A Price Worth Paying: Lymphoma in a Crohn’s Disease Patient Treated with Azathioprine and Infliximab
Fatma F Elmijbri*, Sahar H Summad, Awad Magbri
Benghazi Medical Hospital, Benghazi, Libya and Marshfield Medical Centre-Weston, USA
Received Date: 12/01/2023; Published Date: 08/02/2023
*Corresponding author: Fatma F Elmijbri, Benghazi Medical Hospital, Benghazi, Libya and Marshfield Medical Centre-Weston, USA
Abstract
Malignancy in patients with Inflammatory Bowel Disease (IBD) is ranked second behind cardiovascular diseases as the leading cause of death. People with IBD are prone to develop a variety of extraintestinal malignancies, particularly lymphomas. Many of these malignancies are non-Hodgkin Lymphomas (NHL). Hodgkin Lymphoma (HL) is a rather uncommon lymphoproliferative condition to occur in IBD. To date, there have been just a few cases of HL in IBD patients reported in the literature.
Modern treatment regimen for CD has helped prevent enterectomy, intestinal perforation, or stenosis. Thiopurine is a proven maintenance therapy for CD, while Tumour Necrosis Factor (TNF) inhibitors are effective for remission induction and maintenance treatment. Despite the increased likelihood of malignancy associated with treating CD with these agents, the risk is worth the complications. As these patients require long-term treatment to keep the disease at bay.
Here we report a case of HL developing in a patient with Crohn’s disease being treated with both azathioprine and infliximab. The occurrence of HL in IBD patients should be considered a complication to therapy, especially if they are subjected to long-term treatment with these agents.
Keywords: Inflammatory bowel disease; non-Hodgkin’s lymphoma; Hodgkin’s Lymphoma; Infliximab; Azathioprine; Crohn’s disease; Ulcerative colitis
Introduction
Immunosuppressed individuals have a higher propensity of developing lymphoproliferative diseases, particularly non-Hodgkin’s lymphoma [1]. Patient with Crohn's Disease (CD) have been found to have a higher risk of developing lymphoma [2]. However, most lymphoma cases related to infliximab were of the hepatosplenic T-cell or the B-cell NHL. Infliximab is a chimeric IgG1 monoclonal antibody that exerts its action by binding to human tumour necrosis factor-a (TNF-a) [3-6].
Modern treatment regimen for CD may help prevent enterectomy, intestinal perforation, or stenosis. Thiopurine is a proven maintenance therapy for CD, while Tumour Necrosis Factor (TNF) inhibitors are effective for remission induction and maintenance treatment. Despite the increased likelihood of malignancy associated with treating CD with these agents, the risk is worth the complications. As these patients require long-term treatment to keep the disease at bay [7].
The FDA acknowledged that there is correlation between infliximab therapy and the development of lymphoma. The small number of lymphomas occurring in individuals with IBD treated with these agents made it impossible to confirm or refute the association with precise confidence [8].
We present a case of HL in a CD patient who was treated on a long-term basis with azathioprine and infliximab. The association of HL with the use of infliximab and azathioprine in this patient have been deduced based on circumstantial, chronological, and historical data.
Case Report
52-year-old lady, with CD on azathioprine and infliximab treatment, presented with progressive exertional dyspnoea for few weeks. The patient denies night sweats, weight loss, or fever. Physical examination was within normal limits except for hard fixed lymph nodes in the left cervical area and left axilla. No other superficial lymphadenopathy or organomegaly could be detected.
Subsequently, analysis of laboratory tests including complete blood count with differential, hepatic and renal function tests; Lactate Dehydrogenase (LDH); serum electrolytes; serology tests for Epstein-Barr Virus (EBV), and Cytomegalovirus (CMV), HIV, and inflammatory markers of Erythrocyte Sedimentation Rate (ESR), and C-Reactive Protein (CRP) confirm the diagnosis of CD. The chest X-ray and the CT of the chest were also provided below.
The biochemical results showed increased ESR and CRP as well as a neutrophilic leucocytosis of approximately 13,000/mcl. The chest X-ray showed a left mediastinal enlargement (Figure 1).
Computed Tomography of chest (provided), and abdomen (picture not provided): showed multiple pathologically enlarged supraclavicular, cervical, mediastinal and hilar lymphadenopathies in the right para tracheal, right trachea-bronchial, right hilar, subcarinal, and right broncho-pulmonary group. The CT of the upper abdominal, showed the presence of similarly enlarged porta hepatis and peri-pancreatic nodes, average size 10-26 mm with the same features as the mediastinal group (Figure 2).
