Caroli Disease with Autosomal Dominant Polycystic Kidney Disease in Kidney Transplant Patient
Rania Afifi*, Soukaina Rostoum, Ghislaine Medkouri, Naoufal Mtioui, Selma Elkhayat, Mohamed Zamd, Benyouns Ramdani, Mohamed Benghanem
Department of Nephrology, University Hospital Center IbnRochd Casablanca, Morocco
Received Date: 19/12/2022; Published Date: 09/01/2023
*Corresponding author: Rania Afifi, Department of Nephrology, University Hospital Center IbnRochd Casablanca, Morocco
Abstract
Both Caroli Disease (CD) and Autosomal recessive polycystic kidney disease “ARPKD” are rare autosomal recessive disorders, and both are claimed to be related to mutations in polycystic kidney and hepatic disease (PKHD1) [1] (i.e., the only pathogenic gene currently known)
The common cause of those two diseases is the expression of the same gene mutation in different parts of the liver and kidney to differing degrees.
This is a diagnostic and therapeutic emergency which need an adequate care, in order to reduce morbidity also possibly prolong both graft and patient survival.
We present a case of Caroli Disease with autosomal dominant polycystic kidney disease.
Keywords: Caroli disease; Autosomal dominant polycystic kidney disease; Kidney transplantation; Autosomal recessive polycystic kidney disease
Introduction
Polycystic Kidney Disease (PKD) is a genetic disorder leading to end-stage renal disease more commonly in the fourth to sixth decades of life. Cyst formations in the kidneys and other organs such as the liver and pancreas are the main characteristic of this disease. A significant number of patients with PKD undergo kidney transplantation and receive significant immunosuppression, predisposing them to comorbidities such as infections and malignancies [2].
Caroli's syndrome is a rare congenital disorder characterized by dilation of intrahepatic bile ducts and hepatic fibrosis, while Caroli's disease is a condition where there is only intrahepatic bile duct dilation without any fibrosis [3].
Caroli’s disease or syndrome is a condition that has rarely been associated with polycystic kidney disease even more rarely it has been described in patients with the autosomal dominant genotype (ADPKD).
We herein present a rare case of a patient with autosomal dominant polycystic kidney disease who underwent kidney transplantation and was eventually diagnosed with Caroli disease.
Case Report
We report the case of 60 years old male presented to our department with complaints of abdominal pain and jaundice for 2 weeks, with fever these symptoms were progressively increasing with a clinical cholestasis: dark urine, discolored tools for which the patient received intra venous antibio-therapy: cephalosporin and metronidazole.
In his medical history we found a kidney transplant in 2010 (from an apparent living donor her sister) with autosomal dominant polycystic ADPKD, then he underwent a cholecystectomy in 2018.
At the time of admission, he was alert and oriented, his temperature and blood pressure were 36.7, 13/8 respectively.
The rest of physical examination was unremarkable.
A laboratory evaluation revealed the following results: Total Bilirubin: 185 mg/l, Direct bilirubin: 135 mg/l, Indirect Bilirubin: 50 mg/l, Alkalinephosphatase: 309 IU/l Gamma glutamyl transferase: 405 IU/l,AST: 75 IU/l,ALT: 118 IU/l CRP: 71 mg/l.Serologies for hepatitis B, C and E were negative. CA19.9: 400UI/L
CRP: 77.3 mg/lProcalcitonin: 0.5ng/ml
Ultrasound of the liver revealed dilated intra hepaticbiliarytree, and BILI RMI showed multiple cystic formation evoking a Caroli syndrome with multiple stones within main biliary duct tree (Figure 1)
Due to the worsening clinical and biological symptoms , in particular worsening jaundice and increasing total bilirubin >250mg/l, direct bilirubin to >150 mg/l , Indirect bilirubin >100 mg/l (Table1), the patient underwent a oesophago gastroduodenoscopy which didn’t show abnormalities, including no esophageal or gastric varices, then an endoscopic retrograde cholangiopancreatography ERCP was performed under antibiotic protection ,showing a dilation of the intrahepatic bile ducts IHBD with the presence of multiple cystic formations of different sizes, some of which communicate with the IHBD in conclusion; it revealed an element in support of cholelithiasis or cholangiocarcinoma. (Figure 2)
The patient was scheduled for exploratory surgery, but he declined, a second ERCP was carried out to evacuate bile sludge, then the evolution was marked by a clinical-biological regression of the jaundice.
