Concomitant Dislocations on The Same Side; Erecta Dislocation of the Shoulder and Hip Obturator Dislocation (Exceptional Association)
Rafaoui A*, Alshaikh A , Jadib I , Elkassimi C, Messoudi A , Rahmi M and Rafai M
Department of Orthopedic and Traumatological Surgery (Pavilion 32), CHU Ibn Rochd, Casablanca, Hassane II University of Casablanca, Faculty of Medicine and Pharmacy Casablanca
Received Date: 15/02/2023; Published Date: 12/04/2023
*Corresponding author: Abderrahim Rafaoui, Professor of Orthopedic and Trauma Surgery, Department of Orthopedic and Traumatological Surgery (Pavilion 32), CHU Ibn Rochd, Casablanca, Hassane II University of Casablanca, Faculty of Medicine and Pharmacy Casablanca, Morocco
Abstract
Obturator hip dislocation is a rare variety of regular hip dislocations. Shoulder erecta dislocation is also a rare condition. the association of these two entities is exceptional. We report an exceptional case of a 19-year-old patient who presented with concomitant dislocations; erecta of the left shoulder and obturator of the hip on the same side following an accident on the public highway, motorcyclist hit by car with point of impact at the level of the internal face of his right knee then he fell on his shoulder left in abduction. The patient presented to the emergency room with an attitude of irreducible abduction of the left shoulder and flexion, abduction, external rotation of the left lower limb. The vascular and nervous examination was normal. The X-ray confirmed the diagnosis of a dislocation erecta of the left shoulder associated with an obturator dislocation of the hip on the same side. Emergency reduction under general anesthesia and curarization within 4 hours was performed in the operating room for both dislocations. a restraint of the left upper limb by orthosis elbow to the body, for three weeks and A discharge of 45 days was prescribed. An early rehabilitation of the left shoulder and the left lower limb without support was started after 03 weeks of immobilization followed deferred support from the 45th post-traumatic day. The Follow-up after 16 months was noted without stiffness or pain in the shoulder and hip, and without radiological signs of osteonecrosis of the femoral head.
Keywords: Concomitant dislocations; Erecta; Obturator; Shoulder; Hip
Introduction
Traumatic anterior dislocation of the hip without fracture of the acetabulum or femoral head is rare [1]. They are often secondary to road traffic accidents, and erect dislocation is a rare form of shoulder dislocation with an estimated incidence of 0.5% of all such dislocations [2]. It is a functional emergency that requires an orthopaedic reduction in the first instance and as soon as possible. We report here an exceptional case of a 19-year-old patient who presented concomitant dislocations; an erecta dislocation of the left shoulder and an obturator dislocation of the hip on the same side, and the functional result after 16 months of follow-up.
Case Presentation
The patient was 19 years old and was the victim of a road traffic accident. He was hit by a car with an impact point on the inside of his right knee and then fell on his left shoulder in abduction, resulting in a closed trauma of the left hip and shoulder. The initial examination revealed total functional impotence of the left upper and lower limb, with a hip in flexion abduction external rotation and an upper limb in forced abduction and external rotation, arm in the air with an impossibility of bringing the elbow to the body (Figure 1).
The vascular and neural examination was without abnormality, as was the skin examination. A standard radiological work-up was carried out urgently, and the variety erecta was confirmed by a frontal X-ray of the left shoulder (Figure 2), which showed the subglenoid position of the humeral head and a humeral axis projected above the horizontal, and a frontal X-ray of the pelvis (Figure 3), which showed an obturator dislocation of the left hip. Emergency reduction under general anaesthesia and curarisation within 4 hours was performed in the operating theatre using the following manoeuvres: for the left shoulder; traction in the axis of the limb with slight abduction, for the left hip; initial traction in the axis of the limb followed by flexion of the hip in internal rotation and abduction while maintaining traction. X-rays of the left shoulder and pelvis (Figure 4) were satisfactory and a post-reduction CT scan of the pelvis (Figure 5) confirmed the reduction and the absence of associated injury and intra-articular fragment. Early rehabilitation of the left shoulder and the left lower limb without support was started after 03 weeks of immobilisation followed by deferred support from the 45th post-traumatic day. 16 months later, the Postel-Merle d'Aubigné functional score (PMA) was 18, with no stiffness or pain in the shoulder and hip, and no radiological signs of osteonecrosis of the femoral head.

Figure 1: Clinical picture showing the vicious attitude of the left upper limb in forced abduction and external rotation, and the left lower limb in flexion, abduction and external rotation.

Figure 2: Frontal X-ray of the left shoulder shows an erecta dislocation of the shoulder.

Figure 3: Frontal X-ray of the pelvis shows an obturator-type dislocation of the left hip.
