of unique interest as they have the potential to improve not only immediate postoperative pain, but also long-term outcomes for patients, including lower risk of chronic post-surgical pain and improved function. In this case, we sought to determine if there was a difference in postoperative pain scores and recovery for a patient receiving PNB versus PAI.
Case Report
A 5’4” (1.626m), 69.4kg healthy male in his 50s presented for elective bilateral total hip arthroplasty due to advanced osteoarthritis. His preoperative worst pain scores were 7 out of 10 in the right hip and 8 out of 10 in the left hip. The patient’s preoperative and postoperative x-rays can be found in Figure 1.
On the day of surgery, the patient was consented for left-sided preoperative PNBs and right-sided intraoperative PAI with the understanding that we wanted to compare these two analgesic modalities for postoperative pain relief. The PNBs were performed under direct ultrasound guidance (SonoSite, X-Porte, C60) by the anesthesiologist. The patient was placed in the right lateral decubitus position. A transmuscular Quadratus Lumborum (QL) block was performed using a 20-gauge insulated, short-bevel nerve block needle with a total of 30mL of 0.2% ropivacaine, 40mg Methylprednisolone Acetate (MPA), and 5mg dexamethasone sodium phosphate (DEX).
The patient was turned supine, and both a femoral nerve block and lateral femoral cutaneous nerve (LFCN) block were performed using 10mL of 0.2% ropivacaine, 20mg MPA, and 2.5mg DEX in each block.
In the operating room, the patient received intravenous sedation and an L3-L4 combined spinal/epidural. A total of 3mL of 0.5% bupivacaine was administered intrathecally and a total of 13 mL of 0.25% bupivacaine was administered epidurally throughout the procedure. The procedure was performed bilaterally via the direct anterior approach on a Hana table (OSI, Medine, MN, USA). At the end of the procedure, the surgeon performed a PAI using liposomal bupivacaine mixed with 30 ml 0.5% plain bupivacaine on the right hip. The local injection was performed using a 20-gauge needle into the closed capsule of the hip joint, the reflected head of the rectus, the tensor fascia lata, and the subcutaneous tissues.
The patient was transferred to the Post-Anesthesia Care Unit (PACU) in stable condition and denied any pain. An epidural infusion of 0.1% bupivacaine at 8mL per hour was started. Ten hours postoperatively, the patient had increasing pain, which improved with 10mg oxycodone. On postoperative day (POD) 1, the patient reported right hip pain greater than left hip pain, controlled with scheduled acetaminophen (975mg orally every 6 hours), scheduled ketorolac (15mg intravenously every 6 hours), and 5-10mg oxycodone as needed (total 25mg). He had swelling to bilateral incision sites, right greater than left. Motor function of his bilateral lower extremities was intact except for reduced strength (4/5) with right hip flexion. Sensation to his bilateral lower extremities was intact except for numbness to the bilateral upper thighs. The epidural infusion was discontinued, and the catheter removed on POD 1. The patient was able to ambulate with physical therapy with minimal assistance.
On POD 2, the patient continued to have right hip pain greater than left hip pain. He reported residual numbness to the bilateral hips and buttocks, and was discharged home. The patient took 5mg oxycodone as a preventative measure rather than for ongoing pain. On POD 3, the patient continued to take oxycodone as a preventative measure, as well as acetaminophen (975mg three times a day) and meloxicam (15mg daily). On PODs 4-5, he reported bilateral swelling and minimal pain, right greater than left. He participated in daily home physical therapy.
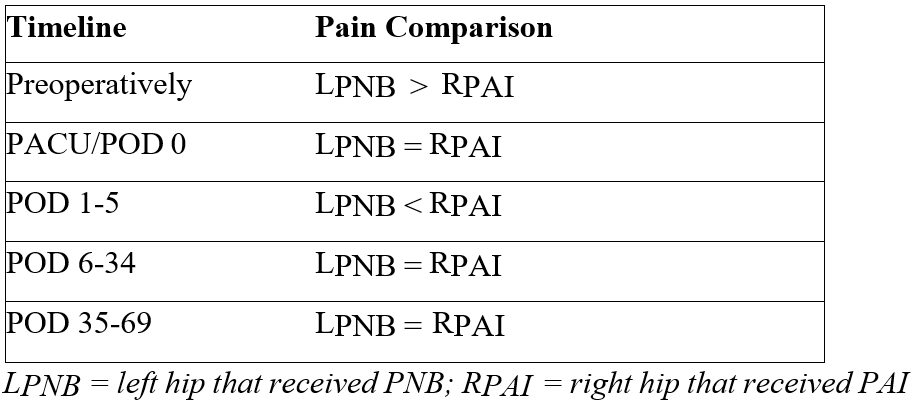
After POD 5, the patient denied pain at rest. The swelling to his left hip resolved on POD 13, while the swelling to his right hip resolved on POD 34. He transitioned to outpatient physical therapy on POD 20 and continued weekly physical therapy sessions until POD 69. By POD 51, the patient resumed his regular exercise routine. A summary of the patient’s daily postoperative pain scores, postoperative opioid consumption, and postoperative pain comparison between the left and right hips can be found in Tables 1 and 2.
Table 1: The patient’s average daily pain scores at rest and postoperative opioid consumption.

Table 2: The patient’s subjective pain comparison between the left and right hip over time.
Discussion
This case report is unique because, preoperatively, this patient’s bilateral hip pain and the morphology of his degenerative disease was both radiographically and clinically similar in duration and disability. This is often a confounding factor in comparing perioperative analgesia between patients with similar diagnoses but dissimilar severity. As a result, we were able to contrast two very common analgesia modalities for hip replacement surgery in a single patient.