Table 1: Laboratory Data on Admission to the Hospital.
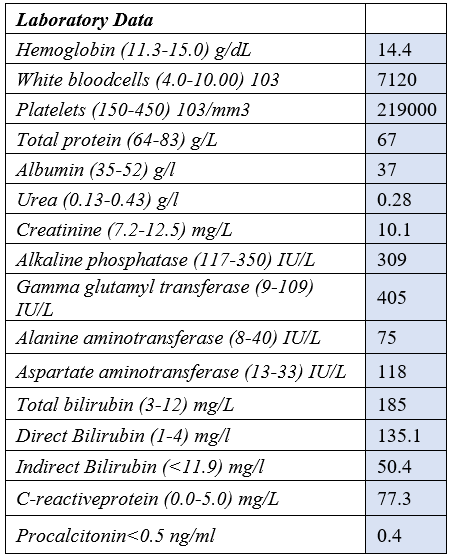
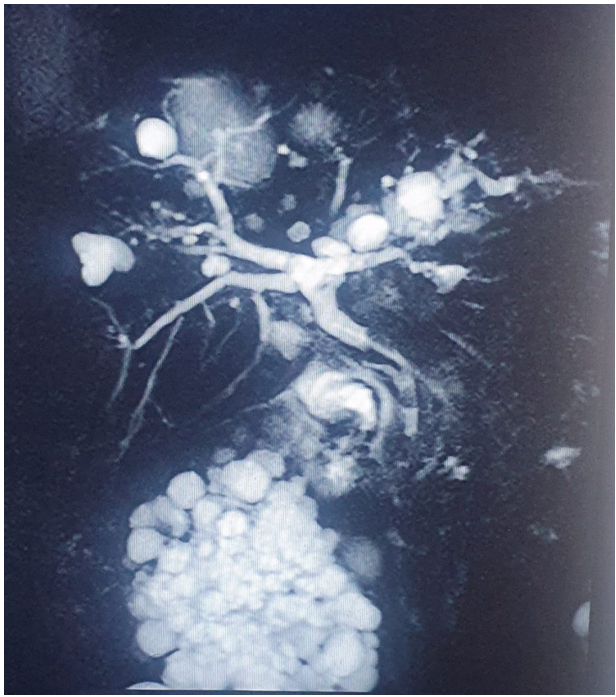
Figure 1: BILI-RMI.

Figure 2: ERCP.
Discussion
Caroli disease was first described in 1958 by Dr. Jacques Caroli, a French gastroenterologist who observed "nonobstructive saccular or fusiform multifocal segmental dilatation of the intrahepatic bile ducts." It is now known as a genetic disorder involving the PKHD1 gene (polycystic kidney and hepatic disease), which affects a protein called fibrocystin [4] this gene, is expressed in the fetal biliary system and is likely involved in the bile duct embryogenesis as part of its cell-cell or cell-matrix interactions [5] beside liver cholangiocytes it is also expressed in several organ systems: renal tubular cells, liver and the pancreas. Genetic abnormalities in this protein lead to fibrocystic changes in the kidneys and liver. Caroli disease is frequently seen with autosomal recessive polycystic kidney disease (ARPKD) [6] which is rarer than the most common type ADPKD characterized by progressive enlargement of the kidneys with multiple bilateral cysts and eventual loss of kidney function, often causing ESRD in middle age requiring kidney transplantation.
It is however, a multisystem disorder, with extrarenal manifestation such as polycystic liver, colonic diverticular disease, abdominal wall hernias, and pancreatic cysts [7].
However, some cases of ADPKD associated with Caroli syndrome have been reported such as our case.
