Non-Puerperal Uterine Inversion in Young Women
Etber A, Mahtate M, Cherradi S, Lakhdar A and Baidada A
Department of Gynecology-Obstetris and Endoscopy, Maternity SOUISSI/university hospital center Ibn Sina, Morocco
Received Date: 03/10/2022; Published Date: 28/10/2022
*Corresponding author: Etber Amina, Department of Gynecology-Obstetris and Endoscopy, Maternity SOUISSI/university hospital center Ibn Sina, Rabat, Morocco
Abstract
Non-puerperal uterine inversion is an extremely rare condition. it affects the young woman less frequently than the woman in periods of perimenopause and menopause. The causative pathology is frequently benign but could also be malignant. Uterine conservation for fertility purposes is the treatment of choice in young women, except in cases of malignancy.
We report the case of a young woman who presented with stage 3 uterine inversion secondary to a submucosal uterine fibroid.
Introduction
Uterine inversion is a pathology in which the fundus of the uterus turns inside out into or through the endometrial cavity or the cervix, subsequently the uterus may prolapse into the vagina or exteriorise to the vulva. It is a rare condition; puerperal uterine inversion, a pathology of delivery, is estimated at 1/3500 deliveries [1,18]. Non-puerperal or gynecological uterine inversion is even rarer: only 303 cases have been reported in the literature from 1911 to 2018 [4]; affecting more frequently women in the peri-menopausal and menopausal periods than young women. The possibility of a malignant cause should always be kept in mind in front of any uterine inversion.
Case Report
A 34-year-old female patient from Senegal Gravida 2 Para 2: 2 alive children delivered vaginally, admitted to the emergency department of our maternity hospital for a prolapsed mass through the vaginal cavity for one week following straining when urinating. The patient reported the externalization of the second mass the day before her admission following its attraction to the first one, and the associated symptomatology was chronic menometrorrhagia and pelvic pain. Her