Inguinal Bladder Hernia
Chadli A, Safwate R*, Daghdagh Y, Dakir M, Debbagh A and Aboutaeib R
Department of Urology, IBN Rochd University Hospital Center, Morocco
Received Date: 22/12/2022; Published Date: 16/01/2023
*Corresponding author: Safwate Reda, Department of Urology, IBN Rochd University Hospital Center, Morocco
Introduction
Inguinal hernia is a frequent pathology in surgery, it corresponds to the passage of abdominal or pelvic contents through the inguinal orifice. We speak of inguinal bladder hernia (IBH) when the contents concern the bladder, it is an uncommon entity and occurs most often in subjects over 50 years old. It is encountered in 1 to 4% of inguinal hernias, however its frequency increases to 10% after the age of 50 [1]. We report the case of a 40-year-old obese patient diagnosed with IBH preoperatively.
Report Box
This is a 40-year-old patient, without comorbidities, never operated, who presented with a left inguinal swelling 1 year before his admission to the urology department. The patient reported a progressive increase of a left inguinal tumefaction, which disappeared in dorsal decubitus, reproducible with the cough effort, reducible, with a sensation of incomplete bladder emptying made in 2 steps, the second step corresponds to a urination after compressing the hernial content. However, the patient did not report any lower urinary tract disorders preceding the appearance of the hernia, nor any factors increasing abdominal pressure, in particular no cough or chronic constipation. The clinical examination found a patient with normal vital signs, obese with a BMI of 37.8 kg/m², a left inguinoscrotal hernia and testicles of normal size and consistency with no nodule on palpation.
A radiological investigation was performed, the ultrasound revealed a left hernia with fluid content without evidence of a communication with the bladder which was in contact with the deep inguinal orifice. A retrograde urethrocystography showed a bladder of normal capacity with passage of a left bladder portion into the scrotum during micturition without evidence of a diverticulum (Figure 1). A uroscanner confirmed the diagnosis of HIV with the presence of a left inguinal parietal defect whose neck measures 30 mm in diameter with the passage of fat content and the anterosuperior part of the bladder through it (Figure 2).
After checking that there was no obstructive cause, the patient underwent an open hernia repair, which consisted of a bladder reduction with repair of the parietal defect after placing a bladder catheter at the beginning of the procedure. The postoperative course was simple and the patient was referred to a nutritionist for managing his obesity.
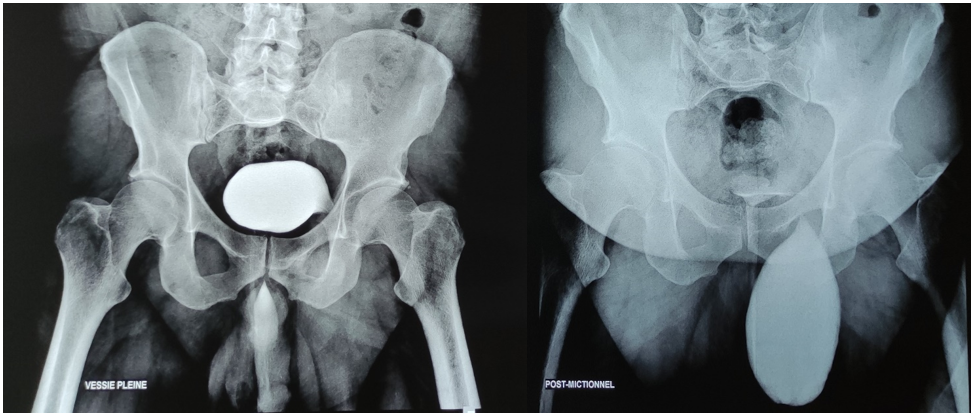
Figure 1: Retrograde cystography revealing a bladder of small capacity with an extension at the level of the left hernial orifice with scrotal opacification in post miction.