To our knowledgeas very few such cases have been reported in literature, we were prompted to publish this case.
The exact numbers for its incidence and prevalence are not known as the condition is rare, but it is estimated to occur in approximately 1 in 1000,000 live births, with a female preponderance [8]. The clinical features of Caroli's disease are usually characterized by recurrent episodes of cholangitis [9] cholelithiasis, gallbladder abscess, jaundice and sepsis.Pruritis is also commonly reported, it is caused by hyperbilirubinemia from intrahepatic cholestasis.However, the esophagogastroduodenoscopy in our patient who was suffering from pruritis, revealed no abnormalities. In addition to that there is a high risk of cholangiocarcinoma in Caroli’s disease [10]; for this reason, tumor markers had a considerable interest, particularly ca19-9, which had shown high results in our case.
Imaging studies play a significant role in the diagnosis of Carolidisease. Ultrasonography is widely available and is often used first in the diagnosis [11] CT scans, ERCPs, MRCPs, and MRIs are also required to make a diagnosis [12].
Most of these tests were performed on our patient figure 1,2 inorder to allow us to make the diagnosis.
For our patient the ERCP revealed multiple saccular dilations within the intrahepatic biliary tree worsened by intrahepatic lithiasis.
The Mainstay of therapy is used as conservatory and can also be individualized according to the presentation
If the disease is localized to a segment or lobe in the liver, then a lobectomy may be considered. If the dilated bile ducts are located throughout the liver, antibiotics may be able to prevent cholangitis [12].
Patients with ADPKD who already received a kidney transplant, are more prone to Caroli disease in the post-transplant period, this may lead to a proper and more aggressive treatment of infectious cholangitis or even prophylactic antibiotic treatment to prevent recurrent infections [2].
The ERCP can help to remove an embedded stone by sphincterotomy and balloon scanning which was applied to our patient in the second ERCP to remove the sludge. As in Caroli disease, there is biliary stasis and sludge formation leading to obstruction of bile flow [4].
Liver transplant is the only cure for refractory or chronic cholangitis, liver failure or malignancy. Finally, a genetic investigation is crucial due to the fact that the disease can be autosomal recessive [13].
Medical treatment of CS includes antibiotics for cholangitis,ursodeoxycholic acid for cholestasis,beta blocker therapy and treatment of varices for portal hypertension [14]. Surgical treatment depends on the clinical features and the location of the biliary abnormalities. Segmental or lobar hepatic resection provides symptomatic relief and removes the risk of malignancy when the abnormalities are localized. In case of diffuse involvement of liver, treatment options include conservative management, endoscopic therapy (sphincterotomy for clearance of intra-hepatic stone), internal biliary bypass procedures and liver transplantation [15-18]. If concomitant renal failure ensues from the dysplastic kidneys, liver transplantation combined with renal transplantation might be warranted [19].
Genetic counselling and screening of family members is important is important as the disease should be best managed by an interprofessional team that includes a geneticist, gastroenterologist, liver specialist, urologist, nephrologist, radiologist, and transplant surgeon [20].
Conclusion
Caroli's disease is a rare biliary tract disease. The exact incidence of this disease is unknown because many cases are asymptomatic, causing the disease to be diagnosed later. This disease can strike at any age, but it is most common in adolescents and the elderly.
ARPKD is a genetically inherited kidney disease characterized by bilateral cystic kidney. It demonstrates a range of severity, with 30% dying early on and the majority having a good prognosis if they survive the first year of life.
The expression of the same gene mutation in different parts of the liver and kidney to varying degrees is the common cause of these two diseases.
This is a diagnostic and therapeutic emergency that requires immediate attention in order to reduce morbidity and possibly extend both graft and patient survival.
Conflicts of Interest: No
References
- Xiuzhen Yao, Weiqun Ao, Jianhua Fang, Guoqun Mao, Chuanghua Chen, Lifang Yu, et al. Imaging manifestations of Caroli disease with autosomal recessive polycystic kidney disease: a case report and literature review.
