Every Hot Spot is not Cancer - Pulmonary Tuberculosis Mimicking Lung Cancer in PET-CT
Ankita Goyal1,*, Santosh Rai1, Vishak Acharya2 and Jyoti Kini3
1Department of Radiodiagnosis, Kasturba Medical College, Manipal Academy of Higher Education, India
2Department Of Chest Medicine, Kasturba Medical College, Manipal Academy of Higher Education, India
3Department Of Pathology, Kasturba Medical College, Manipal Academy of Higher Education, India
Received Date: 03/02/2023; Published Date: 27/03/2023
*Corresponding author: Ankita Goyal, MBBS, Junior Resident, Department of Radiodiagnosis, Kasturba Medical College, Mangalore, Manipal Academy of Higher Education, Manipal, Karnataka, India
Introduction
Tuberculosis is caused by a bacteria mycobacterium tuberculosis. In 2014, there were an estimated 9.6 million new TB cases: 5.4 million among men, 3.2 million among women and 1.0 million among children. There were also 1.5 million TB deaths (1.1 million among HIV-negative people and 0.4 million among HIV-positive people), of which approximately 890 000 were men, 480 000 were women and 140 000 were children [1].
Differentiation of malignant from benign pulmonary nodules is a common dilemma in diagnostic imaging. The primary objectives for treatment of patients with solitary pulmonary nodules are to expedite the removal of malignant lesions that may be curable surgically and to decrease the use of thoracotomy in benign entities [2]. Metabolic imaging with 2-(18F) FDG (Fluoro-deoxy-glucose) positron emission tomography (PET) is being used more and more to differentiate benign from malignant focal lesions and it has been shown to be more efficacious than conventional chest Computed Tomography (CT). It has a unique ability to differentiate benign from malignant nodules, and it offers a different approach to the diagnosis of chest diseases because it exploits fundamental biochemical differences between benign and malignant cells [3].
Active tuberculosis or tuberculoma, acute and chronic pneumonia, abscess, fungal infection, sarcoidosis, parasitic infestation, and pneumoconiosis are frequent causes of increased 18F-FDG uptake [4].
Due to the high prevalence of tuberculosis in India, false positive cases during oncologic workup with FDG-PET are commonly encountered in practice [5-7]. Though FDG PET/CT is not specific for tuberculosis, it plays an important role in the evaluation of known or suspected TB cases. FDG PET/CT can determine the activity of lesions, guide biopsy from active sites, assess disease extent, detect occult distant foci, and evaluate response to therapy [3].
Case Report
A 60 years old male patient is referred with complaints of chest tightness, cough with expectoration for 4 weeks and 2 episodes of hemoptysis in last 2 weeks. He has history of smoking 20 cigarettes per day for 35 years and estimated as 35 pack years. No history of fever. No history of significant weight loss. On clinical examination the vitals were stable. Routine laboratory investigations were within normal limits. Chest radiograph and contrast enhanced CT shows a heterogeneous mass lesion in the right hilar region (Figure 1A, 1B). 18-FDG PET CT done was showing a mass lesion in the right hilar region with high metabolic activity (Figure 1 D). With these a provisional diagnosis of malignancy is made but for histopathological proof the patient is subjected to CT guided FNAC and transbronchial biopsy of the mass (Figure 1C). Strikingly the FNAC and biopsy result are positive for Tuberculosis and negative for malignant cells. Fine needle aspiration cytology revealed clusters of bronchial epithelial cells with uniform nuclei and a background of granular caseous necrotic debris and numerous AFB positive tubercle bacilli (Figure 2A, 2B). Transbronchial Lung biopsy shows caseating epithelioid granulomas and occasional multinucleated giant cells and foci of caseous necrosis. So, the patient was diagnosed as tuberculosis and treated with anti-tubercular drugs for a 6 months regimen. The Chest radiograph on follow up after 6 months revealed complete resolution of the lesion (Figure 3).
