Upper Urinary Tract Candida Albicans Fungal Ball Treatment with Continuous Nephrostomy Tube and Antegrade Fluconazole Instillation
Mohammed Al-Zubaidi1,*, Jeanie Misko2, Matthew DM Rawlins2, John R Dyer3, Steve McCombie1,4 and Dickon Hayne1,4
1Department of Urology, Fiona Stanley Hospital, Australia
2Department of Pharmacy, Fiona Stanley Hospital, Australia
3Department of Infectious Diseases, Fiona Stanley Hospital, Australia
4UWA Medical School, University of Western Australia, Australia
Received Date: 31/10/2022; Published Date: 14/11/2022
*Corresponding author: Mohammed Al-Zubaidi, Department of Urology, Fiona Stanley Hospital, Australia
Abstract
Urinary tract candida infections can be caused either by hematogenous dissemination of the organism or an ascending infection. Systemic treatment with antifungals is often challenging due to many antifungals achieving low concentrations in the urine. Herein, we report a case with sepsis from infected obstructed kidneys with Candida albicans fungal ball which was treated with a different approach of continuous antegrade fluconazole irrigation through percutaneous nephrostomy tubes bilaterally along with systemic administration of antifungals.
Keywords: Fungal ball; Candida albicans; Fluconazole; Nephrostomy
Introduction
Fungal urinary tract infections are generally uncommon in the community. However, it is more common in hospitals where 10 to 30% of urine cultures isolate Candida spp. Clinical features vary from asymptomatic urinary tract colonization (most common) to cystitis, pyelonephritis, or even severe sepsis with fungemia. Treatment is recommended only when funguria is symptomatic or in cases of fungal colonization with host factors that increase the risk of fungemia. Prevention of fungal infections is crucial, this can be achieved by better control of risk factors, including removing urinary catheters, limiting antibiotic treatment, and optimizing diabetes mellitus treatment [1].
Case Report
A 49-year-old male, with a background history of type 2 diabetes mellitus, was admitted to the hospital with bilateral infected obstructed kidneys and acute kidney injury. Non-contrast CT scan showed bilateral moderate to severe hydronephrosis with no obvious obstructive cause (Figure 1). Urine cultures grew C. albicans raising the possibility of obstructive uropathy secondary to fungal balls in the urinary tract. Blood tests showed White Cell Count (WBC) 18.62 x 109/L, C-Reactive Protein (CRP) 272 mg/L, serum creatinine 1070 micromol/L (Estimated Glomerular Filtration Rate [eGFR] of 4 mL/min/1.73m2), potassium 8.4 mmol/L, and Creatine Kinase (CK) level 2100 units/L. He was resuscitated in the emergency department as per CCrISP guidelines with intravenous fluids, calcium gluconate intravenously along with dextrose and insulin infusion to correct the potassium level. He was also treated with broad spectrum intravenous antibacterials. He was admitted to the intensive care unit for haemodynamic support and haemo-filtration. Urgent bilateral nephrostomy tubes were inserted to unblock the kidneys and control the infection source. Blood cultures confirmed Candida albicans fungaemia, which was treated initially with intravenous fluconazole (400mg daily) plus intravenous anidulafungin 200mg loading dose, followed by 100mg daily. The systemic therapy was rationalised after 5 days to fluconazole 400mg daily intravenously. Fluconazole instillation through the nephrostomy tubes was considered by the infectious diseases department due to persistent fever and poor infection source control in the urinary tract after excluding valvular vegetation and endophthalmitis in echocardiogram and formal ophthalmological review respectively. Fluconazole was infused continuously via the nephrostomy tubes on a rate of 40mL/hour (300mg fluconazole in 500mL sodium chloride 0.9%) with significant improvement within 3 days, White cell count was 5.72 x 109/L, CRP 42 mg/L, serum creatinine 79 micromol/L (eGFR >90 micromol/L/1.73m2) with resolved hydronephrosis in a CT urogram (image 2). Fluconazole infusion via nephrostomies continued for total of 6 days followed by removal of the nephrostomies. However, oral fluconazole was continued at 400mg once daily for total of 20 days until discharge due to concerns of poor compliance with medications. Patient remained well for 6 months after discharge.
