Transoral Incisionless Fundoplication Versus Nissen Fundoplication in the Management of Refractory Gastroesophageal Reflux Disease
Shaniah Holder1,*, Yesenia Brito2, Janice Mwaniki2, Zayn Mehboob2 and Frederick Tiesenga3
1Department of Medicine, American University of Barbados School of Medicine, Barbados
2Department of Medicine, Saint George’s University School of Medicine, Grenada
3Department of Surgery, Community First Hospital, USA
Received Date: 30/01/2023; Published Date: 03/03/2023
*Corresponding author: Shaniah Holder, Department of Medicine, American University of Barbados School of Medicine, Barbados
Abstract
Gastroesophageal Reflux Disease (GERD) affects millions of people and is known to decrease the quality of life. Management strategies range from conservative measures such as lifestyle changes to medication with the use of Proton Pump Inhibitors (PPIs) and even surgical treatment with fundoplication. Fundoplications are normally done laparoscopically, such as the Nissen Fundoplication, however, there has been a groundbreaking advancement in the procedure. Transoral Incisionless Fundoplication (TIF) is an endoscopic procedure performed under general anesthesia which allows the stomach to be folded and secured around the lower esophageal sphincter, preventing reflux. TIF is an effective treatment option for patients who have experienced the symptoms of GERD that are refractory to a medicinal approach. It is safe, well tolerated by patients, and is associated with fewer postoperative adverse effects. In this report, we will describe the case of a 53-year-old male with a history of GERD refractory to medications. He was subsequently treated surgically with the TIF procedure and showed significant improvement in his symptoms. The aim of this report is to describe the benefits of TIF in comparison to Nissen Fundoplication in the management of GERD.
Keywords: GERD; Refractory Esophageal Reflux; Nissen Fundoplication; Transoral incisionless Fundoplication; Reflux Management
Introduction
Gastroesophageal Reflux Disease (GERD) is a chronic condition that affects approximately 15-30% of the US adult population and is characterized by a weak Lower Esophageal Sphincter (LES) allowing the retrograde flow of stomach acid into the esophagus [1]. GERD is multifactorial with risk factors including obesity, smoking, excessive caffeine and alcohol consumption, and hiatal hernias [2]. Heartburn that is exacerbated after eating or lying flat, upper abdominal or chest pain, and dysphagia are some features of GERD [2]. Complications include esophageal erosion, ulceration, stricture formation, and Barrett esophagus which can lead to esophageal adenocarcinoma due to intestinal-type metaplasia of the epithelium [2,3]. Medical and surgical treatments are utilized to prevent worsening reflux and its associated complications.
The initial management of GERD consists of lifestyle changes such as weight reduction, dietary modification, and Proton Pump Inhibitor (PPI) use [2]. Approximately 30-40% of people develop refractory GERD; in these cases, surgical intervention is warranted [4]. The initial surgical management of refractory GERD is Nissen Fundoplication (NF) [5]. It is an invasive laparoscopic procedure that involves a tight 360-degree wrap of the gastric fundus around the esophagus at the gastro-esophageal junction, in an effort to restore the Gastroesophageal Valve (GEV) strength [5]. As a result of this complete and tight fundoplication, a variety of complications have been reported in over 7% of patients [6].
A less invasive, surgical option known as the Transoral Incisionless Fundoplication (TIF) was FDA-approved in 2007 and utilizes the Esophyx ® device (EndoGastric Solutions, Redmond, WA, USA) [7]. TIF is an endoscopic procedure that has a similar mechanism of action as NF. However, instead of a 360-degree wrap, it incorporates a 270-degree wrap that is one to three centimeters in length, thus creating a strong, tensile Gastroesophageal Valve (GEV) that withstands acid reflux [8]. This revolutionary procedure has become more popular over the years and it has improved the quality of life in many persons with refractory GERD. This endoscopic incisionless method is associated with less discomfort, faster recovery time, and affordable costs compared to standard surgical modes such as NF [7].
In this case report and literature review, we present a 53-year-old male with refractory GERD and subsequent esophagitis that has responded favorably to the TIF procedure.