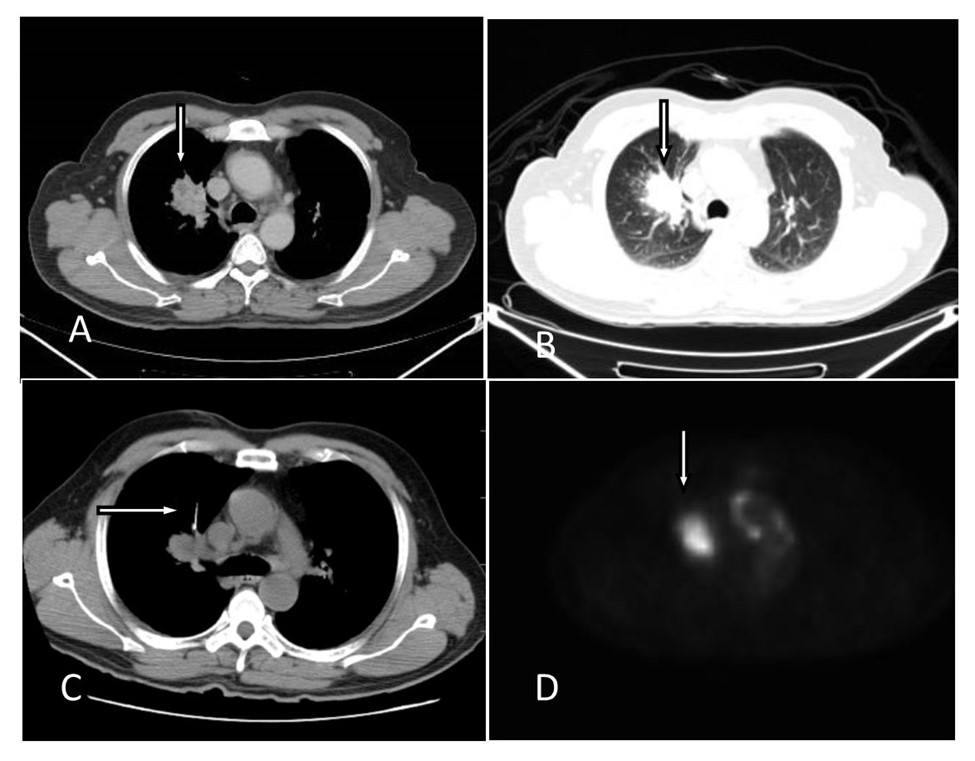
Figure 1:
A & B: Contrast enhanced Computed Tomography (CT) shows heterogeneously enhancing lesion with irregular margins at the right hilum of the Lung (arrow).
C: CT guided biopsy of the right perihilar mass lesion. Thick arrow pointing at the biopsy needle.
D: PET CT image. Arrow pointing at mass lesion in the right hilar region with high metabolic activity.
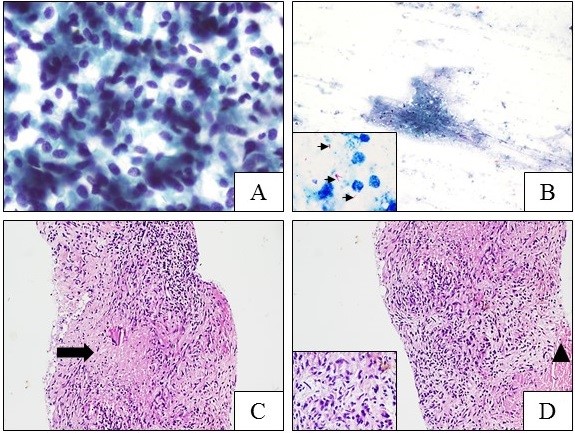
Figure 2:
A & B: FNAC of the lung lesion:
A: Clusters of bronchial epithelial cells with uniform nuclei. [Pap stain; 400X] B: The background shows granular caseous necrotic debris. [Pap stain; 40X] Inset: Numerous AFB positive tubercle bacilli (arrows). [Pap stain; 1000X]
C & D: Transbronchial Lung biopsy:
C: Pulmonary tuberculosis diagnosed by tranbronchial biopsy that shows caseating epithelioid granulomas (arrow) and occasional multinucleated giant cells. [H & E; 100X]
D: Epithelioid cell aggregates forming granulomas admixed with lymphocytes and plasma cells. Foci of caseous necrosis also noted (arrow head). Inset: Epithelioid cells that are elongated with pale granular eosinophilic cytoplasm and central ovoid nuclei. [H & E; 400X]

Figure 3: Chest radiograph on follow up after 6 months revealed complete resolution of the lesion.
Discussion
Tuberculosis (TB) is a major global health problem. It causes ill-health among millions of people each. In India 2.2 million new TB cases were estimated. There were 220 000 deaths (189 000 among HIV negative people and 31 000 among HIV positive people) [1]. Timely diagnosis and correct treatment can cure tuberculosis in most patients.
TB and lung cancer have been confused and misdiagnosed especially in countries with low TB incidence and risk of diagnosis of TB getting missed. Differentiation according to the radiological findings cannot be provided. The diagnosis has to be confirmed by pathological and microbiological tests. Jin Mo Goo and his colleagues did study on 10 cases of pulmonary tuberculoma who underwent PET-CT in that 9 cases showed high FDG uptake, which was finally diagnosed by wedge resection or lobectomy or needle biopsy [2].