Ultimately, the patient consistently reported better postoperative pain control on the left hip with PNB than on the right hip with PAI.
The transmuscular QL, femoral, and LFCN blocks were chosen for this patient for a variety of reasons. The transmuscular QL block has been shown to provide effective analgesia and reduce opioid consumption as compared to no PNB or PAI following THA [2]. In addition, it has been shown to result in fewer side effects such as lower extremity weakness [3]. The femoral nerve block can cause quadriceps weakness, but has also been shown to reduce time to first analgesic request, time spent in PACU, and overall opioid consumption during the first 24 hours postoperatively [4]. To minimize weakness and maximize pain control, we used low concentration local anesthetic.
The LFCN block is purely sensory with no risk of lower extremity weakness and a large coverage area extending from the knee to the posterolateral gluteal region [5]. The LFCN block can be helpful for postoperative pain management, though its efficacy when used alone in THA is controversial.4 We chose the combination of transmuscular QL, femoral, and LFCN blocks to minimize risk of lower extremity weakness and for the documented efficacy in dermatomal coverage for patient’s undergoing THA.
Single administration PNB or PAI without adjuvants seldom lasts beyond 24 hours, therefore, various local anesthetic adjuvants have been adopted by practitioners. DEX and MPA are commonly used to augment the block and prolong the duration of analgesia. MPA alone has been used extensively in chronic pain management and has demonstrated efficacy for long-term post- surgical pain control [6]. MPA has variable onset that may take up to 24 hours. DEX is water- soluble, has a faster onset than MPA, and prolongs the duration of local anesthetics for 6-8 hours [7]. For these reasons, DEX was utilized as a “bridge” between the local anesthetic and the longer-acting MPA in this case [8].
Conclusion
While the results for this patient favored PNB over PAI for THA, this data cannot be generalized to all patients. This patient’s increased swelling on the right hip may have contributed to an increased pain score. Additionally, different medications were used for the PNB and PAI, which may have contributed to varying pain scores. Ultimately, despite the patient’s increased pain and reduced range of motion in the right hip, he was able to participate well in physical therapy and reach full recovery bilaterally after only three months.
Persistent postsurgical pain after THA can affect anywhere from 7% to 23% of patient, significantly impacting patient satisfaction and daily life. The pre-existing pain, and the severity and duration of poorly controlled acute postoperative pain are identified as predictors of persistent post-surgical pain [9]. Despite the controversial roles of PAI and PNB in acute and chronic pain prevention, it is believed that aggressive and effective management of perioperative acute pain may minimize the transformation of acute pain to chronic pain [10]. It is our goal to develop a protocol for THA that not only targets acute pain, but also sub-acute pain after surgery, and subsequently impacts persistent post-surgical pain prevention.
Authorship:
RK, ML, and JL contributed to the initial planning, design, and implementation of the methods described in this case report. They each contributed to reporting data and to editing the final draft of the case report. CS contributed to the acquisition and interpretation of the data, drafting of the final report, and editing the report based on feedback from all listed authors.
Conflicts of Interest: The authors deny any conflicts of interest.
Grant Information: The authors received no specific funding for this work.
References
- Tyagi A, Salhotra R. Total hip arthroplasty and peripheral nerve blocks: Limited but salient role? Journal Anaesthesiology Clinical Pharmacology, 2018; 34(3): 379-380.
- Kukreja P, MacBeth L, Sturdivant A, et al. Anterior quadratus lumborum block analgesia for total hip arthroplasty: a randomized, controlled Regional Anesthesiology & Pain Medicine, 2019; 44: 1075-1079.
- Adhikary SD, Short AJ, El-Boghdadly K, et al. Transmuscular quadratus lumborum versus lumbar plexus block for total hip arthroplasty: A retrospective propensity score matched cohort Journal Anaesthesiology Clinical Pharmacology, 2018; 34(3): 372-378.
- Bugada D, Bellini V, Lorini LF, Mariano ER. Update on Selective Regional Anesthesia for Hip Surgery Anesthesiology Clinics, 2018; 36: 403-415.
- Vilhelmsen F, Nersesjan M, Andersen JH, et Lateral femoral cutaneous nerve block with different volumes of Ropivacaine: a randomized trial in healthy volunteers. BMC Anesthesiology, 2019; 19(1): 165.
- Richardson AB, Bala A, Wellman SS, et Perioperative Dexamethasone Administration Does Not Increase the Incidence of Postoperative Infection in Total Hip and Knee Arthroplasty: A Retrospective Analysis. The Journal of Arthroplasty, 2016; 31(8): 1784-1787.
- Kirkham KR, Jacot-Guillarmod A, Albrecht Optimal Dose of Perineural Dexamethasone to Prolong Analgesia After Brachial Plexus Blockade: A Systematic Review and Meta-analysis. Anesthesia & Analgesia, 2018; 126(1): 270-279.
- Li J, Perese F, Rubin LE, Carlyle D. Effective Pain Management After Total Hip Arthroplasty in a Sickle Cell Patient Emphasizing Dexamethasone Sodium Phosphate/Methylprednisolone Acetate Administered via a Peripheral Nerve Blockade: A Case A&A Practice. 2019; 12(5): 171-175.
- Richebe P, Capdevila X, Rivat Persistent Postsurgical Pain: Pathophysiology and Preventative Pharmacologic Considerations. Anesthesiology, 2018; 129(3): 590-607.
- Liu SS, Buvanendran A, Rathmell JP, et A cross-sectional survey on prevalence and risk factors for persistent postsurgical pain 1 year after total hip and knee replacement. Regional Anesthesiology & Pain Medicine, 2012; 37(4): 415-422.

