Simultaneous Development of Hemorrhagic and Gangrenous Cholecystitis Secondary to Metastatic Pancreatic Cancer
Shaniah Holder1,*, De’jeau Pyfrom2, Ulochi Nwagwu3, Obinna Okolocha3, Joancy Archeval-Lao3 and Frederick Tiesenga4
1Department of Surgery, American University of Barbados School of Medicine, Barbados
2Department of Surgery, Saint James School of Medicine, Anguilla
3Department of Surgery, Saint George’s University School of Medicine, Grenada
4Department of Surgery, Community First Hospital, USA
Received Date: 16/01/2023; Published Date: 15/02/2023
*Corresponding author: Shaniah Holder, Department of Surgery, American University of Barbados School of Medicine, 1325 East 52nd Street Chicago IL 60615, USA
Abstract
Pancreatic carcinoma is one of the most aggressive forms of cancer that often presents in its late stages. Due to its silent nature, it can manifest with a rapid clinical progression and, similarly to other types of cancer, metastasize to other organs. In a few instances, metastatic cancer can invade bile ducts and arteries, leading to an obstruction that can precipitate the formation of hemorrhagic and gangrenous cholecystitis. Little research has explored the association between pancreatic cancer and simultaneous hemorrhagic and gangrenous cholecystitis development. This ground-breaking report showcases a 60-year-old male patient presenting with jaundice, abdominal pain, and CA-19-9. Computed Tomography (CT) discovered severe metastatic pancreatic cancer and cholecystitis. Surgical management with laparoscopic cholecystectomy discovered a gangrenous gallbladder with hemorrhagic bile and extensive areas of necrosis. This report aims to examine the etiology of gangrenous and hemorrhagic cholecystitis and its simultaneous development secondary to metastatic pancreatic cancer.
Keywords: Pancreatic Cancer; Cholecystitis; Hemorrhagic Cholecystitis; Gangrenous Cholecystitis; Metastatic Disease; Cholecystectomy
Introduction
Pancreatic cancer is considered one of the deadliest malignancies, with projections to become the second leading cause of cancer-related deaths in the near future [1]. The 5-year survival rate at the time of diagnosis is approximately 10% in the United States due to most patients presenting with metastatic or unresectable disease [1]. The clinical progression of pancreatic cancer is typically aggressive, with a high symptom burden and a declining quality of life [2]. As pancreatic cancer progresses, acute cholecystitis is a common symptomatic manifestation of disease progression [3].
Cholecystitis is usually caused by inflammation of the gallbladder wall in the setting of outflow obstruction, often in the presence of gallstones [4]. However, in some instances, there may be an obstruction in the absence of gallstones. The inflammatory process is thought to arise due to biliary stasis or ischemia secondary to severe illnesses [4]. Metastatic cancer increased the risk of cholecystitis due to direct obstruction of the bile duct, malnutrition, and a decrease in immunity [3]. When left untreated, AC can progress to gangrenous and hemorrhagic cholecystitis (GC, HC) due to extensive tissue necrosis and hemorrhaging within the gallbladder lumen, respectively [4]. One study aimed to identify the risk factors associated with developing gangrenous and hemorrhagic cholecystitis and noted that approximately 45% of these cases were associated with anticoagulation use [5]. Other notable risk factors included obstructive cholecystitis, trauma, infections, and biliary neoplasms [5]. Accurate diagnosis and prompt treatment are paramount, given that gallbladder perforation and intraperitoneal hemorrhaging are common complications associated with a high mortality rate [5].
While several studies have outlined the aforementioned associated risk factors, there are few to no studies addressing the association of metastatic pancreatic carcinoma with the development of simultaneous hemorrhagic and gangrenous cholecystitis. This report presents a patient with stage IV pancreatic cancer who had an incidental finding of hemorrhagic and gangrenous cholecystitis.
Case Report
In this case, we present a 60-year-old male with a known history of alcohol abuse who presented to the ED for a recent onset of altered mental status and bilateral leg swelling. The underlying circumstance causing his symptoms was unknown, as the patient had difficulty remembering the details of his medical history. On physical examination, he was noted to be pale and cachectic in appearance with diffuse upper and lower extremity weakness and apparent muscle wasting; he also had scleral icterus and vague upper abdominal tenderness that worsened on palpation. Laboratory tests were significant for elevations in calcium 12.4 (N: 8.5-10.2), bilirubin 7.5 (N: 0.1-1.2), AST 177 (N: 8-33), lipase 402 (N: 0-160) and the pancreatic tumor marker CA 19-9 385 (N: <37).
Due to the abnormal labs and positive physical findings, there was a high clinical suspicion of malignancy, specifically pancreatic cancer; therefore, the patient underwent a CT scan of his abdomen. It showed an ill-defined low attenuation within the head and uncinate process of the pancreas, indicating the presence of a mass. (Figure 1) below demonstrates these findings; the arrow points to the pancreatic head mass.