- Kumar A, Akselrod D, Prikis M. Caroli Disease Revisited: A Case of a Kidney Transplant Patient with Autosomal Polycystic Kidney Disease and Recurrent Episodes of Cholangitis Author links open overlay panel.
- Prasad Satish Kumar, Mehta Sameer Kumar, Poddar Ankit. A Rare Case of Caroli's Syndrome.
- Maladie de Caroli, Jalaluddin Umar, PujithaKudaravalli, Savio Jean. Dans: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021.
- Newby LJ, Streets AJ, Zhao Y, Harris PC, Ward CJ, Ong AC. Identification, characterization, and localization of a novel kidney polycystin-1-polycystin-2 complex. J Biol Chem, 2002; 277: 20763e7
- Sweeney WE, Avner ED. Polycystic Kidney Disease, Autosomal Recessive. In: Adam MP, Everman DB, Mirzaa GM, Pagon RA, Wallace SE, Bean LJH, Gripp KW, Amemiya A, editors. GeneReviews® [Internet]. University of Washington, Seattle; Seattle (WA): 2001.
- Parminder K Judge, Charlie HS Harper, Benjamin C Storey, Richard Haynes, Martin J Wilcock, Natalie Staplin, et al. Biliary Tract and Liver Complications in Polycystic Kidney Disease. J Am Soc Nephrol, 2017; 28(9): 2738–2748.
- Satish Kumar Prasad, Sameer Kumar Mehta, Ankit Poddar. A Rare Case of Caroli's Syndrome. Int J Appl Basic Med Res, 2021; 11(3): 195–197.
- Liang JJ, Kamath PS. Caroli syndrome. Mayo Clin Proc, 2013; 88: e59.
- Sato Y, Ren XS, Nakanuma Y. Caroli's disease: Current knowledge of its biliary pathogenesis obtained from an orthologous rat model. Int J Hepatol, 2012; 2012: 107945.
- William J Romano, John Karani. Caroli Disease Imaging, 2022
- Caroli Disease NORD gratefully acknowledges .Brittany A. Hodge, MMSc, NORD Editorial Intern from the Emory University Genetic Counseling Training Program and Cecelia A. Bellcross, PhD, MS, CGC, Associate Professor, Director, Genetic Counseling Training Program, Emory University School of Medicine, for assistance in the preparation of this report
- Satish Kumar Prasad, Sameer Kumar Mehta, et Ankit Poddar. Un cas rare de syndrome de Caroli (Caroli’s Syndrome with Autosomal Recessive Polycystic Kidney Disease Prithi Shenoy, Syed Ahmed Zaki, PreetiShanbag, Swapnil Bhongade Division of Pediatric Nephrology, Department of Pediatrics, Lokmanya Tilak Municipal General Hospital and Medical College, Sion, Mumbai, India).
- Alvarez Navascués R, Quiñones L, Guinea OF, Guerediaga F. Enfermedad de Caroli enpacienteportador de trasplante renal porpoliquistosis [Caroli disease in a kidney transplant patient with polycystic kidney disease]. Nefrologia, 2005; 25: 336e7.
- Bavikar R, Kulkarni R. Caroli’s syndrome: A case report. CurrPediatr Res, 2011; 15: 59-60.
- Gunay-Aygun M. Liver and kidney disease in ciliopathies. Am J Med Genet C Semin Med Genet 2009; 151C: 296-306.
- Yonem O, Bayraktar Y. Clinical characteristics of Caroli's syndrome. World J Gastroenterol 2007; 13: 1934-1937.
- Mrowka C, Adam G, Sieberth HG, Matern S. Caroli's syndrome associated with medullary sponge kidney and nephrocalcinosis. Nephrol Dial Transplant, 1996; 11: 1142-1145.
- Susan Shedda, Amanda Robertson. Caroli's syndrome and adult polycystic kidney disease. Affiliations expand, PMID: 17388839. DOI: 10.1111/j.1445-2197.2006.03659.x
- Karim AS. Caroli's disease. Indian Pediatr, 2004; 41: 848-850

