Invasive Mole Causing in Uterine Perforation, Case Report and Literature Review, 2022
Berhe Tesfai1,*, Okbu Frezgi1 and Dawit Sereke2
1Orotta College of Medicine and Health Science, Obstetrics and Gynecology, Post-Graduate, Ministry of Health, Eritrea
2Obstetrician and Gynecologist, Orotta National Referral Maternity Hospital, Ministry of Health, Eritrea
Received Date: 02/01/2023; Published Date: 27/01/2023
*Corresponding author: Berhe Tesfai (MD), Orotta College of Medicine and Health Science, Obstetrics and Gynecology, Post-Graduate, Ministry of Health, Eritrea
Abstract
Gestational trophoblastic neoplasia comprises a group of aggressive fertilization disorders characterized by invasion of the uterine endometrial and myometrial layers by malignant trophoblastic cells.
A 42 years gravida nine para eight mother from Ghedem, Massawa subzone of Eritrea, came with amenorrhea of four months; vaginal bleeding associated with passage of vesicular structures, dizziness and generalized body weakness of one week duration. She had pale conjunctiva non-icteric sclera; chest was clear to auscultation and had systolic ejection murmur. Abdomen was soft, symmetric and globular mass of fundal height of 18 weeks and fetal heart beat was not heard. Hemoglobin was 6.7g/dl and trans-abdominal ultrasonography of uterus revealed honey comb appearance and urine β-hCG titter was positive at > 1:4096. With the assessment of severe anemia and complete mole, she was admitted and transfused with 03 units of blood followed by suction evacuation and curettage. Post evacuation, another 2 units were given and discharged home with follow-up and oral contraceptive pills for three months. Unfortunately, she lost from follow-up and referred back from lower centers after 6 months with the same complaint. During re-admission her hemoglobin was 11.82g/dl, the ultrasonography revealed snow storm appearance with myometrial invasion and urine for β-hCG titter was positive at > 1:4096. With the assessment of persistent invasive mole, laparotomy with total abdominal hysterectomy was done and multiple uterine perforations with spilling vesicles were found. Pathology revealed invasive molar pregnancy of complete type and she was started on intravenous methotrexate alternated with leucoverine after 10 postoperative days. β-hCG titer on urine dipstick became negative after completing her first cycle of chemotherapy.
Invasive mole is highly sensitive to chemotherapy. She had typical clinical presentation and invasive mole succeeding complete molar pregnancy. Missing from follow-up paid her complications with uterine perforation. Patients should be counseled on adherence with post suction evacuation β-hCG surveillance to tackle the anticipated complications.
Key words: Persistent mole; Invasive mole; Gestational Trophoblastic Neoplasia
Introduction
Gestational Trophoblastic Disease (GTD) is a group of uncommon conditions associated with pregnancy. Histologically, it includes the premalignant partial hydatidiform mole (PHM) and complete hydatidiform mole (CHM), as well as the malignant invasive mole, choriocarcinoma, placental site trophoblastic tumor (PSTT), and epithelioid trophoblastic tumor (ETT) [1]. Invasive mole is a condition where the trophoblastic tumor invades the myometrium that may erode into the uterine vessels, causing massive intra-peritoneal hemorrhage [2].
Gestational choriocarcinoma arising from placental trophoblastic tissue is a malignant germ cell tumor that early metastasis to distant sites, especially to the lungs, liver, and brain, is quite common [3]. Invasive, metastatic GTD is very rarely seen in the emergency department, but it must be recognized and treated appropriately and immediately to prevent serious complications [4]. β-hCG is an excellent biomarker of disease progression, response, and subsequent post-treatment surveillance [1]. Thus, a plateaued or rising β-hCG level enables the early detection of progression of CHM and PHM to Gestational Trophoblastic Neoplasia (GTN) [1].
In order to monitor persistent GTN following evacuation in low-risk patients, β-hCG levels should be followed weekly until 3 consecutive normal values are obtained. It is also recommended to follow monthly β-hCG titer for six months after the level has turned normal [4]. Patients with low-risk GTN should be treated with one of the single agent methotrexates or actinomycin D [1]. Chemotherapy should be changed to the alternative single agent if there has been a good response to the first agent but the β-hCG level plateaus or rises during treatment, or if toxicity precludes an adequate dose or frequency of treatment. Multiple agent chemotherapy regimens are used to treat high-risk GTN [1].