Case Presentation
We present a 53-year-old male with a body mass index (BMI) of 27 kg/m2 and a 20-year medical history of GERD. There was no positive family history, the patient was a nonsmoker and consumed only one alcoholic drink a day. However, his dietary habits were poor with high fat and low fiber intake. He complained of worsening intermittent heartburn that was exacerbated when lying flat, upper abdominal discomfort, and occasional bouts of nausea. His symptoms increased in severity at night, leading to sleep disruption and subsequent difficulty keeping up with his daily activities.
Two years ago, an Esophagogastroduodenoscopy (EGD) with biopsy was conducted and showed squamous mucosa with mild basal layer hyperplasia and intracellular edema, indicating reflux esophagitis. (Figure 1) below shows the pathological findings of GERD.

Figure 1: Squamous cells with mild basilar cell hyperplasia, intracellular edema, and scant eosinophils.
The patient implemented dietary changes and used Proton Pump Inhibitors (PPI), however, there was no symptomatic alleviation despite increasing the dosage. Due to his normal BMI, refractory GERD, and lack of a significant past medical history, the patient was an excellent candidate for TIF.
During the surgery, an EGD showed the Gastroesophageal (GE) junction at 45cm with no visualization of a hiatal hernia. At this time, the EsophyX® device (Endogastric Solutions® Redmond, WA) was inserted and a 270-degree 3cm wrap was created utilizing sequential firings of nonabsorbable H-type fasteners. (Figure 2) below shows the top of the stomach wrapped around the esophagus.
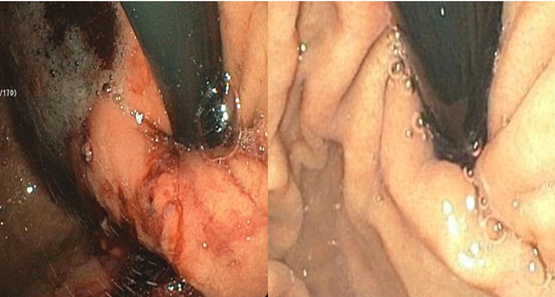
Figure 2: Endoscopic view of the superior portion of the stomach wrapped around the esophagus.
Repeat endoscopy after the procedure showed an excellent valve and no bleeding which is shown in (Figure 3) below.
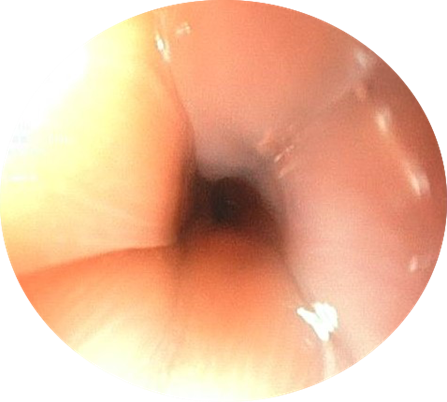
Figure 3: Endoscopic view of the gastroesophageal junction after the TIF procedure.
There were no surgical complications and the patient was discharged on postoperative day one. He followed up on postoperative day seven and reported significant improvement in his reflux symptoms. He denied any recent episodes of heartburn and stated that his sleep had not been affected since the procedure. The only adverse effect reported by the patient was mild chest tightness. He has been tolerating the liquid diet well and plans to advance his diet with close follow-up.
Discussion
Transoral Incisionless Fundoplication (TIF) is a minimally invasive procedure that involves the reconstruction of the GEV without laparoscopic incisions [8]. It utilizes the EsophyX ® device which is inserted through the oral cavity and advanced into the stomach where it lengthens, strengthens, and tightens the lower esophageal sphincter (LES) by creating a 3 cm, 270-degree esophagogastric fundoplication [7,8]. The device places 20+ SerosaFuse fasteners at four different positions around the wrap to stabilize it, thus restoring the integrity of the GEV and subsequently correcting the underlying cause of GERD [1,8]. The TIF procedure is revolutionary, with an operation time of one-hour maximum and an approximate success rate of 98% [9]. In a study consisting of 257 patients, 51 underwent the TIF procedure. 50 out of 51 patients reported complete symptomatic relief, indicating efficacy [9].