Histopathology of cervical and axillary LNs is suspicious for lymphomatous neoplasm possibly Hodgkin’s lymphoma. The diagnosis is subsequently confirmed with immunohistochemistry as it was positive for CD30 in RS-Burg-like cells. The diagnosis is of atypical lymphoproliferative disease mirroring Hodgkin’s lymphoma.
PET scan was positive for multiple pathologically enlarged LNs. These LNs are seen bilaterally in upper and lower deep cervical LNs, left supra-clavicular LN, and bilateral mediastinal (peri-tracheal, retro-caval, sub-carinal) and right hilar LNs. Abdominal LNs (bilateral para-aortic and common iliac), are also seen (picture not provided).
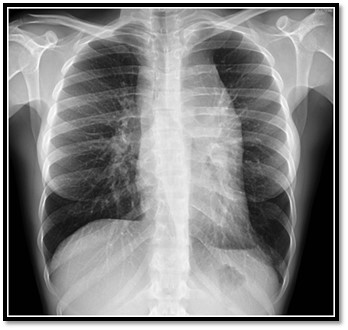
Figure 1: Chest X-ray showed a marked left mediastinal enlargement.
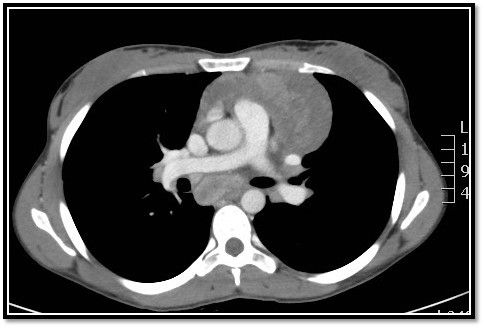
Figure 2: CT of the upper chest showed enlarged mediastinal hilar lymphadenopathies, right para tracheal, right trachea-bronchial, subcarinal, and right broncho-pulmonary group.
Discussion
The incidence of extra-intestinal HL in CD patient receiving long-term maintenance therapy with infliximab and azathioprine was rare in the literature. Most infliximab-associated lymphomas are hepatosplenic T-cell or B-cell non-Hodgkin’s types [3-6]. If infliximab is used with another immunosuppressive medication such as ciclosporin or methotrexate, the risk of lymphoma development increases many folds regardless of the underlying condition [4,5]. Biancone et al. [6] in a multi-centre study did not show any significant increase in the incidence of neoplasia in patients with CD treated with infliximab when compared with those who did not receive the drug [6].
As of December 1998, 12 clinical trials of infliximab had involved 913 patients (Jack McGowan, Centocor Inc., personal communication, December 1998) have been studied. Of the 771 patients who received the active drug, 6 patients treated with infliximab have developed lymphoproliferative disorders. Four of these cases (2 of B-cell non-Hodgkin’s Lymphoma [NHL], 1 of multiple myeloma, and 1 of Hodgkin’s disease [HD]) have been recorded. Four lymphoproliferative tumours occurred in patients with rheumatoid arthritis. The remaining 2-patients (1 with CD, 1 with Human Immunodeficiency Virus [HIV] infection) both developed B-cell NHL [8].
IBD are known to be linked to the development of lymphoma. Although literature reports so far implicated the occurrence of lymphoma to be more in Ulcerative Colitis (UC) than CD. Other reports have shown that CD patients can infrequently be associated with extra-intestinal HL, even without immunosuppressive therapy. Nevertheless, the use of immunosuppressive therapy in CD patients can considerably increase the incidence of lymphoma [9,10].
Another distinctive aspect of immunosuppression-associated lymphomas is the well-established link between many of these malignancies and oncogenic viruses like EBV and CMV infections. Which is not the case in our patient, as serology of both viruses were negative. Moreover, EBV-associated HL usually involves the colorectal region, and the small bowel, contrary to this patient, where HL occurrence was extra-intestinal [11-13].
Azathioprine is long been used in patients with CD to maintain remission and as a steroid-sparing medication. Long-term azathioprine usage has previously been connected to the development of reversible lymphoma in IBD patients [14,15]. Nevertheless, its advantages clearly outweigh the risk of lymphoma, justifying its use in IBD [16]. It must be determined whether the risk of developing HD increases with concomitant long-term usage of infliximab.
Back to our patient, Infliximab was stopped and Pentasa and azathioprine were continued. The patient was referred to Hem/Onc for further evaluation and management.
In conclusion, the occurrence of HL in patients with CD on long-term therapy with infliximab and azathioprine is rare. A higher index of suspicion and closer monitoring of patients who are on this therapy are needed to avoid the rare side-effects of these valuable armamentarium. We need to be vigilant and cognizant of this potential uncommon complication.