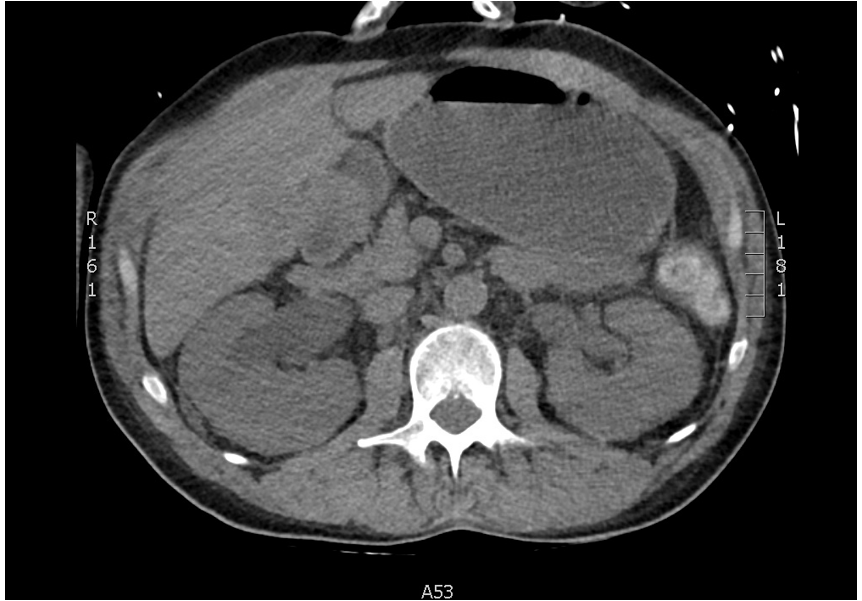
Figure 1: Non-contrast CT KUB showing bilateral hydronephrosis with no obvious cause of obstruction.
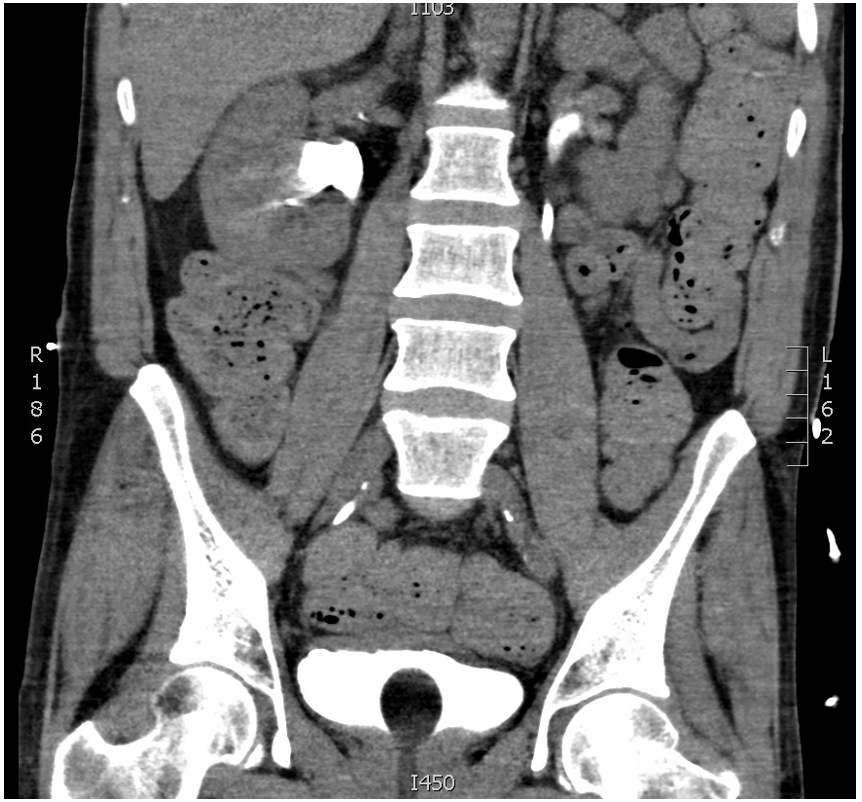
Figure 2: CT Urogram showing resolved hydronephrosis, no obstruction with contrast flow to bladder.
