Spondylodiscitis, A Rare Infective Endocarditis Complication: About Two Cases
Mouhib Z1,*, Laktib N2, Boumaaz M1, Malki M1, Zaimi A1, Mouine N1, Asfalou I3 and Benyass A4
1Department of Clinical Cardiology, Cardiology center of Mohammed V Military Teaching Hospital, Morocco
2Department of Cardiology Intensive Care Unit, Cardiology center of Mohammed V Military Teaching Hospital, Morocco
3Department Non-invasive cardiac explorations, Cardiology center of Mohammed V Military Teaching Hospital, Morocco
4Cardiology center of Mohammed V Military Teaching Hospital, Morocco
Received Date: 11/09/2022; Published Date: 05/10/2022
*Corresponding author: Mouhib Z, Department of Clinical Cardiology, Cardiology center of Mohammed V Military Teaching Hospital, Rabat, Morocco
Abstract
Infective endocarditis is associated with a high risk of complications such as cerebral emboli, splenic infarction, and rheumatic manifestations (spondylodiscitis, arthritis). The prevalence of rheumatic complications ranges from 25% to 44% and are often predating the diagnosis of infective endocarditis. However, spondylodiscitis remains a rarely observed complication. The goal of this article is to shed a light on this rare complication through two cases of infective endocarditis revealed by a spondylodiscitis. We reported two cases of a 75-year-old male and 50-year-old male both with Streptococcus Bovis infective endocarditis.
Introduction
Infective Endocarditis (IE) refers to a microbial infection of native heart valve, prosthetic valve, or the endocardium, it often occurs in patients with cardiac structural abnormalities but also in normal structural hearts. IE is associated with a high risk of complications such as cerebral emboli, splenic infarction, and rheumatic manifestations (spondylodiscitis, arthritis). The prevalence of rheumatic complications ranges from 25% to 44% and are often predating the diagnosis of IE. However, spondylodiscitis remains a rarely observed complication. The goal of this article is to shed a light on this rare complication by presenting two cases of IE revealed by a spondylodiscitis.
Case Report
Case n°1:
We report the case of a 75-year-old male with no history of cardiovascular disease who presented 15 days prior to his admission, back pain, fever, and night sweats, he was put under pain relief treatment without improvement. One week later, he presented balance disorders, diplopia, and dysarthria. The patient was first admitted in infectious diseases department the transferred to the cardiology department. On examination the patient had murmur in the mitral valve, obliterative arterial disease of the lower limbs and a malleolar ulceration. A Transthoracic Echocardiography (TTE) and a Transesophageal Echocardiography (TOE) were performed and revealed vegetations on the mitral valve (Figure 1). Two blood cultures grew up Streptococcus Bovis. The diagnosis of infective endocarditis was made, and the patient underwent a full work-up to search for complications. Cerebral Computed Tomography (CT) showed a right acute cerebellar infarct, lumbar spine and abdominal CT revealed findings consistent with spondylodiscitis (Figure 2), renal infarction, and aneurysm of the subrenal aorta (Figure 3). He was treated successfully with ciprofloxacin and gentamycin for 6 weeks without sequelae and was discharged.

Figure1: TOE showing a vegetation on the mitral valve (Red arrow).
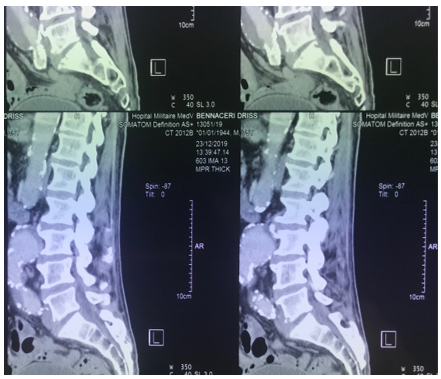
Figure 2: CT-scan revealing a lumbar spondylodiscitis.
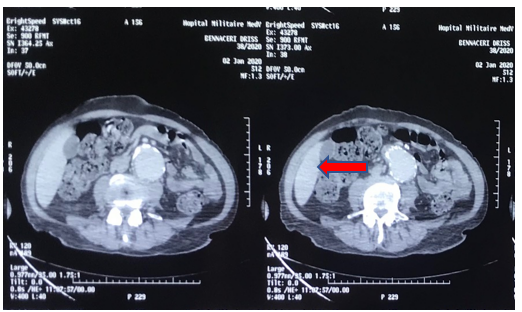
Figure 3: Abdominal CT showing aneurysme of the subrenal Aorta(red arrow).