Figure 1: Image showing a mass on the pancreatic head.
In addition to the mass, enlarged lymph nodes and lesions in the lungs, bone, and liver were visualized, concerning for metastases. RUQ U/S was conducted and showed a two cm mass on the liver, a distended gallbladder with wall thickening, possible sludge, and a dilated common bile duct without evidence of choledocholithiasis.
Findings were concerning for acute cholecystitis; therefore, the Gastroenterology department (GI) was consulted for an ERCP, and a HIDA scan was conducted to evaluate the gallbladder function. GI deferred performing the ERCP as he was not a candidate for surgical resection and it would not change the course of clinical management. HIDA Scan results showed a significantly reduced EF of 4%, indicating surgical management with laparoscopic cholecystectomy. The gallbladder was significantly massive during the operative procedure, with a gangrenous appearance. Due to the immense inflammation encountered, the surgeons converted the procedure from a laparoscopic to an open approach with a right upper quadrant kosher incision. The gallbladder was successfully removed and sent to pathology. The report showed chronic acalculous cholecystitis without biliary sludge and the presence of necrotic serosa with the perplexing finding of hemobilia. (Figure 2) shows gallbladder cell necrosis which gave it a gross gangrenous appearance. (Figure 3) shows blood in the gallbladder lumen.
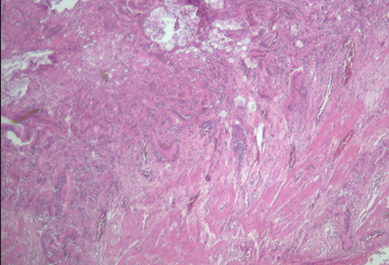
Figure 2: Necrotic biliary tissue on microscopy.

Figure 3: Image showing blood in the gallbladder lumen.
The diagnosis of his gallbladder disease was noted to be simultaneous Hemorrhagic and Gangrenous acalculous cholecystitis and was suspected to be a sequela of his pancreatic cancer. Oncology was consulted for this CT confirmed Stage 4 Pancreatic cancer, and the patient was scheduled to be sent to a palliative care facility. The patient subsequently passed away due to complications of his widespread disease.
Discussion
Gangrenous and Hemorrhagic Cholecystitis are both severe life-threatening conditions that are considered the final stages of disease in the spectrum of cholecystitis [6]. They usually appear as separate entities and have varying underlying etiologies; however, in this case of metastatic pancreatic cancer, both features were present, which was a perplexing finding. To our knowledge, this is the first case of gangrenous and hemorrhagic acalculous cholecystitis co-occurring and as a manifestation of pancreatic cancer. Metastatic pancreatic cancer is characterized by a pancreatic tumor with widespread lymphatic and organ involvement in areas such as the lungs, liver, bone, and biliary system, including the gallbladder [1]. Tobacco use and excessive alcohol intake are two of the most common risk factors [1]. Typically, patients develop cholelithiasis, acute calculous cholecystitis, and cholangitis in the setting of pancreatic cancer due to tumor compression of the bile ducts and subsequent stasis and infection of the biliary system [4]. However, there is a scarcity of literature on the incidence of hemorrhagic and gangrenous cholecystitis as a complication of pancreatic cancer.
Gangrenous cholecystitis is characterized by widespread necrosis of the gallbladder tissue and is caused by prolonged compression of the cystic duct and artery [7]. The most common contributing factors are the male sex, advanced age, and delayed surgery. The cystic artery is a branch of the right hepatic artery originating from the Superior Mesenteric Artery (SMA). It lies in the Calot triangle, bordered inferiorly by the cystic duct, and supplies blood to the gallbladder [8]. In pancreatic cancer, there is a high incidence of vascular invasion, with increased involvement of the SMA and its branches [9]. Persistent obstruction of the cystic duct and artery by metastasis can increase gallbladder wall tension and precipitate epithelial cell injury, which subsequently stimulates the release of phospholipases that mount a severe inflammatory response [7]. This inflammation and vascular insufficiency rapidly lead to tissue necrosis, accelerating gangrene formation.
Hemorrhagic Cholecystitis (HC) is characterized by bleeding into the gallbladder or biliary system (hemobilia) and is often due to trauma or anticoagulation use [5]. While there is a known association of HC in patients with chronic illnesses, a cohort study found that patients with cancer have a greater risk of developing complicated cholecystitis than the general population, with an even greater risk in patients over the age of 70 [7]. Gallbladder bleeding or HC can be secondarily caused by pancreatic cancer due to protease upregulation and activation and downregulation of protease inhibitors [10]. These active proteases invade and break down the blood vessel stroma and endothelium to allow malignant cell migration, resulting in bleeding and HC [10].