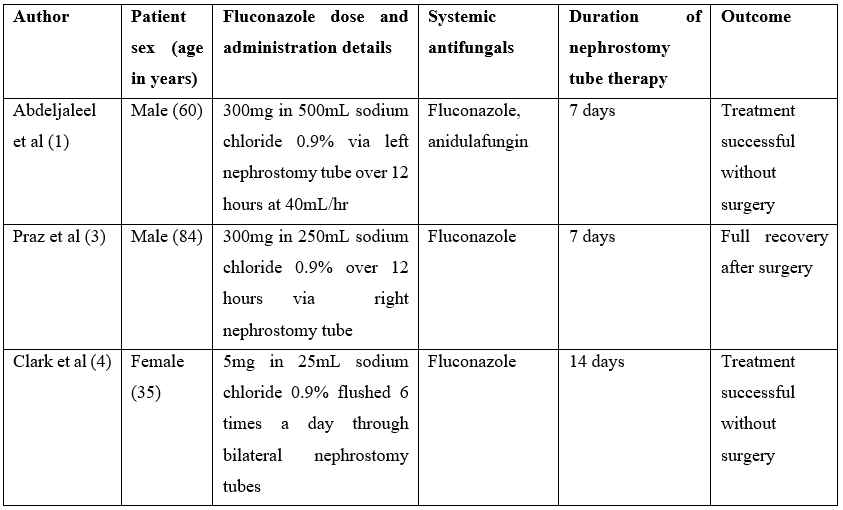
Table 1: Case reports in the literature utilising fluconazole via nephrostomy tube for C.albicans fungal ball.
Discussion
The Infectious Diseases Society of America (IDSA) Clinical Practice Guideline for the Management of Candidiasis 2016 recommends the use of amphotericin B deoxycholate irrigation via nephrostomy tube in combination with systemic antifungals for the management of C. albicans fungal ball. The recommendation for amphotericin B deoxycholate irrigation is based on low-quality evidence, [2] and , C. albicans is generally susceptible to fluconazole and antifungal resistance is relatively uncommon [2].
Published information on instillation of fluconazole via a nephrostomy tube is limited to case reports. Nephrostomy regimens reported to date have either been as 12 hour instillations within a 24 hour period, or using shorter intermittent doses to flush the nephrostomy tubes. Table 1 summarises these cases. Our hypothesis was that using a continuous nephrostomy irrigation of fluconazole may be more effective in treating the C. albicans fungal ball, avoiding the need for surgical intervention. The duration of the fluconazole irrigation used was similar to the previously reported regimens.
Anidulafungin has shown a trend towards improved outcomes and survival when used as the primary therapy for candidaemia due to C. albicans [2]. This was an appropriate choice for the patient as blood cultures were positive for C. albicans on admission to hospital. The oral fluconazole dose the patient received was in accordance with the IDSA guidelines [2]. Both blood and urine cultures were susceptible to anidulafungin and fluconazole.
Conclusion
Continuous instillation of fluconazole via nephrostomy tubes, in addition to systemic antifungal treatment, appeared to be effective treatment for C. albicans fungemia secondary to bilateral infected obstructed kidneys. These interventions helped to avoid the need for surgery in this patient.
References
- Abdeljaleel OA, Alnadhari I, Mahmoud S, Khachatryan G, Salah M, Ali O, et al. Treatment of Renal Fungal Ball with Fluconazole Instillation Through a Nephrostomy Tube: Case Report and Literature Review. Am J Case Rep, 2018; 19: 1179-1183.
- Pappas PG, Kauffman CA, Andes DR, Clancy CJ, Marr KA, Ostrosky-Zeichner L, et al. Clinical Practice Guideline for the Management of Candidiasis: 2016 Update by the Infectious Diseases Society of America. Clin Infect Dis, 2016; 62(4): e1-e50.
- Praz V, Burruni R, Meid F, Wisard M, Jichlinski P, Tawadros T. Fungus ball in the urinary tract: a rare entity. Can Urol Assoc J, 2014; 8(1-2): E118-E20.
- Clark MA, Gaunt T, Czachor JS. The use of fluconazole as a local irrigant for nephrostomy tubes. Mil Med, 1999; 164(3): 239-241.