Case Report
A 42 years gravida nine para eight married, housewife women from Ghedem, Massawa subzone of Eritrea, was referred to Orotta National Maternity Hospital on 22/04/2022 from massawa hospital with the assessment of molar pregnancy. The mother came with complaint of amenorrhea of four months with vaginal bleeding of one week duration. The vaginal bleeding was intermittent, pain less of clotted blood associated with passage of vesicular structures. She had also history of vomiting of ingested material which was not frequent, dizziness and generalized body weakness of one week duration. She denies any history of cough, epigastic pain, headache or lateralizing signs. She also denied history of previous miscarriages or molar pregnancy.
On physical examination, she was acutely sick looking not in respiratory distress. Her vital signs were: blood pressure of 90/60mmHg on right arm, semi-siting position, respiratory rate 18 breaths/minute, pulse rate 82 beats/minute right radial artery and temperature of 36.5oc in left axilla. She had pale conjunctiva and non-icteric sclera. Chest was clear to auscultation with systolic ejection murmur in all auscultatory areas of pericardium. Abdomen was soft and non-tender with symmetric and globular supra-pubic mass. Fundal height corresponds to 18 weeks and fetal heart beat was absent. On per-vaginal examination, cervix was open with blood on examining finger.
She was investigated with trans-abdominal ultrasonography, complete blood count and urine dipstick for β-HCG. Her hemoglobin was 6.7g/dl, hematocrit of 20.7% and platelet of 108x103. The ultrasonography revealed uterus filled with cystic structure with honey comb appearance without fetal parts. She was positive for β-hCG titter on urine dipstick at >1:4096. She was admitted to Orotta National Maternity Hospital with the diagnosis of molar pregnancy and was transfused with 05 units of blood. On the subsequent days, suction and evacuation was done under spinal anesthesia and vesicular structures with tissues and about 800ml of blood was evacuated. After 01 week stay in the hospital, she was discharged with regular weekly follow-up. The patient lost from follow-up and referred back to Orotta National Maternity Hospital on 26/10/2022 with same complaint and in similar condition.
On physical examination, she was sick looking, with vital signs of blood pressure of 90/50 mmHg in sitting position on right arm, pulse rate 104 beats/minute, respiratory rate of 24 breaths /minute and temperature of 36.1oC in left axilla. She had slightly pale conjunctiva, dry buccal mucosa and chest was clear to auscultation with good air entry bilaterally. The abdomen was soft with mild tenderness and shifting dullness. Uterus was palpable at 16 weeks of gestation which was firm and symmetrical in configuration. On per-vaginal examination, cervix admitted tip of finger and there was blood in examining finger. Her complete blood count result revealed hemoglobin of 11.82g/dl, hematocrit of 39.6% and platelet 382.2 x 103/μL. Trans-abdominal ultrasonography revealed snow storm appearance with involvement of myometrium and absent fetal parts. The urine β-hCG titter was positive at >1:4096. Peritoneal fluid cytology indicated active chronic inflammatory process.
She was investigated with ultrasound of abdomen, showed normal size, configuration and texture of liver, spleen, and both kidneys and chest x-ray didn’t show any metastasis. Renal function test and liver function test displayed normal finding. Gestational trophoblastic neoplasia was entertained and surgical management was decided. Under spinal anesthesia, midline incision done and 500ml of blood was evacuated. There were multiple perforations in the anterior and posterior wall of the uterus with spilling of vesicles through the perforation site to peritoneal cavity (Figure: 1a-1c). Total abdominal hysterectomy and bilateral salpingo-oopherectomy was done. There were no signs of distant metastasis to the liver and peritoneum. Intra-operatively, bleeding was minimal and sample was sent for pathology which revealed invasive molar pregnancy, complete type and secondary active chronic inflammation. She had improved clinically and at 10th day of post operation, she was started on single agent chemotherapy of methotrexate alternate with leucoverine was given for 5th day period of treatment. On her subsequent follow-ups, her β-hCG titter on urine dipstick become negative at 1:2.