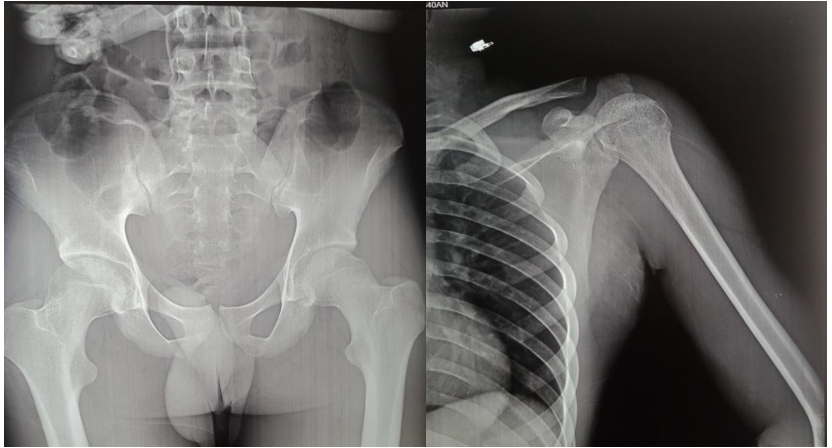
Figure 4: Control X-ray of the left shoulder from the front and pelvis from the front showing reduction of both dislocations.

Figure 5: Post-editing CT scan of the pelvis showing reduction of the femoral head without associated osteoarticular injury.
Discussion
Erecta dislocation is a rare form of shoulder dislocation [2], first described in 1895 by Middeldorpf and Scharm [3,4].
Davids and Talbott reported two mechanisms of erecta dislocation in 1990 [5]: a direct mechanism by the application of violent abduction forces to an initially abducting limb, with the acromion acting as a lever for the humeral axis; and an indirect mechanism following the application of heavy overload to a limb in full abduction. Road traffic accidents are the main etiology. The clinical study of erecta dislocation can be summarised by Stimson's definition [6]: "This remarkable dislocation is characterised by the marked elevation of the arm next to the head, from which position it is impossible to lower it without causing great pain. Physical examination reveals a humeral head palpated in the axillary fossa, the vacuity of the glenoid and changes in the muscular and bony relief.
A radiological assessment is necessary to confirm the dislocation and reveal any associated lesions. Standard radiographs of the face and a true axillary profile show the humeral head projected below the inferior pole of the glenoid and a humeral diaphysis always above the horizontal [7]. The evolution can be marked by different complications depending on the age of the patient [8]; thus, the most frequent complication before the age of 45 is the recurrence of the dislocation.
After the age of 45, a rotator cuff injury as well as a fracture of the major tubercle are possible.
Erecta dislocation occurred when the tear in the inferior glenohumeral ligament was longitudinal. For dislocation to occur experimentally, seven out of eight cases required deep rotator cuff disinsertion.
We did not note any vascular or nerve complications in our patient, although cases of damage to the axillary artery and brachial plexus have been observed due to the proximity of the glenohumeral joint to these two noble elements. In the series by Mallon et al [9], comprising 86 observations, damage to the axillary nerve was reported in 60% of cases and damage to the axillary artery in 3% of cases.
The treatment of uncomplicated erecta dislocations is orthopaedic [10].
According to Nho et al [11], the non-bloody reduction of this dislocation takes place in two steps, under minimal analgesia. The manoeuvre consists, according to these authors, in transforming the lower dislocation into an anterior dislocation, then reducing the head
The humerus is placed in the glenoid cavity. Thus, the operator places one hand on the shaft and the other hand on the medial condyle of the humerus. The hand on the shaft applies anterior force and rotation to the humeral head, bringing it back to an anterior position, and then the humerus is adducted and externally rotated, reducing the head into the glenoid cavity. This reduction is followed by elbow to body shoulder immobilisation for three weeks. Radiological control after reduction is always indicated. Rehabilitation is the only guarantee of satisfactory functional recovery [12]. The long-term prognosis is generally favourable.
Obturator dislocation accounts for 6 to 10% of dislocations reported in the literature [1]. The mechanism of occurrence of this entity is a movement in flexion, abduction and forced external rotation [13] with the cam effect of the greater trochanter on the ́ilion in maximum abduction. It is this mechanism that explains the dislocation in our case.
Anterior capsular injuries are constant [14]. These lesions can lead to irreducibility by a buttonhole effect [15]. Osteoarticular injuries are also very frequent and depend on the mechanism and violence of the initial trauma. Fractures of the femoral head occur in more than 50% of anterior dislocations [16].
Orthopaedic reduction is urgently required [17]. Reduction difficulties related to muscle mass, the risk of femoral head entrapment in the obturated foramen, and iatrogenic fracture of the neck have been reported [14]. This reduction must be performed under general anaesthesia with complete muscle relaxation.
