Trans-Vesical Migration of a Swallowed Needle with Intra-Urethral Impaction in a 12-Year-Old Boy
Aliyu S1 and Ningi AB2,*
1Department of Surgery, University of Maiduguri Teaching Hospital, Borno State, Nigeria
2Department of Surgery, Abubakar Tafawa-Balewa University Teaching Hospital, Bauchi State, Nigeria
Received Date: 18/11/2022; Published Date: 16/12/2022
*Corresponding author: Ningi Adamu Bala, Department of Surgery, Abubakar Tafawa-Balewa University Teaching Hospital, Bauchi State, Nigeria
Abstract
Foreign body, of whatever type, when ingested, either accidentally or intentionally, elicits strong reaction from care-givers, especially; if the victim is a child. Infants and children are the most commonly seen victims, ingestion is often intentional, unlike adults, who constitute a small proportion of victims and ingestion is often accidental. The number of foreign bodies found at the emergency units of many hospitals is quite large. These include coins, safety pins, sewing needles, button batteries and nuts. However, many of the foreign bodies are excreted safely without any untoward events, except for foreign bodies with sharp ends, containing toxic chemicals and where there is a pre-existing anatomical abnormality in the gastro-Intestinal Tract (GIT). Foreign bodies, especially those with sharp ends are prone to getting arrested, inflicting mucosal erosion or even perforating any part of the GIT, particularly at the site of physiologic or anatomic constrictions. These areas are the three Oesophageal anatomic narrowing, the pylorus, Ileo-Caecal valve and the recto-sigmoid junction. Most foreign bodies can be seen on plain radiograph, removal, where indicated, can be done endoscopically or through an open surgery. But, majority can be managed expectantly, aided by patience, careful serial radiographic monitoring and perhaps use of lubricating solutions like liquid paraffin.
Report of a transluminal migration is rare. We therefore report an unusual case of a trans-vesical migration of a swallowed sewing needle with intra-urethral impaction in a 12-year-old boy. The impacted needle was removed via an open Urethrotomy.
Keywords: Swallowed Needle; Trans-Vesical Migration; Intra-Urethral Impaction; Case Report
Introduction
Report of foreign body ingestion is common, due to infants that recognise objects by putting them in the mouth, a child intentionally swallowing an object, an adult accidentally ingesting or intentionally inserting a foreign material [1]. Foreign bodies within the Gastro-Intestinal or Respiratory tracts are a common cause of presentation at the emergency room (ER) globally. The mechanism of delivery to these tracts could be ingestion, aspiration, and deliberate insertion [1]. The United States of America (USA) National Hospital Ambulatory Medical Care Survey in 2010 reported approximately 535,000 cases of foreign body ingestion requiring treatment at the Emergency Unit [2].
Majority of swallowed foreign bodies are passed down the GIT without any complications, although a limited number present at the emergency department of various hospitals requiring urgent intervention [3]. The foreign bodies that are excreted out uneventfully are often asymptomatic, those not noticed by the caregivers of children or those in negligent or poor rural dwellers that attempt treatment at home [4]. Symptomatic victims of foreign body ingestion usually present at the Emergency Room and are likely to develop complications than the asymptomatic group [5]. The risk for complication is related to both the patient and the foreign body, most especially the foreign body. Apart from the normal site of anatomic narrowing in the alimentary tract, iatrogenic or post-traumatic stenosis in the GIT increase the risk of a foreign body getting stuck at such places and resulting in complications [6]. Foreign bodies with a soft end hardly erode or perforate the GIT, but those with a hard sharp edge can do so [7].
Reports of an extraluminal migration of foreign bodies are rare [8,9]. Few Authors have reported trans-luminal migration of pins, fish bones and other sharp objects in to the bladder, resulting in haematuria and recurrent urinary tract infections [10,11]. Intra-Vesical foreign bodies may get excreted out during micturition, get arrested within the urethra or remain in the bladder forming a nidus for stone formation [12]. No single report of trans-vesical migration of a needle with intra-urethral arrest was found on literature search. This informed our decision to publish this case report of a 12-year-old boy we managed with such presentation.
Case Report
A 12-year-old boy presented at the Surgical Out-Patient department of State Specialist Hospital Potiskum in Yobe State-Nigeria with an 11 months history of recurrent dysuria. The pain is said to be dull aching, usually at the end of micturition. There was also a 6 months history of intermittent total haematuria. No associated passage of clots in the urine, dizziness or syncope. There was no history of loin pain, pyuria, passage of stones in the urine and no family history of urolithiasis. He has been treated with multiple antibiotics as a case of recurrent urinary tract infection before presentation. He presented at our facility due to a sudden onset of sharp pain in the penile shaft, difficulty in passing urine and presence of an induration in the penile shaft. Patient is a professional traditional cap maker, usually adorned with exquisite embroidery using thread and needle. He recalled accidentally swallowing a needle he was using while holding it between his lips a year prior to presentation. He was asked by his colleagues to takes three gulps of locally made gruel and no medical treatment was sought for. He remained symptomless until a month after the incident when he started experiencing suprapubic discomfort and painful micturition.
On examination we were found to be in painful distress with a tender suprapubic swelling that is dull to percussion and surrounded by resonant percussion zones all around. A tender indurated cylindrical mass was felt in the dorsal aspect of the penile shaft. A well lubricated 16 Fr gauge foley’s catheter was passed to relieve the acute urinary obstruction and a urine sample was obtained for microbiological assessment. A plain abdominal radiograph revealed a slender, cylindrical, radio-opaque foreign body lodged in the penile urethra (Figure 1). The urine culture revealed Klebsiella pneumoniae and was appropriately treated based on the antibiogram. The patient and his parents were counselled on the possibility of trans-luminal migration of the previously swallowed needle and the need for its removal. An informed consent was obtained for Urethrotomy and foreign body removal.