Common manifestations of gangrenous and hemorrhagic cholecystitis include tachycardia, chills, and fever in addition to the typical features of cholecystitis such as right upper abdominal pain that worsens on palpation, nausea, and vomiting [3]. These conditions are difficult to diagnose preoperatively. Laboratory results that increase the diagnostic suspicion for cholecystitis are elevated Liver Function Tests (LFT) and leukocytosis. Right Upper Quadrant Ultrasound (RUQ U/S) continues to be the first step in diagnostic imaging, which shows gallbladder wall thickening, indicative of cholecystitis [11]. There is some difficulty visualizing cholecystitis complications on U/S, so Computed Tomography (CT) is often used to make an early diagnosis [12]. Studies show that early cholecystectomy is effective and can lower the mortality of cholecystitis [13]. As previously stated, in this patient’s case, the U/S showed gallbladder distension with wall thickening and dilation of the common bile duct indicating blockage by the pancreatic mass. However, the presence of this mass ultimately led to extensive damage to the gallbladder by blocking its cystic and common bile outflow as well as eroding its arterial supply, which caused simultaneous gangrene and hemobilia.
This case discovers how late-stage pancreatic cancer can lead to acalculous cholecystitis, progressing to gangrenous and hemorrhagic cholecystitis over time, especially in the event of delayed treatment. A high degree of clinical suspicion is required in the setting of RUQ pain with the positive finding of pancreatic malignancy to prevent the development of gangrene and hemorrhagic bile formation. Management with emergent cholecystectomy is paramount to prevent a fatal outcome.
Conclusion
Secondary gangrenous and hemorrhagic cholecystitis should be considered as possible clinical manifestations in patients with metastatic pancreatic carcinoma. Pancreatic carcinoma usually is asymptomatic with no paraneoplastic or other stand-out complications. The development of hemorrhagic and gangrenous cholecystitis are both challenging to diagnose; however, if clinically suspected in a patient with pancreatic cancer, it warrants prompt medical investigation. Incorporating a possible prophylactic cholecystectomy is an adequate treatment strategy when developing a care plan for a patient with pancreatic carcinoma.
Author Contributions
Shaniah Holder: Concept and Design of study, Acquisition of data, drafting article, revising article. Guarantor Author
De’jeau Pyfrom: Acquisition of data, drafting article, revising article
Ulochi Nwagwu: Concept and Design of study, intellectual content, revising article
Obinna Okolocha: Acquisition of data, drafting article, revising article
Joancy Archeval- Lao: Drafting article, revising article
Frederick Tiesenga: Final Approval, Intellectual Content, revising article
Informed Consent: A signed statement of informed consent was obtained for publication of the details of this case
Competeing Interests: None
Grant Information: None
References
- Mizrahi JD, Surana R, Valle JW, Shroff RT. Pancreatic cancer. Lancet, 2020; 395(10242): 2008-2020.
- Sohal DP, Mangu PB, Khorana AA, et al. Metastatic Pancreatic Cancer: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol, 2016; 34(23): 2784-2796.
- Acute Cholecystitis, 2022.
- Thomsen RW, Thomsen HF, Norgaard M, et al. Risk of cholecystitis in patients with cancer: a population-based cohort study in Denmark. Cancer, 2008; 113(12): 3410-3419.
- Leaning M. Surgical case report-acalculous hemorrhagic cholecystitis. J Surg Case Rep, 2021; 2021(3): rjab075
- Teranishi K, Murase M, Maeda M, et al. [A case of acute hemorrhagic gangrenous acalculous cholecystitis with bile peritonitis during anti-coagulant therapy after coronary-artery bypass grafting]. Nihon Kyobu Geka Gakkai Zasshi, 1993; 41(1): 83-87.
- Önder A, Kapan M, Ülger BV, et al. Gangrenous cholecystitis: mortality and risk factors. Int Surg, 2015; 100(2): 254-260.
- Kapoor V. Gallbladder Anatomy, 2022.
- Buchs NC, Chilcott M, Poletti PA, et al. Vascular invasion in pancreatic cancer: Imaging modalities, preoperative diagnosis and surgical management. World J Gastroenterol, 2010; 16(7): 818-831.
- Keleg S, Büchler P, Ludwig R, Büchler MW, Friess H. Invasion and metastasis in pancreatic cancer. Mol Cancer, 2003; 2: 14.
- Shirah BH, Shirah HA, Saleem MA, Chughtai MA, Elraghi MA, Shams ME. Predictive factors for gangrene complication in acute calculous cholecystitis. Annals of hepato-biliary-pancreatic surgery, 2019; 23(3): 228–233.
- Schiappacasse G, Soffia P, Silva C, Villacrés F. Computed tomography imaging of complications of acute cholecystitis. The Indian journal of radiology & imaging, 2018; 28(2): 195–199.
- Koti RS, Davidson CJ, Davidson BR. Surgical management of acute cholecystitis. Langenbecks Arch Surg, 2015; 400(4): 403-419.

