Tumour at the Junction of Hard and Soft Palate: A Benign Mixed Tumor of Minor Salivary Gland, an Unusual Entity
Pankaj Goyal* and Kishan Kumawat
Department of ENT, Apollo ENT Hospital, India
Received Date: 13/02/2023; Published Date: 04/04/2023
*Corresponding author: Dr. Pankaj Goyal, Department of ENT, Apollo ENT Hospital, Pal Road, Jodhpur, Rajasthan, India
Abstract
Minor salivary gland tumours are extremely uncommon. The most common benign salivary gland tumour is Pleomorphic Adenoma (PA), which accounts for approximately 40-70% of all major and minor salivary gland tumours. The palate, buccal mucosa, and lips are the most common sites for intraoral PA. Palatal PA most commonly manifests as a slow-growing submucosal mass on the hard or soft palate. We present a case of palatal PA at the junction of the soft and hard palate that was successfully treated with intraoral surgical excision.
Key words: Palate; Pleomorphic adenoma; Minor salivary glands; Surgical excision
Introduction
The occurrence of benign, minor salivary gland tumours is extremely rare. The literature only lists salivary gland cancers as less than 3% of head and neck tumours [1]. Pleomorphic adenoma (PA) makes up between 40 and 70 percent of all major and minor salivary gland tumours [2]. The minor salivary gland benign tumour known as PA is the most prevalent type. The palate, lip, buccal mucosa, mouth's floor, lingual tonsil, pharynx, and retromolar region are the areas where this tumour appears most frequently in the oral cavity [3]. The condition manifests clinically as a submucosal tumour devoid of any inflammation [4]. On the basis of the history, physical examination, cytology, and histology, PA is diagnosed. The location, size, and extent of the tumour to the surrounding superficial and deep tissues can be determined using Computed Tomography (CT) scans and Magnetic Resonance Imaging (MRI). A radiological inquiry in the form of a CT scan is required to be done in order to keep in mind that it could end up being malignant. After radiological assessment of the surrounding area, surgical excision will be necessary from a therapy standpoint. Wide local excision with the removal of any affected periosteum or bone is the preferred course of treatment for PA hard palate region. Simple enucleation of this tumour has a high risk of local recurrence and ought to be avoided [5].
Case Report
A 45-year-old male patient presented to our Apollo E.N.T. hospital with a one-year history of painless swelling in the upper left palatal region. His medical history was minimal, and he had no drug allergies. Intraoral examination revealed a single ovoid mass 2 x 2 cm (Figure 1) in diameter at the junction of the hard and soft palate on the left side. The mass was non-tender, slow-growing, firm, and well defined, with no radiographic evidence of bone involvement (computed tomography scan-figure 2). Following a routine examination and proper consent, the patient was scheduled for surgical excision (intraoral approach- figure 3). After the tumour had been completely removed, the surgical site was predominantly sutured with absorbable suture material (vicryl 3-0 round body) and post op patient shifted to recovery. Intravenous antibiotics were started for two days. The third day, the patient was discharged. Post-operative recovery went well. According to the histopathological report, it was a pleomorphic adenoma.
