Cerebral Localization Without Neurological Repercussions: Interest of Imaging in Bourneville Tuberous Sclerosis
Imane Kacimi Alaoui*, Hanane Baybay, Zakia Douhi, Meryem Soughi, Sara Elloudi and Fatima Zahra Mernissi
Department of Dermatology, University Hospital Hassan II, Morocco
Received Date: 21/02/2023; Published Date: 19/04/2023
*Corresponding author: Dr. Imane Kacimi Alaoui, Department of Dermatology, University Hospital Hassan II, Fes, Morocco
Abstract
Bourneville Tuberous Sclerosis (BTS) involves abnormalities of the skin, brain, kidney, heart and lungs. Central nervous system tumors are the leading cause of morbidity and mortality; renal disease is the second leading cause of early death.
There are two observations of BTS, specifically their late revelation as well as their absence of intellectual consequences.
Keywords: Bourneville; Tuberous; Sclerosis
Introduction
Bourneville Tuberous Sclerosis (BTS) is a hereditary phacosmia with autosomal dominant inheritance, usually diagnosed in children and characterized by tumors of the skin, kidney and nervous system, the latter causing frequent epilepsy and mental retardation [1].
We report 2 observations of BTS, particular by their late revelation as well as by the absence of intellectual repercussions.
Case Report
Case 01
This is a 17-year-old patient with no previous pathological history who has presented for the past 7 years with raised lesions on the midface that are increasing in size.
The dermatological examination showed angiofibromas (Figure 1), a temporal patch of grief skin (Figure 2), hypopigmented macules on the back and buttocks.
The cerebro-thoraco-abdomino-pelvic CT scan showed a few calcified subependymal nodules, linear subcortical calcifications, and bilateral renal angiomyolipomas in the brain (Figure 3). The patient had never had an epileptic seizure.
Case 02
A 28-year-old female patient with no previous pathological history presented with a frontal nodule evolving for 5 years. Dermatological examination revealed a 4 cm left frontal pigmented tumor, facial angiofibromas (Figure 4) and café au lait spots.
The neurological examination was normal, with good psychomotor development.
Abdominal and pelvic ultrasound showed 5 renal angiomyolipomas bilaterally.
Brain MRI showed intraventricular subependymal nodules with no other localizations.

Figure 1: Multiple periocular and perioral angiofibromas.

Figure 2: Temporal patch of shagreen.
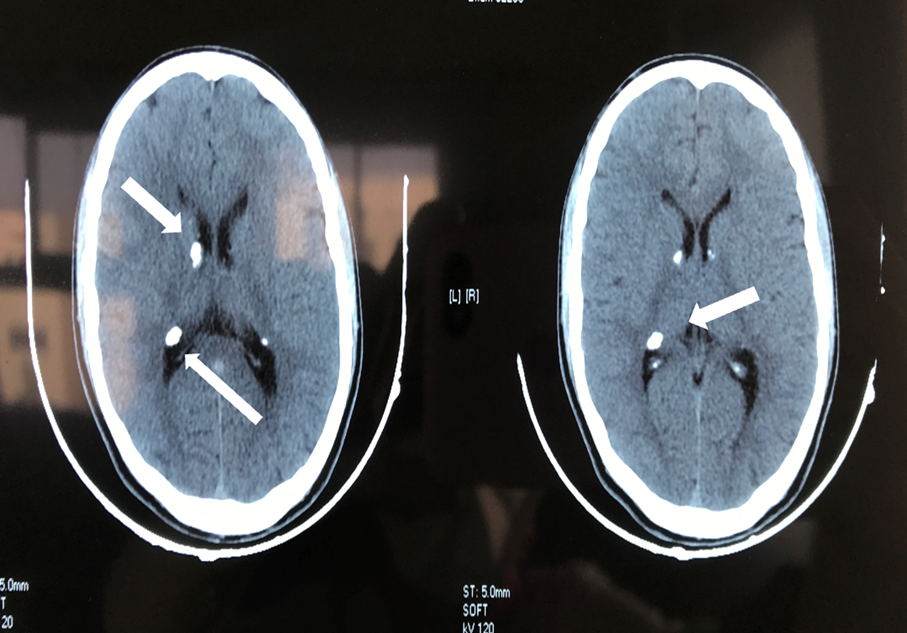
Figure 3: Brain CT scan without injection showing cortical tubers with calcified appearance (arrows).

Figure 4: Frontal pigmented tumor with angiofibromas.
Discussion
Bourneville tuberous sclerosis is an autosomal dominant genetic disorder with an incidence of approximately 1 in 10,000 live births [1].
classic picture related trio of mental retardation, epileptic seizures, skin symptoms. This definition is misleading as some subjects may have normal intellectual status [2].
Epilepsy may be the first clinical sign in 70-90% of cases and occurs at any age.
45-82% have mental retardation, mood disorders, attention disorders and obsessive-compulsive disorders [3].
The cerebral manifestations present are subependymal nodules, cortical nodules, and giant cell astrocytoma. The diagnosis of BTS remains clinical based on the combination of at least two hyperplastic sites in the retina, skin, brain, kidney, and heart. This should lead to evaluation of lesions consisting of brain imaging, renal and cardiac ultrasound.
MRI of the brain is recommended every 1-3 years to monitor the potential of a subependymal nodule to grow into a subependilemal tumor [2].
Conclusion
It is therefore important that patients with BTS benefit from a radiological and neuropsychological evaluation outside of the clinical signs of call, in order to better adapt their school and social integration.
Consent: The examination of the patient was conducted according to the Declaration of Helsinki principles.
Conflicts of interest: The authors do not declare any conflict of interest
References
- Northrup H, Koenig MK, Pearson DA, Au KS. Tuberous Sclerosis Complex. 1999 Jul 13. In: Adam MP, Everman DB, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A, editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2023. PMID: 20301399.
- Ciobanu AM, Lisievici MG, Coman TC, Ciurea J, Popa MC. Atypical Bourneville sclerosis without epilepsy and mental retardation: case report and literature review. Rom J Morphol Embryol, 2014; 55(2): 413-418.
- de Vries PJ, Whittemore VH, Leclezio L, Byars AW, Dunn D, Ess KC, et al. Tuberous sclerosis associated neuropsychiatric disorders (TAND) and the TAND Checklist.Pediatr Neurol, 2015; 52: 25–35.