The authors have no financial disclosure.
References
- Beral V, Newton R. Overview of the epidemiology of immunodeficiency-associated cancers. J Natl Cancer Inst Monogr, 1998; (23): 1-6. doi:10.1093/OXFORDJOURNALS.JNCIMONOGRAPHS.A024164
- Lo B, Zhao M, Vind I, Burisch J. The Risk of Extraintestinal Cancer in Inflammatory Bowel Disease: A Systematic Review and Meta-analysis of Population-based Cohort Studies. Clin Gastroenterol Hepatol, 2021; 19(6): 1117-1138.e19. doi:10.1016/j.cgh.2020.08.015
- Zeidan A, Sham R, Shapiro J, Baratta A, Kouides P. Hepatosplenic T-cell lymphoma in a patient with Crohn’s disease who received infliximab therapy. Leuk Lymphoma, 2007; 48(7): 1410-1413. doi:10.1080/10428190701345433
- Bucher C, Degen L, Dirnhofer S, et al. Biologics in inflammatory disease: infliximab associated risk of lymphoma development. Gut, 2005; 54(5): 732. doi:10.1136/gut.2004.059352
- Mahé E, Descamps V, Grossin M, Fraitag S, Crickx B. CD30+ T-cell lymphoma in a patient with psoriasis treated with ciclosporin and infliximab. Br J Dermatol, 2003; 149(1): 170-173. doi:10.1046/J.1365-2133.2003.05384.X
- Biancone L, Orlando A, Kohn A, et al. Infliximab and newly diagnosed neoplasia in Crohn’s disease: a multicentre matched pair study. Gut, 2006; 55(2): 228. doi:10.1136/GUT.2005.075937
- Nakashima C, Tanioka M, Takahashi K, Miyachi Y. Diffuse large B-cell lymphoma in a patient with rheumatoid arthritis treated with infliximab and methotrexate. Clin Exp Dermatol, 2008; 33(4): 437-439. doi:10.1111/J.1365-2230.2007.02683.X
- Bickston SJ, Lichtenstein GR, Arseneau KO, Cohen RB, Cominelli F. The relationship between infliximab treatment and lymphoma in Crohn’s disease. Gastroenterology, 1999; 117(6): 1433-1437. doi:10.1016/S0016-5085(99)70294-5
- Musso M, Porretto F, Crescimanno A, BondÌ F, Polizzi V, Polizzi R. Crohn’s disease complicated by relapsed extranodal Hodgkin’s lymphoma: prolonged complete remission after unmanipulated PBPC autotransplant. Bone Marrow Transplant, 2000; 26(8): 921-923. doi:10.1038/SJ.BMT.1702621
- Palli D, Trallori G, Bagnoli S, et al. Hodgkin’s disease risk is increased in patients with ulcerative colitis. Gastroenterology, 2000; 119(3): 647-653. doi:10.1053/gast.2000.16487
- Wong NACS, Herbst H, Herrmann K, et al. Epstein-Barr virus infection in colorectal neoplasms associated with inflammatory bowel disease: detection of the virus in lymphomas but not in adenocarcinomas. J Pathol, 2003; 201(2): 312-318. doi:10.1002/PATH.1442
- Kumar R, Gandhi R. Reasons for cancellation of operation on the day of intended surgery in a multidisciplinary 500 bedded hospital. J Anaesthesiol Clin Pharmacol, 2012; 28(1): 66-69. doi:10.4103/0970-9185.92442
- Bai M, Katsanos K, Economou M, et al. Rectal Epstein-Barr virus-positive Hodgkin’s lymphoma in a patient with Crohn’s disease: case report and review of the literature. Scand J Gastroenterol, 2006; 41(7): 866-869. doi:10.1080/00365520500529629
- Connell WR, Kamm MA, Ritchie JK, Lennard-Jones JE, Dickson M, Balkwill AM. Long-term neoplasia risk after azathioprine treatment in inflammatory bowel disease. Lancet (London, England), 1994; 343(8908): 1249-1252. doi:10.1016/S0140-6736(94)92150-4
- Larvol L, Soule JC, Le Tourneau A. Reversible lymphoma in the setting of azathioprine therapy for Crohn’s disease. N Engl J Med, 1994; 331(13): 883-884. doi:10.1056/NEJM199409293311321
- Lewis JD, Schwartz JS, Lichtenstein GR. Azathioprine for maintenance of remission in Crohn’s disease: benefits outweigh the risk of lymphoma. Gastroenterology, 2000; 118(6): 1018-1024. doi:10.1016/S0016-5085(00)70353-2