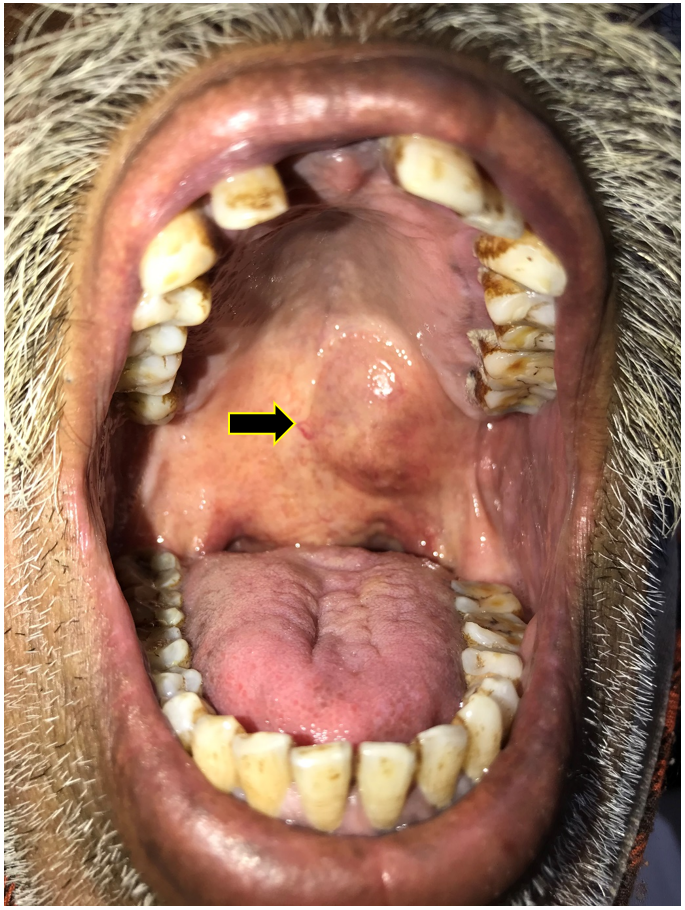
Figure 1: Clinical picture showing soft cystic swelling (2x1cm) at the junction of left sided soft and hard palate.
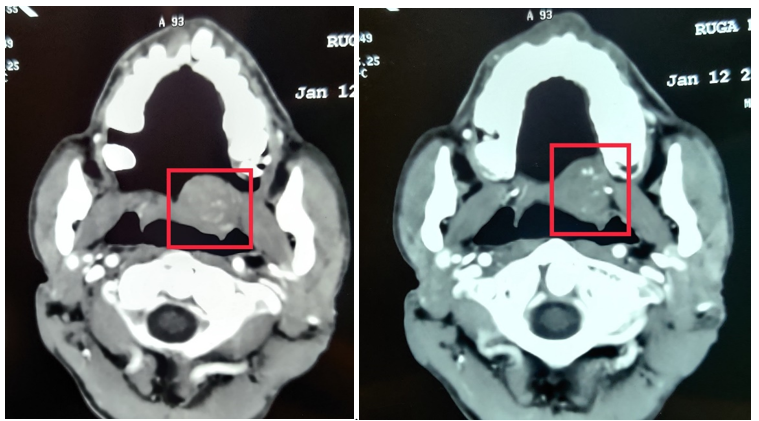
Figure 2: CECT (Contrast Enhanced Computed Tomography) scan axial plane demonstrating a well-defined enhancing mass lesion arising from junction of hard and soft palate with no evidence of bone erosion.

Figure 3: Intraoperative picture after removal of tumor without any underlying bony erosion.

Figure 4: Surgical specimen.
Discussion
The most typical salivary gland lesion is usually a benign mixed tumour or pleomorphic adenoma, however minor salivary gland lesions are quite rare. The parotid, the submandibular, and the minor salivary glands account for 84%, 8%, and 4-6%, respectively, of the cases. With a 2:1 ratio, women are more predisposed [6]. It can happen at any stage of life, but it typically appears in the fourth and fifth decades. The palate's minor salivary glands (which account for roughly 73% of cases), upper lip (17%), buccal mucosa, the floor of the mouth, the lingual tonsil, the throat, and the retromolar region are the next most likely sites for it to develop. It appears as a submucosal bulge with a painless, gradually enlarging, hard, and well-defined swelling at the palatal region [7]. But if the underlying mucosa is ulcerated, malignant characteristics should be taken into consideration.