Reduction manoeuvres differ between authors Epstein [18] and Brav [17] recommend traction in the ́axis of the femur followed by ́progressive flexion of the hip into internal rotation and abduction while maintaining traction.
Post-reduction CT should systematically look for a chondral lesion or an infra radiological fracture. An osteochondral fracture of the femoral head is frequently associated with this type of dislocation [18,19,20].
The risk of secondary avascular necrosis is increased by the delay in reduction; Hougaard [21] noted 52.9% necrosis when the reduction time exceeded 6 hours. Our reduction was completed within 4 hours without iatrogenic fracture, due to early diagnosis and atraumatic reduction.
Conclusion
Obturator hip dislocation is a rare variety of regular hip dislocation. The erecta dislocation is also a rare condition. The association of the two dislocations is exceptional, their diagnosis is made clinically and confirmed by standard radiography. The orthopaedic reduction must be done as a matter of urgency, and the triad of reduction, bandaging and early rehabilitation is the guarantee of good evolution.
Links of interest: The authors declare that they have no ties of interest.
References
- Elouakili I, Ouchrif Y, Ouakrim R, Lamrani O, Kharmaz M, Ismael F, et al. Luxation obturatrice de la hanche: un traumatisme rare en pratique sportive. Pan AfricanMedical Journal, 2014; 18: 138.
- Grate Jr I. Luxatio erecta: a rarely seen, but often missed shoulder dislocation. Am J Emerg Med, 2000; 18: 317–321.
- Jon R, Davids MD, Richard D. Luxatio erecta humeri. Clin Orthop, 1990; 252: 145–149.
- Nakagawa Y, Umegaki S, Sakurai G, Ozaki J, Nakagaki K. Luxation erecta of the shoulder. J Shoul.
- Matsumoto K, Ohara A, Yamanaka K, Takigami I, Naganawa T. Luxatio erecta (Inferior dislocation of the shoulder): a report of two cases and review of literature. Injury Extra, 2005; 36: 450–453.
- Stimson LA. Injuries in the main blood-vessels in the axilla caused by efforts to reduce dislocations of the shoulder. Ann Surg, 1885; 2: 369–385.
- Snyder BK. Luxatio Erecta. J Emerg Med 2001; 20: 83–84.
- Goldstein JR, Eilbert WP. Locked anterior-inferior shoulder subluxation presenting as luxatio erecta. J Emerg Med, 2004; 27: 245–248.
- Mallon WJ, Bassett FH 3rd, Goldner RD. Luxatio erecta: the inferior glenohumeral dislocation. J Orthop Trauma, 1990; 4(1): 19-24.
- Mills LD, Barrows T, Benitez F. Bilateral Luxatio Erecta. Emerg Med J, 2003; 24: 61–63.
- Nho SJ, Dodson CC, Bardzik KF, Brophy RH, Bomb BG, MacGillivray JD. The two-step maneuver for closed reduction of inferior glenohumeral dislocation (luxatio erecta to anterior dislocation to reduction). J Orthop Traum, 2006; 20: 354–357.
- Barnet AJ, Eastaugh-Waring SJ, Sarangi PP. Delayed presentation of luxatio erecta dislocatio of the shoulder. Injury extra, 2005; 36: 277–279.
- Toms AD, Williams S, White SH. Obturator dislocation of the hip. J Bone Joint Surg (Br), 2001; 83(1): 113115.
- Boyer P, Bassaine M, Huten D. La luxation obturatrice traumatique chez l'adulte: À propos d'un cas et revue de la littérature. Revue de chirurgie orthopédique, 2004; 90(7): 673–677.
- Canale ST, Manugian AH. Irreductible traumatic dislocation of the hip. J Bone Joint Surg, 1979; 61(1): 7–14.
- Catonné Y, Meyer A, Sariali E, Biette G. Pathologie du complexe pelvi-fémoral du sportif. Pathologie du complexe pelvi-fémoral du sportif, 2009: 88–99.
- Brav EA. Traumatic anterior dislocation of the hip. J Bone Joint Surgery (Am), 1962; 44(A): 1115-1121.
- Epstein HC, Wiss DA. Traumatic anterior dislocation of the hip. Orthopedics, 1985; 8(1): 130-132-134.
- Richards BS, Howe DJ. Anterior perineal dislocation of the hip with fracture of the femoral head: a case report. Clin Orthop. 1988;228: 194-201.
- Badelon O, Leroux D, Huten D, Duparc J. Anterior luxation of 11. Bonnemaison MF, Henderson ED. Traumatic anterior the hip associated with a fracture of the anterior aspect of the acetabulum: Report of a case. AnnChir, 1986; 40(1): 3840.
- Hougaard K. Traumatic posterior dislocation of the hip: prognostic factors influencing the incidence of avascular necrosis of femoral head. Arch Orthop Trauma Surg, 1986; 106(1): 32-35.