Yaichiro Hashimoto and his colleagues did a study on 360 consecutive patients who underwent PET-CT they restrospectively found out 43 patients had solid pulmonary nodules. 16 were malignant and 27 were benign. PET-CT correctly identified all 16 cases but yielded false positive results in 10 out of 27 benign cases [7]. Because of active glucose metabolism caused by active granulomatous inflammation, tuberculomas sometimes have been reported to accumulate 18F-FDG and to cause PET scans to be interpreted as false-positive for malignancy. 11C-choline PET scans can help differentiate between lung cancer and tuberculoma. The standard uptake value of tuberculoma is low in 11C-choline PET scans [5]. Few malignant neoplasms of lung may show decreased uptake of 18F-FDG-PET (Mucinous and nonmucinous Bronchioloalveolar Carcinomas (BACs), adenocarcinomas with BAC components, carcinoids, and mucoepidermoid carcinomas).
18F-FDG PET/CT is now the cornerstone of staging procedures in the state-of-the-art management of HL and aggressive NHL. It plays an important role in staging, restaging, prognostication, planning appropriate treatment strategies, monitoring therapy, and detecting recurrence [6]. PET/CT may identify metabolically active areas within the mass and help to optimize the diagnostic tissue yield - PET providing physiological information and CT providing the anatomical details [8].
In conclusion, differentiating of lung TB from neoplasm, according to the clinical and radiological findings can be challenging. Both diseases present parenchymal infiltrates with high or low metabolic activity on the 18F-FDG-PET scanning and can have similar symptoms [9]. On the other hand, the diagnosis of pulmonary TB can be established with relatively simple microbiological tests. FNAC and biopsy is more sensitive and specific method in diagnosing and differentiating malignant lesions from benign and inflammatory lesions. This case shows that pulmonary tuberculosis can manifest as pulmonary nodules mimicking lung metastasis. CT guided FNAC or biopsy is warranted for confirmatory diagnosis.
Teaching points:
- Active glucose metabolism caused by active granulomatous inflammation, tuberculomas sometimes have been reported to accumulate 18F-FDG and to cause PET scans to be interpreted as false-positive for malignancy
- FNAC and biopsy is more sensitive and specific method in diagnosing and differentiating malignant lesions from benign and inflammatory lesions.
Differential diagnosis:
| Primary lung malignancy |
| Tuberculoma |
| Metastasis |
Source of Support: Nil
References
- Global tuberculosis report. WHO, 2015.
- Jin Mo Goo, Jung-Gi Im, Kyung-Hyun Do, Jeong Seok Yeo, Joon Beom Seo, Hyae Young Kim, et al. Pulmonary Tuberculoma Evaluated by Means of FDG PET: Findings in 10 Cases. RSNA, 2000; 216: 117-121.
- Harkirat S, Anand SS, Indrajit IK, Dash AK. Pictorial essay: PET/CT in tuberculosis. Indian J Radiol Imaging, 2008; 18: 141-147.
- Jung Min Chang, Hyun Ju Lee, Jin Mo Goo, Ho-Young Lee, Jong Jin Lee, June-Key Chung, et al: False Positive and False Negative FDG-PET Scans in Various Thoracic Diseases. Korean J Radiol, 2006; 7: 57-69.
- Yeon Joo Jeong, Kyung Soo Lee: Pulmonary Tuberculosis: Up-to- Date Imaging and Management. AJR 2008; 191: 834–844.
- D'souza MM, Jaimini A, Bansal A, Tripathi M, Sharma R, Mondal A, et al. FDG-PET/CT in lymphoma. Indian J Radiol Imaging, 2013; 23: 354-365.
- Yaichiro Hashimoto, Tetsuya Tsujikawa, Chisato Kondo, Masako Maki, Mitsuru Momose, Atsushi Nagai: Accuracy of PET for Diagnosis of Solid Pulmonary Lesions with 18F-FDG Uptake below the Standardized Uptake Value of 2.5. J Nucl Med, 2006; 47: 426–431.
- Govindarajan MJ, Kalyanpur A, Nagaraj KR, Ravikumar H, Kallur KG, Sridhar PS. Technical note: Preprocedural PET/CT guidance for fine needle aspiration cytology of a lung mass. Indian J Radiol Imaging, 2008; 18: 90-91.
- Sung Shine Shim, Kyung Soo Lee, Byung-Tae Kim, Joon Young Choi, Myung Jin Chung, Eun Jeong Lee: Focal parenchymal lung lesions showing a potential of false-positive and false-negative interpretations on integrated PET/CT. AJR, 2006; 186: 639–648.