hemodynamic status was stable: BP =11 /06 pulse=90 beats/min, rectal temperature = 38.3. On gynecological examination, inspection revealed 2 rounded masses, the outermost one attached to the other mass by a pedicle, infected and externalized at the vulva, in front of which uterine inversion was not considered. The vagina was filled by the mass.
The ultrasound scan allowed us to diagnose uterine inversion. Her hemoglobin was 4g/dl. The patient was put on antibiotics and transfused in preparation for surgery. The treatment was an interannual hysterectomy by vaginal approach.
Final histology confirmed uterine inversion secondary to a submucosal uterine fibroid.
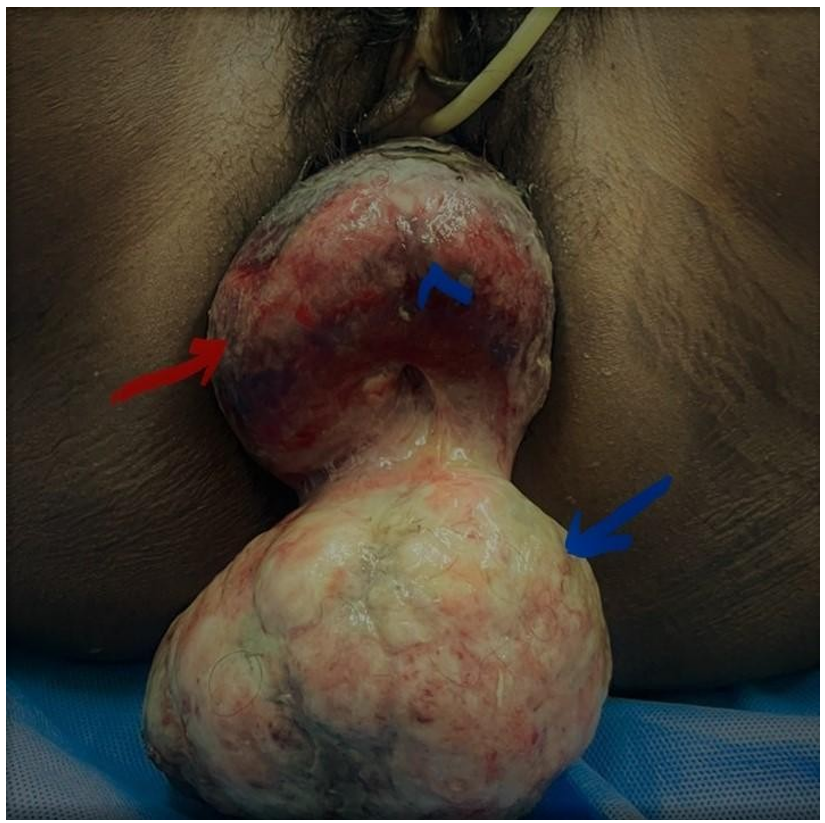
Figure 1:
→ inverted uterine fundus
→ pedunculated submucosal fibroma type 0
< endometrium
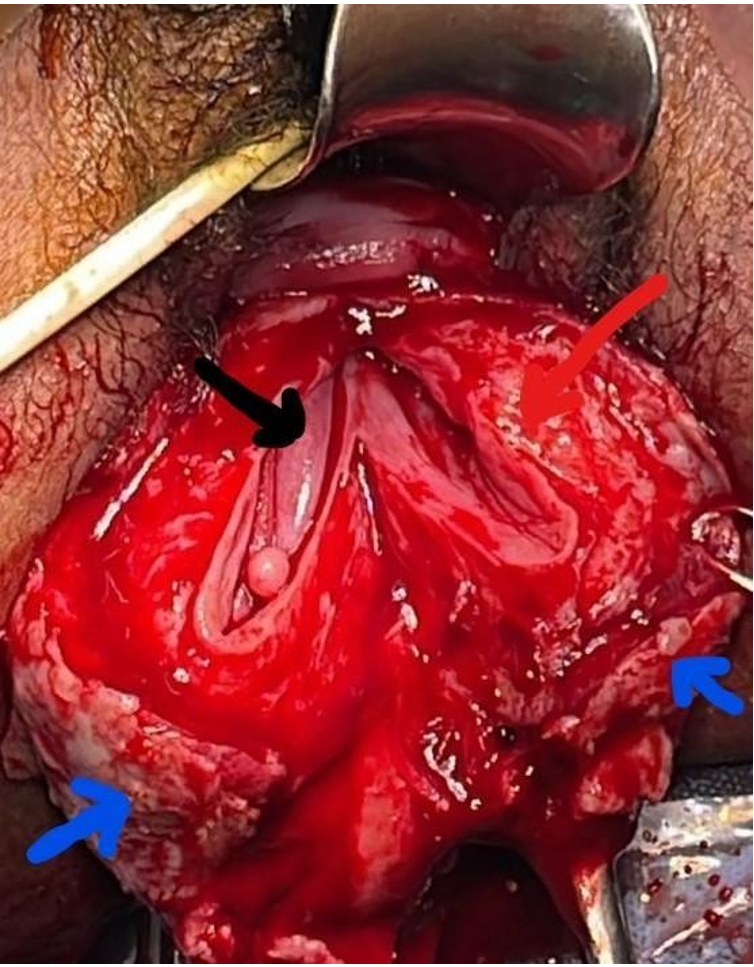
Figure 2: midline incision of the inverted uterus after resection of submucosal fibroid.
The 3 layers of the uterus are inverted
→endometrium
→myometrium
→serosa
Discussion
Uterine inversion is a rare condition. Non puerperal origin is a much rarer one; only 303 cases have been reported in the literature from 1911 to 2018 [4]. It is more common in perimenopausal and menopausal women than in young women [4,5,13-15].
Non puerperal inversion is often chronic which differentiates it from puerperal uterine inversion which is often acute due to the fact that it leads to delivery hemorrhage and hemodynamic instability [1,3,4,18].
The resulting symptomatology is often chronic: minimal menometrorrhagia, pelvic pain with heaviness and urinary signs such as dysuria and pollakiuria.
2 types of uterine inversion classified in 4 stages: incomplete uterine inversion corresponding to stage 1 (simple depression of the uterine fundus without crossing the cervical os). complete uterine inversion corresponding to stages 2 (the uterine fundus crosses the cervical os but remains intravaginal), 3 (the uterine fundus exteriorized to the vulva) and 4 (training of the vaginal walls which take part in the reversion resulting in uterine and vaginal inversion [1-3,14,18].