Figure 1: Showing the intra urethral radio-opaque foreign body.
Procedure
After a spinal anaesthesia, patient was placed in a lithotomy position and the penile shaft was re-examined. The impacted foreign body became prominent (Figure 2). Urethrotomy was done via a dorsal incision and the impacted needle was exposed (Figure 3). The impacted needle was removed (Figure 4) and the urethral rent was repaired over a 16 Fr Foley’s catheter (Figure 5). A check pelvic radiograph was done the following day and it showed no foreign body (Figure 6). The urethral stent (catheter) was removed 14 days after the surgery and patient has been micturating freely with no lower urinary tract symptoms. He was scheduled to have a Retrograde Urethrogram at 3 months and 6 months after surgery to check for stenosis or fistulation.

Figure 2: Showing the impacted intra-urethral foreign body.

Figure 3: Showing the intra-urethral needle after urethrotomy.
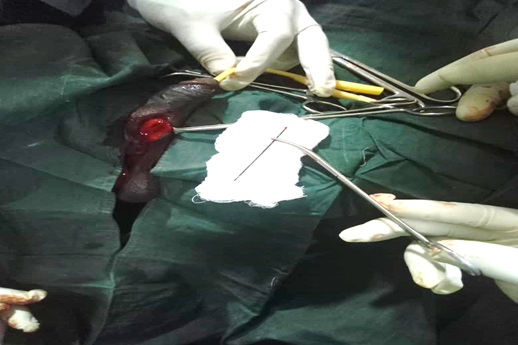
Figure 4: Showing the extracted needle following urethrotomy.

Figure 5: Showing the penile shaft after urethroplasty.