Case n°2:
A 50-year-old white man developed 3 months before his admission lower back pain, a lumbar spine CT was performed and showed herniated disc. The patient was given pain reliefer but without improvement. Six weeks later, he presented fever, chills, weight loss and worsening of his back pain despite symptomatic treatment. He underwent an MRI of the lumbar spine that revealed a spondylodiscitis of the L2-L3 and L5-S1 vertebrae. The needle aspiration of the spinal site came up positive to non-groupable streptococcus. The patient was first admitted in rheumatology Clinique and was put under empirical antibiotic treatment without improvement. Clinical examination showed a diastolic murmur in the aortic valve and purpura. Blood culture grew out S.Bovis, TTE and TOE displayed two vegetations (Figure 4) of the aortic valve and moderate aortic regurgitation. A clinical diagnosis of IE was made, and an abdominal CT showed renal and splenic infraction (Figure 5). The patient, who was allergic to penicillin, received 6 weeks of intravenous antibiotic therapy: Teicoplanin at a dose of 600 mg daily and Gentamicin at a dose of 160 mg daily with good outcome.

Figure 4: TOE showing two aortic vegetations.
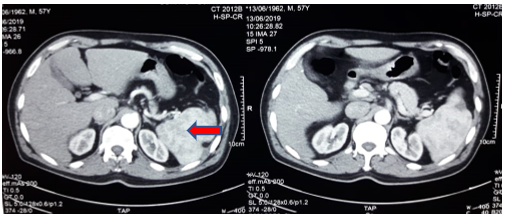
Figure 5: Abdominal CT showing splenic infarction (Red arrow).
Discussion
IE can mimic a variety of manifestations: neurologic, systemic, and rheumatic. The frequency of rheumatic manifestations (RM) ranges from 19 to 44% [1-3], they are not specific of EI and are particularly hard to diagnose. Moreover, they often precede the diagnosis of EI; patients often present first to a rheumatology clinic; causing a delay up to 4 weeks in the diagnosis.
In the recent years, many studies have emphasized the prevalence of these manifestations in patients with IE [4-7]. The RM can be symmetric polyarthritis, arthralgia, myalgia, osteitis, or spondylodiscitis; [2,8]. The incidence of spondylodiscitis as a complication of endocarditis varies widely, ranging from 0,02% to up to 16% [5,9], those numbers show that spondylodiscitis remain rare and has only been described as case reports in the past few years. Ninet et al [10] found the prevalence of spondylodiscitis in patients with IE to be 5,9% and Thomas et al. [11] reported a prevalence of 3,7% among 108 with IE. The rarity of this association contrasts with frequency of back pain as a clinical finding in patient with IE. In many studies on IE back pain was reported in up to 43% of patients [12]. In our case report the two patients had backpain as main clinical manifestation like the results shown in most of the studies. However, in their study Myers and al found that all the patients presenting with back pain had kidney manifestations related to endocarditis (muscular abscess, renal infarction discovered post-mortem).
As concerning the pathophysiology of this complication many mechanisms have been suggested, such as bacterial emboli, immune dysfunction [2,4] or hematogenous dissemination.
Gender in published reports was predominantly masculine and age was mainly above 55 years [10,13,14], our patients were male and age respectively 50 and 60. A large variety of bacteria are found in cases of IE associated with spondylodiscitis. However, in most studies as in our described cases, group D streptococcus is the most frequent causative agent [10,15]. There have also been reported cases of IE caused by coagulase negative staphylococci especially in patient with pacemaker [4]. In a study published by Churchill and al. about bacteria found in patients with endocarditis and RM; streptococcus was first in line (49%), followed by staphylococcus (19%), group D streptococcus (15%) and Gram-negative bacteria, those results were comparable to the classical germs responsible of endocarditis with no complications. However, Vlahakis and al. [1] showed in a recent published report that among nine described cases of patients with enterococcus and RM complicating IE, seven had spondylodiscitis confirmed on MRI.