Stages 3 and 4 are easy to diagnose if the condition is known.
Pelvic ultrasound and MRI are relevant diagnostic tools [1, 2, 3, 4]: uterine inversion is radiologically translated by a vertical central groove in the uterus in longitudinal section forming a Y-shaped aspect of the uterine cavity in incomplete uterine inversion and a U-shaped aspect in the complete form. The radiological assessment also allows the etiological diagnosis.
Submucosal uterine fibroids remain the most common cause of uterine inversion, however a malignant pathology may be the cause in both young women and women who are in
peri-menopause and menopause.
A literature review analyzed 303 cases of non-puerperal uterine inversion [4], finding malignant pathology in 15.6%, myomatous pathology was estimated at 69.5%, idiopathic uterine inversion was estimated at 8%, and other etiologies at 5%. Gumbo et al reported 3 cases of uterine sarcoma in young women under 45 years of age [15]. A case of endometrial cancer in a 28-year-old woman was reported by Ueda et al [15]. A case of uterine inversion secondary to an immature teratoma in an adolescent girl was reported by Sousa et al [17].
Hysterectomy is the most described treatment in the literature for non-puerperal uterine inversion regardless of the associated benign or malignant pathology: 170 cases reported from 1940 to 2017 [4]: 145 cases (86.8%) treated by hysterectomy of which 78.6% (114 cases) combined the 2 abdominal and vaginal techniques. The repositioning of the uterus was reported in only 13% of cases. This may be justified by the fact that non-puerperal uterine inversion is a pathology that is more frequent in the perimenopausal and menopausal periods. In our case, the patient requested a hysterectomy despite her young age because her parental project was complete.
However, in young women, apart from malignancy, conservation of the uterus by repositioning is the treatment of choice to preserve fertility [4, 5, 19, 20]. Several techniques have been described [18]; by the abdominal approach 2 techniques can be used; Huntington's technique and Haultain's technique. The most common trans-vaginal approach is the Spinelli technique.
The Huntington technique consists of a progressive repositioning of the uterus with the help of non-traumatic forceps placed one after the other in the round ligaments and the uterine fundus until complete disinvagination of the uterus.
The spinelli procedure consists of a vesico-uterine detachment, opening of the vesico-uterine cul de sac, complete anterior uterine incision from the inverted fundus to the cervix thus allowing disinvagination of the uterus, after suture of the hysterotomy the repositioning of the uterus in the abdominal cavity is done through the opening of the vesico-uterine cul de sac.
In the literature review, no study was found evaluating the effectiveness of these different techniques; this can be explained by the rarity of the condition, especially in young women.
Conclusion
Non puerperal uterine inversion is an extremely rare pathology. It must be known in order not to ignore its diagnosis. In front of any mass prolapsed in the vagina or in the vulva, it is necessary to think of uterine inversion, especially in the young woman whose uterine conservation, apart from an associated malignant pathology, is the treatment of choice to preserve her fertility.
References
- Kesrouani A, Cortbaoui E, Khaddage A, Ghossein M, Nemr E. Characteristics and Outcome in Non-Puerperal Uterine Inversion. Cureus, 2021; 13(2): e13345. doi: 10.7759/cureus.13.
- Tibrewal R, Goswami S, Chakravorty PS. Non puerperal uterine inversion. J Obstet Gynaecol India, 2012; 62(4): 452-453. doi: 10.1007/s13224-011-0099-3. Epub 2012 Mar 14.
- Benjelloun AT, Makayssi A, Ennachit S, Elkarroumi M. Chronic non-puerperal uterine inversion: about a case. Pan Afr Med J, 2018; 31: 231. doi: 10.11604/pamj.2018.31.231.16668.
- Herath RP, Patabendige M, Rashid M, Wijesinghe PS. Nonpuerperal Uterine Inversion: What the Gynaecologists Need to Know? Obstet Gynecol Int, 2020; 2020: 8625186. doi: 10.1155/2020/8625186. eCollection 2020.
- Kouamé A, Koffi SV, Adjoby R, Diomandé FA, Effoh D, Oussou C, et al. Non-puerperal uterine inversion in a young woman: a case report. J West Afr Coll Surg, 2015; 5(3): 78-83.