Figure 6: Showing a check pelvic radiograph a day after surgery with bo foreign body.
Discussion
Foreign body ingestion is a common cause of presentation at the surgical department worldwide. A report from the United States of America estimated that up to 1,500 mortalities are recorded annually due to foreign body ingestion [I3]. Children are the most common victims. Some reports estimated that as high as 80% of cases of foreign body ingestion are seen in young children [14,15]. The most commonly ingested materials in children are objects found in the house like coins, pins, nuts, pencils, batteries, nuts, toys and jewellery [15]. This is evident in our index patient, who is a 12-year-old boy and he swallowed a needle. Foreign body ingestion is rare and often accidental in adults and edentulous persons, majority are fish bones or meat bolus [13]. Intentional insertion of foreign bodies like spoons and tooth brushes is seen in psychiatric patients, while drugs and weapons like razor blades and other sharp objects are intentionally concealed in the rectum of prisoners and criminals [16,17,18,19]. A significant number of children that ingest a foreign body may remain asymptomatic, managed by caregivers at home or brought to the hospital for assessment of safety and assurance [20]. Those who are symptomatic may present at the Emergency Room with obvious symptoms of chocking, upper or lower gastro-intestinal tract obstruction [21]. Our patient fell in to the former group. He did not develop any gastro-intestinal symptoms in the aftermath of the ingestion up to a month and did not seek medical care. This may be due to the small size of the needle, perhaps, absence of pathological narrowing in the proximal part of the GIT.
Our patient swallowed a needle that is hard with a sharp end, yet, it passed through the small bowel successfully. The exact mechanism for such phenomenon is not fully understood. But some have opined that sharp objects tend to take a reverse position within the small intestine with the blunt end becoming the lead point and the sharp end following [17]. The Recto-Sigmoid junction is angulated and is said to be a common site of impaction and subsequent complications [22]. Complications from ingested sharp Foreign Bodies may include per rectal bleeding, perforation, or abscess. At presentation the patient might have forgotten the incident of the ingestion [22]. Trans-vesical migration of the swallowed needle in our patient occurred a month after ingestion. Trans-vesical migration of ingested foreign bodies has been reported previously [23], both sharp and blunt foreign bodies have been reported to cause such a complication [12,24,25,26]. Our literature search did not yield a report on trans-vesical migration of a needle with intra-urethral impaction. This unique presentation is what prompted our desire to publish this case report. Since there was no associated history of passage of stool or air in urine and no gastro-intestinal symptoms, we believe the site of the Recto-Vesical fistulation has healed. We will further re-assess the integrity of the bladder wall following the scheduled Retrograde Urethrogram at 3months and 6 months after the surgery.
Conclusion
It is difficult to predict the out-come of transition of an ingested foreign body, especially one with a pointed edge. If a patient ingests a sharp foreign object that is not excreted out in stool, any persistent lower urinary tract symptoms should raise the suspicion of a possible migration via a vesico-enteric fistula.
Acknowledgement: We appreciate the kindness of the patient and his caregivers that gave us the consent to publish his case.
Conflict of interest: None declared.
Authors’ participation: The first and the second Author managed the patient. The second Author wrote the case report and the first Author proofread and made correction on the manuscript.
References
- Hsiang-Jer T, Tarek NH, Waqas S, Majid A, Faisal K, Ken FL. Imaging Foreign Bodies: Ingested, Aspirated, and Inserted. Ann Emerg Med, 2015; 66: 570-582.
- Centre for Disease Control and Prevention. National Hospital Ambulatory Medical Care Survey: 2010 Emergency Department Summary Tables 2010.
- Conners GP. Pediatric Foreign Body Ingestion: Complications and Patient and Foreign Body Factors. Sci, 2022; 4: 20.
- Conners GP, Chamberlain JM, Weiner PR. Pediatric coin ingestions: A home-based survey. Am. J. Emerg. Med, 1995; 13: 638–640.
- Paul RI, Christoffel KK, Binns HJ, Jaffe DM. Foreign bodies in children: Risk of complication varies with site of initial health care contact. Pediatrics 1993; 91: 121–127.
- Louie JP, Alpern E, Windreich RM. Witnessed and unwitnessed esophageal foreign bodies in children. Pediatr. Emerg. Care 2005; 21: 582–585.
- Wright CC, Closson FT. Updates in pediatric gastrointestinal foreign bodies. Pediatr Clin North Am, 2013; 60: 1221-1239.
- Selivanov V, Sheldon GF, Cello JP, et al. Management of foreign body ingestion. Ann Surg, 1984; 199: 187–191.
- Braumann C, Goette O, Menenakos C, et al. Laparoscopic removal of ingested pin penetrating the gastric wall in an immunosuppressed patient. Surg Endosc, 2004;18:870.
- Carp L. Foreign bodies in the intestine. Ann Surg, 1927; 85: 575–591.
- Stricker T, Kellenberger CJ, Neuhaus TJ, et al. Ingested pins causing perforation. Arch Dis Child, 2001; 84: 165–166.
- Shailendra P, Anand P, Vipin G, Jigyasa P and Rajesh V. Presentation of an ingested foreign body as a vesical calculus: a common condition, but uncommon presentation. Ann Pediatr Surg, 13: 50–51. DOI: 10.1097/01.XPS.0000489162.87949.60.
- Kenton LA, Anthony JD. Foreign Bodies in the Gastrointestinal Tract and Anorectal Emergencies. Emerg Med Clin N Am, 2011; 29: 369–400. doi: 10.1016/j.emc.2011.01.009.
- Erbes J, Babbitt DP. Foreign bodies in the alimentary tract of infants and children. Appl Ther, 1965; 7(12): 1103–1109.
- Cheng W, Tam PK. Foreign-body ingestion in children: experience with 1,265 cases. J Pediatr Surg, 1999; 34(10): 1472–1476.
- Conway WC, Sugawa C, Ono H, et al. Upper GI foreign body: an adult urban emergency hospital experience. Surg Endosc, 2007; 21(3): 455–460.
- Webb WA. Management of foreign bodies of the upper gastrointestinal tract: update. Gastrointest Endosc, 1995; 41(1): 39–51.
- Lyons MF, Tsuchida AM. Foreign bodies of the gastrointestinal tract. Med Clin North Am, 1993; 77(5): 1101–1114.
- Brady PG. Esophageal foreign bodies. Gastroenterol Clin North Am, 1991; 20(4): 691–701.
- Arana A, Hauser B, Hachimi-Idrissi S, et al. Management of ingested foreign bodies in childhood and review of the literature. Eur J Pediatr, 2001; 160: 468–472.
- Chen MK, Beierle EA. Gastrointestinal foreign bodies. Pediatr Ann, 2001; 30: 736–742.
- Moreira CA, Wongpakdee S, Gennaro AR. A foreign body (chicken bone) in the rectum causing extensive perirectal and scrota1 abscess: report of a case. Dis Colon Rectum, 1975; 18(5): 407–409.
- Lyons MF, Tsuchida AM. Foreign bodies of the gastrointestinal tract. Med Clin North Am, 1993; 77(5): 1101–1114.
- Wagemakers S, Ibelings M. Colovesicular fistula after migration of a biliary stent. Ned Tijschr Geneeskd, 2011; 155: A3615.
- Garcia Lopez F, Lopez C, Nova Sanchez E, Fernandez Puentes JC, Llorens Martınez FJ, Vazquez Rojas JL, et al. An infrequent etiologic agent of vesico-intestinal fistula. Actas Urol Esp, 1989; 13: 454–456.
- Graziotti P, Maffezzini M, Candiano G, Maugeri O. Vesico-Enteric fistula created by ingested foreign body in Meckel’s diverticulum. J Urol, 2002; 168: 2547.