There are criteria that must be met before being considered for the TIF procedure. Refractory GERD, the presence of a hiatal hernia on EGD, and Barrett's esophagus are features that make patients a good candidate for this procedure [10]. Some contraindications include a BMI over 35 kg/m2, age over 70 years old, a hiatal hernia that’s more than 3cm, irreducible hernias, and severe medical comorbidities such as heart or lung disease [10]. These may decrease the efficacy of the procedure or affect the patient’s ability to tolerate it. Our patient had the classical symptoms of GERD that were refractory to the maximum dosage of PPI; there was no hiatal hernia on preoperative EGD and the patient did not have any severe health comorbidities, thus making him a good candidate.
There is a paucity of research comparing Nissen Fundoplication and TIF. A network meta-analysis compared the efficacy of TIF, NF, and PPI therapy. They found that although there was more sphincter enhancement in NF, there was an increased quality of life in persons who underwent TIF [11]. NF includes a tight fundoplication to rebuild the GEV, however, TIF creates a longer valve that is not twisted or torqued allowing food to pass easily [12]. The gastric blood vessels and vagus nerve branches are in close proximity to the fundus and distal esophagus; when damaged during circumferential wrapping, dysphagia and gastroparesis may arise which presents as bloating, belching, and upper abdominal discomfort [13]. In TIF, the GEJ is only partially tightened, thus decreasing the rate of these complications, and allowing patients to resume their daily activities quickly [12]. TIF is also an incisionless procedure, so it eliminates the risk of skin infections, scarring, and pain associated with laparoscopic surgery [7].
Studies have shown that 90% of patients who undergo TIF have improved symptomatic control of refractory GERD in comparison to standard methods of management [9]. In a study, 94% of patients reported symptomatic resolution that led to the complete cessation of PPI use [9]. Furthermore, TIF is a durable solution for GERD with studies showing that the procedure maintains its efficacy for up to ten years [14]. Patients would not require multiple surgeries or future treatments which are cost-effective. Some notable side effects of TIF include mild throat, chest, or shoulder pain which resolves within a couple of weeks [11]. Studies show that the risk of serious complications such as mucosal tears and bleeding is approximately 3% to 10% [15].
The TIF diet is followed for several weeks after the surgery. It allows the stomach and esophagus to settle into their new shape and heal, preventing complications [11]. The diet consists of liquids for one-week, soft foods for two weeks, and solid foods after the third week [15]. Spicy or fried foods and caffeine should be avoided for several months to prevent gastroesophageal irritation [15].
In this case, our patient who had been suffering from refractory GERD benefitted immensely from the TIF procedure with a report of complete symptom resolution. Due to its minimally invasive nature, the patient experienced less pain and discomfort with no postoperative complications. This advanced fundoplication procedure should be highly considered in the treatment of moderate to severe refractory GERD. Decreased recovery times, instant symptomatic relief and reduced risk of side effects are some of TIF's notable benefits, which make it superior to Nissen Fundoplication regarding a patient’s quality of life.
Conclusion
Medically refractory GERD is treated surgically with either laparoscopic or endoscopic fundoplication. By restoring the antireflux capacity of the GEV, these procedures allow the remission of GERD symptoms. TIF is a safe, durable, and cost-effective mode of surgical management. With minimal invasiveness, long-term efficacy, and decreased surgical complications, this procedure offers an increased quality of life to patients when compared to its laparoscopic counterpart. Further research comparing the long-term benefits and limitations of both procedures is required. It is important that physicians discuss both options with their patients and allow shared decision-making to reflect the patient's values, in an effort to optimize their clinical outcomes.
Author Contributions
Shaniah Holder: Concept and Design of study, Acquisition of data, drafting article, revising article. Guarantor Author
Yesenia Brito: Concept and Design of study, drafting article intellectual content, revising article
Janice Mwaniki: Acquisition of data, drafting article, revising article
Zayn Mehboob: Acquisition of data, drafting article, revising article
Frederick Tiesenga: Final Approval, Intellectual Content, revising article
Informed Consent: A signed statement of informed consent was obtained for publication of the details of this case
Competing Interests: None
Grant Information: None
References
- Freedburg DE, Kim LS, Yang Y. The Risks and Benefits of Long-term Use of Proton Pump Inhibitors: Expert Review and Best Practice Advice from the American Gastroenterological Association. AGA Cln Practice Update: Expert Review, 2017; 152(4): 706-715. DOI: 10.1053/j.gastro.2017.01.031.