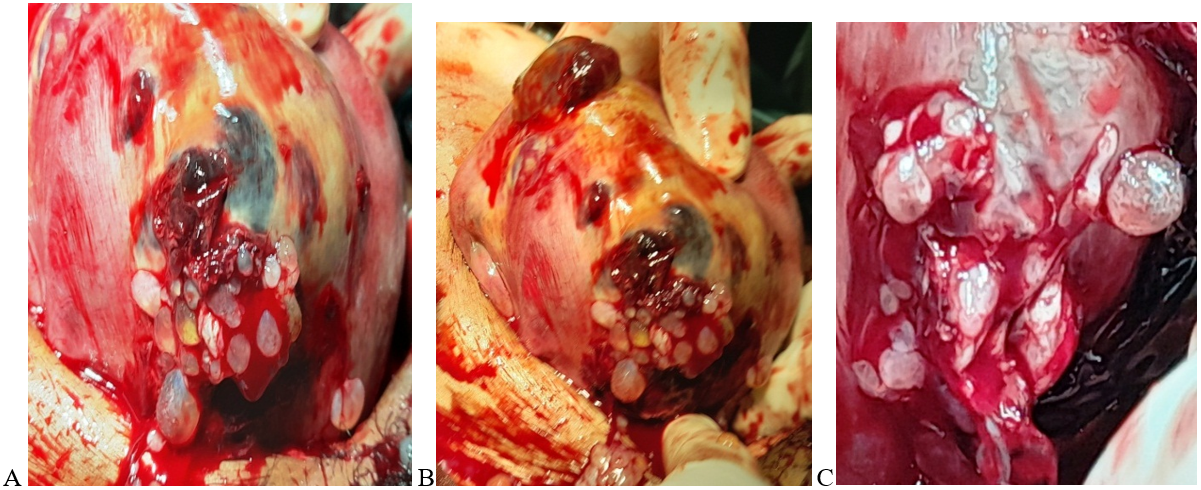
Figure 1: Anterior (A, B) and posterior (C) perforation of uterus with persistent invasive mole.
Discussion
The invasive mole had followed complete molar pregnancy. Similarly, different literatures reported that GTN most commonly develops following a complete hydatidiform molar pregnancy. [4, 5, 6] Therefore patients with molar pregnancy should have strict follow-up for serial β-hCG measurements and the clinical signs of invasive mole for early intervention. The pathology result also revealed invasive molar pregnancy of complete type which coincides with the clinical manifestations. Most invasive mole present with uterine perforation, but distant metastasis is the characteristics of adenocarcinoma. This case has no signs of metastasis to the lung and other organs.
She was lost from serial β-hCG measurement follow-up and her status after discharge was not documented. Finally, she came with invasive mole of uterine perforation. Even though literatures reported that monthly β-hCG levels should be checked for 6 months after the level has returned to zero because of the risk of persistent disease, [4] missing from follow-up tend to happen when a patient does not adhere to the strict follow-up regimen. [6] This could be mainly affected by many reasons; as patient’s awareness on the disease, socioeconomic and financial status, transportation and counseling on follow-up. She was financially poor, far from the treatment site and illiterate that could have an impact in her adherence to the strict weekly β-hCG follow-ups.
After suction and evacuation, she was lost from follow up and during her second visit, another pregnancy which could lead another molar pregnancy could be entertained. But she was on oral contraceptive pills for the first three months and the current problem lasts for two months that the possibility is low. And, as uterine wall during molar pregnancy is fragile, uterine perforation during suction and evacuation can happen in the first visits; but patient would have come early with all the complications like sepsis and bleeding.
As most patients with known molar pregnancy have regular β-hCG testing, those with malignant GTN are often diagnosed before symptoms occur or when repeat β-hCG levels are abnormal [4]. This also adds to the poor adherence of this case which resulted in the catastrophic complications of the persistent invasive mole. She had uterine perforation at the anterior and posterior myometrium with vesicles escaping and hemo-peritonium. This was consistent with other literatures that invasive GTN invades the myometrium or adjacent structures and can penetrate the uterus causing uterine rupture and hemo-peritoneum [2-4,6]. This indicated that if post suction curettage surveillance on β-hCG follow-up is not properly conducted, patient could be exposed to acute and chronic complications of the disease process due to delayed intervention.