The treatment does not differ from IE without complications except for duration of treatment. Patient with the association spondylodiscitis and IE should have 6 weeks of treatment and up to 3 months (this duration is explained by spondylodiscitis) is often based on antibiotic therapy and is extended to 6 weeks.
The rheumatic manifestations of IE have in most cases a good outcome under the effect of antibiotic therapy [1] and the overall prognosis depends on the cardiac complications. The treatment does not differ from IE without complications regarding antibiotic except for duration of treatment. Patient with the association spondylodiscitis and IE receive 6 weeks of treatment and up to 3 months.
Conclusion
Spondylodiscitis are common septic metastatic infections of infective endocarditis, which they can reveal. They should always be evoked when a patient with infective endocarditis has inflammatory back pain.
References
- Marcelli C. Manifestations rhumatologiques des endocardites infectieuses.
- Meyers OL, Commerford PJ. Musculoskeletal manifestations of bacterial endocarditis. Ann Rheum Dis, 1977; 36: 517-519.
- Gonzales-Juanatey C, Gonzalez-Gay MA, Llorca J, Crespo F, Garcia- Porrua C, Corredoira J, et al. Rheumatic manifestations of infective endocarditis in non-addicts. A 12-year study. Medicine, 2001; 80: 9-19.
- Le Moal G, Roblot F, Paccalin M, Sosner P, Burucoa C, Roblot P, et al. Clinical and Laboratory Characteristics of Infective Endocarditis When Associated with Spondylodiscitis. Eur J Clin Microbiol Infect Dis, 2002; 21: 671–675. DOI: 10.1007/s10096-002-0798-x.
- Gonzalez-Juanatey C, Gonzalez-Gay MA, Llorca J, Crespo F, GarcÍa-Porrua C, Corredoira J, et al. Rheumatic manifestations of infective endocarditis in nonaddicts: a 12-year study. Medicine (Baltimore), 2001; 80: 9-19. DOI: http://dx. doi.org/10.1097/00005792-200101000-00002.
- Roberts-Thompson PJ, Rischmueller M, Kwiatek RA, Soden M, Ahern MJ, Hill WR, et al. Rheumatic mani- festations of infective endocarditis. Rheumatol Int, 1992; 12: 61-63.
- Azevedo J, Ribeiro C, Loureiro O, Cordeiro A. Rheu- matic symptoms and signs in subacute infective endocarditis. Eur Heart J, 1984; 5[Suppl C]: 71–75.
- Bontoux D, Massias P, Forette B, Coste F. Spondylodiscite lombaire au cours d’une endocardite à entérocoque. Rev Rhum Mal Osteoartic, 1967; 34: 589-592.
- Karlijn MG Houkesa, Saskia E Muddea, Alina A Constantinescub, Nelianne J Verkaika, Erlangga Yusufa. Concomitant endocarditis and spondylodiscitis due to coagulase-negative Staphylococci and a review of the literature. DOI: 10.1016/j.idcr.2021.e01100
- Ninet J, Gayet JL, Etienne J, Bonvoisin B, Vignon E, Berthou JD, et al. Bac- terial endocarditis presenting as acute vertebral osteomyelitis: 14 cases. Eur Heart J, 1984; 5[Suppl C]: 101-105.
- Thomas P, Allal J, Bontoux D, Rossi F, Poupet JY, Petitalot JP, et al. Rheumatological manifestations of infective endocarditis. Ann Rheum Dis, 1984; 43: 716-720.
- Levo Y, Nashif M. Musculoskeletal manifestations of bacterial endocarditis. Clin Exp Rheumatol, 1983; 1: 49-52.
- Bergemer AM, Fouquet B, Goupille P, Born P, Cosnay P, Fauchier JP, et al. Spondylodiscites revelatrices d’ endocardites d’ Osler (àpropos de 4 cas et revue de la littérat- ure). Rhumatologie, 1987; 39: 195-199.
- Pascaretti C, Legrand E, Laporte J, Fromont P, Masson C, Bregeon C, et al. Bacterial endocarditis revealed by infectious discitis. Rev Rheum Engl Ed, 1996; 63: 119-123.
- Mund DJ. Pyogenic vertebral osteomyelitis. Manifesta- tion of bacterial endocarditis. NY State J Med, 1980; 80: 980-982.