- Katz PO, Gerson LB, Vela MF. Guidelines for the Diagnosis and Management of Gastroesophageal Reflux Disease. American Journal of Gastroenterology, 2013; 108(3): 308-328. DOI: 10.1038/ajg.2012.444.
- van Zanten SV. Chronic GERD and risk of esophageal adenocarcinoma: Should we screen with gastroscopy? CMAJ, 2020; 192(27): 781-782. DOI: 10.1503/cmaj.200697.
- Delshad SD, Almario CV, Chey WD, Spiegel BMR. Prevalence of Gastroesophageal Reflux Disease and Proton Pump Inhibitor-Refractory Symptoms. Gastroenterology, 2020; 158(5): 1250-1261. DOI: 10.1053/j.gastro.2019.12.014
- Shan CX, Zhang W, Zheng XM, Jiang DZ, Liu S, Qiu M. Evidence-based appraisal in laparoscopic Nissen and Toupet fundoplications for gastroesophageal reflux disease. World J Gastroenterol, 2010; 16(24): 3063-3071. DOI: 10.3748/wjg.v16.i24.3063.
- Sandhu DS, Fass R. Current Trends in the Management of Gastroesophageal Reflux Disease. Gut Liver, 2018; 12(1): 7-16. DOI: 10.5009/gnl16615.
- Ihde GM. The evolution of TIF: transoral incisionless fundoplication. Therap Adv Gastroenterol, 2020; 13. DOI: 10.1177/1756284820924206.
- The EsophyX® Device: making transoral reconstructive surgery poss, 2022.
- Canto MI, Olaya IBG, Mohamad D, Vivek K, Mouen AK, Kalloo AN, et al. Outpatient Transoral Incisionless Fundoplication (TIF 2.0) is Safe and Effective for Treatment of Proven Gastroesophageal Reflux Disease (GERD) and Laryngopharyngeal Reflux Disease (LPRD): A Single Center Prospective. Poster Abstracts, 2020; 91(6). DOI: 1016/j.gie.2020.03.1025.
- Testoni PA, Mazzoleni G, Testoni SG. Transoral incisionless fundoplication for gastro-esophageal reflux disease: Techniques and outcomes. World J Gastrointest Pharmacol Ther, 2016; 7(2): 179-189. DOI: 10.4292/wjgpt.v7.i2.179
- Richter JE, Kumar A, Lipka S, et al. Efficacy of Laparoscopic Nissen Fundoplication vs Transoral Incisionless Fundoplication or Proton Pump Inhibitors in Patients with Gastroesophageal Reflux Disease: A Systematic Review and Network Meta-analysis. Gastroenterology, 2018; 154(5): 1298-1308. DOI: 10.1053/j.gastro.2017.12.021.
- Transoral Incisionless Fundoplication (TIF), 2022.
- Shafi MA, Pasricha PJ. Post-surgical and obstructive gastroparesis. Curr Gastroenterol Rep, 2007; 9(4): 280-285. DOI: 10.1007/s11894-007-0031-2.
- Testoni PA, Testoni S, Distefano G, Mazzoleni G, Fanti L, Passaretti S. Transoral incisionless fundoplication with EsophyX for gastroesophageal reflux disease: clinical efficacy is maintained up to 10 years. Endosc Int Open, 2019; 7(5): 647-654. DOI: 10.1055/a-0820-2297.
- Stefanidis G, Viazis N, Kotsikoros N, Tsoukalas N, Lala E, Theocharis L, et al. Long-term benefit of transoral incisionless fundoplication using the esophyx device for the management of gastroesophageal reflux disease responsive to medical therapy. Diseases of the Esophagus, 2016. DOI: 10.1111/dote.12525.