Single agent chemotherapy was started after surgical management with hysterectomy. She had no signs of metastasis to the chest or other organs. Similarly, other studies reported that further evaluation didn’t show occult metastatic disease and the patient was treated with
single agent chemotherapy [6].Patients with low-risk GTN should be treated with one of the single agent methotrexates or actinomycin D [1]. Although an invasive mole is sensitive to chemotherapy and is highly curable, delayed treatment has been associated with serious complications, such as uterine perforation and hemo-peritoneum [5,7].
During her first admission, the FIGO scoring of GTN to this mother without serum β-hCG level was 4, which categorize her to low-risk group for which direct single agent chemotherapy was started. Since serum β-hCG level was not able to be determined in our setting, in which we use urine β-hCG titter which could affect the FIGO scoring result to start single agent chemotherapy. Multiple agent chemotherapy regimens are used to treat high-risk GTN [1]. This patient was classified as low-risk group of GTN with incomplete scoring, and multiple agent chemotherapy regimens were preferable if serum β-hCG level was determined. After completing her first cycle of chemotherapy, the urine β-hCG level dropped but still was weak positive. Studies indicated that the ß–hCG level gradually declined and became zero [6]. This can indicate the effect of the FIGO scoring using serum β-hCG level and type of chemotherapy.
As she had completed her family, hysterectomy with prophylactic chemotherapy was better treatment option for her at the initial presentation to prevent the above-mentioned complications. Direct hysterectomy is an alternative to suction and evacuation if childbearing is completed, age > 40 years and markedly elevated β-hCG. Hysterectomy can decrease GTN risk and limit the number of chemotherapies required. Our patient misses this chance of direct hysterectomy as she was not able to decide without her husband, who was not around during her first visit.
Conclusion
She had invasive mole following complete molar pregnancy and the pathology result coincides with the clinical manifestations. Invasive mole is highly sensitive to chemotherapy. Missing from follow-up paid her complications with uterine perforation and hemoperitoneum. She had good response to the surgical and chemotherapy management. Health professionals should have good knowledge on the atypical clinical presentation and adverse outcomes. Thus, patients should be counseled on adherence with post suction evacuation β-hCG surveillance to tackle the anticipated complications as soon as possible.
Declarations
Acknowledgment: authors acknowledge for the patients, pathology and chemotherapy departments in cooperation for the management of this patient.
Competing of interest: authors declare that they have no any conflict of interest to disclose
Funding: this case report had no any source of funding
Consent: a written informed consent was obtained from the patient to present and publish as case report
Data availability statement: Data is available as request form the corresponding author
Author’s contribution: BT, OF and MB had contributed in case writing and analysis
References
- Hextan YS, NganMichael J, SecklRoss S, Berkowitz Yang Xiang. Diagnosis and management of gestational trophoblastic disease: 2021 update. International Journal of Gynecology & Obstetrics, Figo cancer report, 2021; 155(S1): 86-93.
- Renuka Jindal, Sujata Sharma, Upasna Oberoi. A Rare Case of Invasive Mole with Silent Uterine Perforation- A Case Report, Journal of medical science and clinical research, 2015; 3.
- Chuan Xie, Lan Zheng, Zheng-Yu, Li Xia Zhao. Spontaneous Uterine Perforation of Choriocarcinoma with Negative Beta-Human Chorionic Gonadotropin after Chemotherapy. Med Princ Pract, 2011; 20: 570–573.
- David I, Bruner Amy M, Pritchard DO, Jonathan Clarke. Uterine Rupture Due to Invasive Metastatic Gestational Trophoblastic Neoplasm. West J Emerg Med, 2013; 14(5): 444–447.
- Wu A, Zhu Q, Tan C, Chen L, Tao Y. Invasive Mole Resulting in Uterine Rupture: A Case Report. Front. Surg, 2022; 8: 798640. doi: 10.3389/fsurg.2021.798640
- Yaghmaei M. Uterine perforation due to invasive mole: a case report. Zahedan J Res Med Sci, 2005; 7(4): e94920.
- Bram Pradipta, Andrijono Andrijono. Uterine Perforation on Invasive Hydatidiform Mole during EMACO Treatment. Indonesian Journal of Obstetrics and Gynecology, 2014; 2(3).