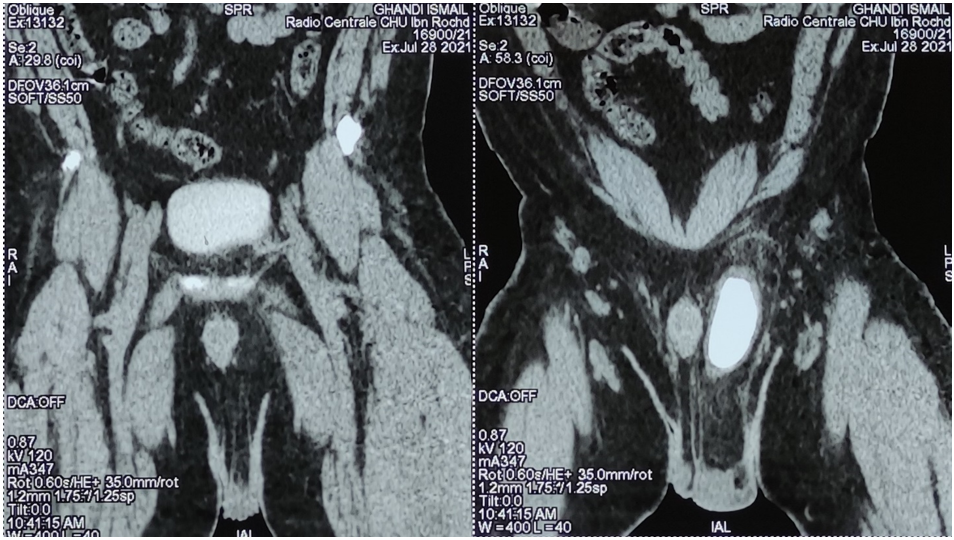
Figure 2: Late-stage CT scan showing part of the bladder entering the left inguinal opening.
Discussion
IBH is a rare entity, it is encountered in 1 to 4% of inguinoscrotal hernias. It is the result of the association of an increase in abdominal pressure with muscular weakness caused most often by obesity, which is the case in our patient. Several factors are involved in the pathophysiological processes of bladder hernias, such as subbladder obstruction caused by benign prostatic hyperplasia, bladder neck strictures and urethral strictures. After the age of 50, bladder tone decreases and the pelvic musculature weakens which increases its mobility. There may also be changes in the structure of the bladder due to increased bladder pressure, previous surgery, or local trauma [2].
IBH is classified according to the relationship of the bladder to the peritoneum. In the intraperitoneal type, the bladder is entirely contained within the peritoneal sac. In paraperitoneal type, the herniated bladder is covered by a peritoneal sac on one side only and is not contained within it. The third type is the extraperitoneal type, in which the peritoneum does not cover the bladder. The most common type is the paraperitoneal type, and the less common is the extraperitoneal type [3,4].
Clinically, IBH can be asymptomatic and be discovered intraoperatively, it can involve a bladder horn, a diverticulum or even the whole bladder. It is responsible for a symptomatology ranging from a simple irritative syndrome to acute obstructive renal failure. Depending on the size and content of the hernia, IBH can manifest itself as low urinary tract disorders such as dysuria, nocturia, and hematuria, which may or may not be associated with supra-pubic abdominal pain. The most specific sign is the Mery sign which includes a two-stage miction, the first step is spontaneous, the second step is done after compression of the herniated bladder. Other signs related to subbladder obstruction or urinary tract infection may be associated. When the diagnosis is not made preoperatively or when the hernia sac is opened during the procedure, the patient may present in the postoperative period hematuria, a parietal infection or a vesico-cutaneous fistula, extending the length of the operative stay and requiring a bladder catheterization which may be complicated by iatrogenic stenosis of the urethra [5-8].
Imaging modalities include ultrasound, intravenous urography, uroscanner, and sometimes MRI [1]. Ultrasound diagnosis is based on the finding of an intrascrotal fluid image that can be followed cranially to see its junction with the intra-abdominal portion of the bladder, as well as visualizing an anechogenic lesion that extends from the bladder into the inguinal canal or scrotum. Emptying of the scrotal cystocele after voiding is suggestive of the diagnosis [9]. Intravenous urography may show a rounded protrusion of the bladder wall directed downward. Reardon and Lowman described a triad for the diagnosis of IBH, involving lateral displacement of the distal third of the ureter, an asymmetric small bladder, and incomplete visualization of the bladder [10]. Nevertheless, retrograde cystography is the optimal examination to perform because it is easy to perform, does not expose the patient to potential danger and has good diagnostic reliability [2]. CT scan can reveal the sign of a herniated bladder with orientation of the bladder to the side of the hernia.