Pleomorphic refers to these tumours' embryogenic origin, which includes both mesenchymal and epithelial components [6]. These tumours develop from intercalated and myoepithelial cells [7]. Various small salivary gland tumours, especially mucoepidermoid carcinoma, as well as other benign and malignant mesenchymal lesions such neurofibroma and rhabdomyosarcoma are included in the differential diagnosis of the palatal lesions [8]. The precise extent of the tumour and any underlying bone degradation can be determined with great accuracy by radiological imaging. The key diagnostic technique for these tumours [9] is a Computed Tomography (CT) scan, which can rule out the pressure effect of a tumour on the underlying bone. The preferred form of treatment is surgical excision. Recurrence and longevity are risk factors for malignant transformation. There is a 1.9–23.3% tendency for malignant transformation [10]. Differential diagnoses for PA include salivary gland tumours, mucoepidermoid carcinoma, adenoid cystic carcinoma, and both odontogenic and non-odontogenic cysts, soft tissue tumours, palatal abscesses, and odontogenic cysts. Palatal tissues house minor salivary gland tissues as well as soft tissue components. As a result, other possible diagnosis for this case should include soft tissue tumours including neurofibroma, fibroma, lipoma, and neurilemmoma as well as tumours of the salivary gland. At the intersection of the hard and soft palates, the patient in our situation experienced a painless swelling. Over the course of a year, it gently advanced and was not painful. We completely removed the tumour surgically, and the underlying bone was not eroded. The absorbable vicryl suture was used principally to close the post-excision surgical incision, which healed successfully. Patient was asymptomatic for the entire year of follow-up.
Conclusion
Palatal pleomorphic adenoma is an uncommon condition that typically affects adults. Minor salivary glands rarely generate benign mixed tumours. The diagnosis is really challenging. A computed tomography scan is necessary to detect any pressure effects or underlying bone degradation. However, malignancy should be taken into consideration, therefore histopathological correlation is essential. Wide local excision with or without removal of periosteum and curettage of bone during surgery is the only option for treatment.
Compliance with Ethical Standards: The procedure performed in this case report was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Funding: This study is not funded by any resources.
Conflict of Interest: The author (s) declares no potential conflicts of interest with respect to the research, authorship, and/or publication of this paper.
Ethical Approval: The study was published with the written consent of the patient.
References
- Luna MA, Batsakis JG, El-Naggar AK. Salivary gland tumors in children. Ann Otol Rhinol Laryngol, 1991; 100: 869–871.
- Jorge J, Pires FR, Alves FA, Perez DEC, Kowalski LP, Lopes MA. Juvenile intraoral pleomorphic adenoma: report of five cases and review of the literature. Int J Oral Maxillofac Surg, 2002; 31: 273–275.
- Sanjay Byakodi, Shivayogi Charanthimath, Santosh Hiremath, Kashalikar JJ. Pleomorphic adenoma of palate: a case report. Int J Dent Case Reports, 2011; 1: 36–40.
- Mubeen K, Vijayalakshmi KR, Patil AR, Giraddi GB, Singh C. Benign pleomorphic adenoma of minor salivary gland of palate. J Dent Oral Hyg, 2011; 3: 82–88.
- Mubeen K, Vijayalakshmi KR, Patil AR, Giraddi GB, Singh C. Benign pleomorphic adenoma of minor salivary gland of palate. J Dent Oral Hyg, 2011; 3: 82–88.
- Batsakis JG. Neoplasms of the minor and ‘lesser’ major salivary glands. In: Tumors of the head and neck. The Williams and Wilkins Company, Baltimore, 1981; p 38–47.
- Suen JY, Synderman NL. Benign neoplasms of the salivary glands. In: Cummings CW, Fredrickson JM, Harker LA, Krause CJ, Schuller DE (eds) Otolaryngology—head and neck surgery. Mosby Year Book, St. Louis, 1993; pp 1029–1042.
- Dhanuthai K, Sappayatosok K, Kongin K. Pleomorphic adenoma of the palate in a child: a case report. Med Oral Patol Oral Cir Bucal, 2009; 14: E73–E75.
- Daniels JS, Ali I, Al Bakri IM, Sumangala B. Sumangala: Pleomorphic adenoma of the palate in children and adolescents: A report of 2 cases and review of the literature: J Oral Maxillofac Surg, 2007; 65: 541-549.
- Ethunandan M, Witton R, Hoffman G, Spedding A, Brennan PA. Atypical features in pleomorphic adenoma: A clinicopathological study and implication for management. Int J Oral Maxillofac Surg, 2006; 35(12): 608-612.