- Dadgar S, Pourhosseini SA. Non Puerperal Uterine Inversion Due to Submucous Myoma: A Case Report. J Family Reprod Health. 2018 Sep;12(3):169-172.
- Kulkarni KK, Ajmera SK. A Rare Case of Non-puerperal Acute Uterine Inversion. J Obstet Gynaecol India, 2014; 64(5): 364-365. doi: 10.1007/s13224-012-0294-x. Epub 2012 Nov 10.
- Mihmanli V, Kilic F, Pul S, Kilinc A, Kilickaya A. Magnetic Resonance Imaging of Non-Puerperal Complete Uterine Inversion. Iran J Radiol. 2015; 12(4): e9878. doi: 10.5812/iranjradiol.9878v2. eCollection 2015 Oct.
- Salameh AEK, Aljaberi LM, Almarzooqi RM, Khloof DR, Abu Ras SA, Tabanja R. Non-puerperal uterine inversion associated with adenosarcoma of the uterus: A case report. Case Rep Womens Health. 2019; 22: e00107. doi: 10.1016/j.crwh.2019.e00107.
- Ambreen A, Ahmed F, Zafar S, Khan S. A case report of an aggressive rhabdomyosarcoma associated with non-puerperal uterine inversion. J Obstet Gynaecol. 2020; 40(3): 434-437. doi: 10.1080/01443615.2019.1601166. Epub 2019 Jul 25.
- Shabbir S, Ghayasuddin M, Younus SM, Baloch K. Chronic non puerperal uterine inversion secondary to sub-mucosal fibroid. J Pak Med Assoc, 2014; 64(5): 586-588.
- Pelissier-Komorek A, Lucereau-Barbier M, Diab J, Gavillon N, Graesslin O. Acute non-puerperal uterine inversion the third degre. Gynecol Obstet Fertil, 2013; 41(2): 130-132. doi: 10.1016/j.gyobfe.2012.12.006. Epub 2013 Jan 29.
- Rathod S, Samal SK, Pallavee P, Ghose S. Non puerperal uterine inversion in a young female- a case report. J Clin Diagn Res, 2014; 8(9): OD01-2. doi: 10.7860/JCDR/2014/8961.4826. Epub 2014 Sep 20.
- Herath RP, Patabendige M, Rashid M, Wijesinghe Non puerperal Uterine Inversion: What the Gynaecologists Need to Know? Obstet Gynecol Int, 2020; 2020: 8625186. doi: 10.1155/2020/8625186. eCollection 2020.
- Kirbas A, Daglar K, Kara O, Sucak A, Caglar T. Non-puerperal uterine inversion due to submucous myoma in a woman: a case report. J Exp Ther Oncol, 2016; 11(3): 221-223.
- Khoiwal K, Zaman R, Gill P, Joshi P, Gaurav A, Chaturvedi J. Acute non-puerperal uterine inversion ascribed to malignant mixed Mullerian tumor of uterus: a rare Women Health. 2022; 62(5): 439-443. doi: 10.1080/03630242.2022.2084213. Epub 2022 Jun 2.
- Souza KT, Negrão MV, da Silva Rocha LS, Di Favero G, da Costa SC, Diz Mdel P. Immature uterine teratoma associated with uterine inversion. Rare Tumors, 2014; 6(3): 5530. doi: 10.4081/rt.2014.5530. eCollection 2014 Jul 30.
- Ramanah R, Maillet R, Riethmuller D. Service de gynécologie-obstétrique, CHU Saint Jacques, 2, place Saint-Jacques, 25000 Besançon, France Inversion utérine puerpérale -[5-107-A-10]. Doi: 10.1016/S0246-0335(10)50197-2.
- Zhang X, Sun L, Chen X, Hua K. Uterus preserving reposition of non-puerperal uterine inversion under laparoscope: a case report and literature review. Gynecol Obstet Invest, 2015; 79(3): 206-209. doi: 10.1159/000366475. Epub 2015 Jan 23.
- Pal M, Samanta R, Deb S, Burman SK, Mukherjee J, Ray M. Modified vaginal hysterectomy for chronic non-puerperal complete uterine inversion: video Int Urogynecol J, 2022; 33(2): 431-433. doi: 10.1007/s00192-021-04903-x. Epub 2021 Jul 8.