Like all hernias, IBH can strangle and be responsible for infarction and ischemia of the bladder wall. The most frequent complications are urinary tract infection and urinary lithiasis. Unilateral or bilateral ureterohydronephrosis with renal insufficiency, development of diverticula and the occurrence of intra hernial bladder tumor are possible but not common [6-8].
The standard treatment is surgical repair with reduction of the herniated bladder followed by herniorrhaphy. It is important to be aware of this diagnosis, because apart from situations that suggest HIV, herniorrhaphy can lead to iatrogenic bladder injury [5]. Bladder resection should only be performed in a few specific cases; in case of necrosis of the bladder wall, a large herniated diverticulum, a tight hernial neck, a bladder perforation that is difficult to repair or a tumor in the herniated bladder. Preservation of bladder capacity should be considered during bladder wall resection [6,11]. Although laparoscopic repair has advantages such as less postoperative pain and early recovery, serious complications such as vascular or organ damage are more common than with open surgery [12]. A measure that may seem simple and harmless and would avoid intraoperative injury is bladder catheterization to obtain a decrease in scrotal size [6]. Treatment of the obstructive cause should be considered before or at the same time as treatment of the hernia, because persistent dysuria carries the risk of recurrence [8].
Conclusion
IBH is an uncommon condition with an increasing prevalence over the age of 50. The risk factors are weakness of the muscle wall and increased abdominal pressure. The most suggestive clinical sign is Mery sign which corresponds to spontaneous voiding completed by compression of the hernial contents. The most optimal examination to perform is retrograde cystography. The treatment is essentially surgical and corresponds to a reduction of the herniated bladder with a repair of the abdominal wall.
References
- Hl She, Kc Lam, Kk Wong, et Wendy WM Lam. Department of Radiology, Queen Mary Hospital, Pokfulam, Hong Kong. « Urinary Bladder Inguinal Hernia: An Uncommon Cause of Scrotal Swelling ». Hong Kong Medical Journal 20, no, 2014; 4: 351.e1-351.e2.
- Moufid, Kamal, Driss Touiti, et Lezrek Mohamed. « Inguinal Bladder Hernia: Four Case Analyses ». Reviews in Urology 15, no, 2013; 1: 3236.
- Levine B. Scrotal cystocele. JAMA, 1951; 147(15): 22–24.
- Bjurlin MA, DeLaurentis DA, Jordan MD, et HM Richter. « Clinical and Radiographic Findings of a Sliding Inguinoscrotal Hernia Containing the Urinary Bladder ». Hernia 14, no, 2010; 6: 63538.
- Vindlacheruvu RR, Zayyan K, Burgess NA, Wharton SB, Dunn DC. Extensive bladder infarction in a strangulated inguinal hernia. Br J Urol, 1996; 77: 926-927.
- Gonzalez-Urquijo M, Mayagoitia-Gonzalez JC, Rodarte-Shade M, Bermea-Mendoza JH, et G. Gil-Galindo. « Large Inguinal Bladder Hernias: Can a Preoperative Diagnosis Be Made? » Hernia 23, no, 2019; 6: 122127.
- Sarr Alioune, Cyrille Ze Ondo, Yaya Sow, Boubacar Fall, Amath Thiam, Babacar sine, et al. "Inguinal hernia of the bladder: about 8 cases". Pan African Medical Journal, 2015.
- El Anzaoui, J., Y. El Harrech, N. Abbaka, D. Touiti, M. Lahkim, J. Fassi Fihri, W. Bakzaza, M. Majdane, and A. Achour. "Inguinal or bladder hernia?" Canadian Urological Association Journal, 2013; 7(1112): 837.
- Bacigalupo LE, Bertolotto M, Barbiera F, Pavlica P, Lagalla R, Mucelli RSP, et al. Imaging of urinary bladder hernias. Am J Roentgenol, 2005; 184: 546–551.
- Reardon JV, Lowman RM. Massive herniation of the bladder: “the roentgen findings”. J Urol, 1967; 97(6): 1019–1020.
- Tazaki Tatsuya, Masaru Sasaki, Mohei Kohyama, Yoichi Sugiyama, Shinnosuke Uegami, Ryuta Shintakuya, et al. « Inguinoscrotal Hernia Containing the Urinary Bladder Successfully Repaired Using Laparoscopic Transabdominal Preperitoneal Repair Technique: A Case Report ». Asian Journal of Endoscopic Surgery 12, no, 2019; 2: 2013.

