Pacemaker Implantation Via a Persistent Left Superior Vena Cava
Nguadi Jaouad1, Meryem Bennani1, Amine Maliki1, Abdelilah Benelmekki1, Hicham Bouzelmat1, Ali Chaib1, Jihane Fagouri2,*, Zaynab Mouhib2, Lahmouz Youssef2, Hamza Zineeddine2, Najat Mouine2 and Aatif Benyass3
1Rhythmology department, Cardiology Center, Mohammed V Military Instruction Hospital of Rabat, Mohammed V University, Morocco
2Clinical cardiology department, Cardiology Center, Mohammed V Military Instruction Hospital of Rabat, Mohammed V University, Morocco
3Head of Cardiology Center, Mohammed V Military Instruction Hospital of Rabat, Mohammed V University, Morocco
Received Date: 09/09/2022; Published Date: 03/10/2022
*Corresponding author: Jihane Fagouri, Clinical cardiology department, Cardiology Center, Mohammed V Military Instruction Hospital of Rabat, Mohammed V University, Morocco
Abstract
Abnormalities of the superior vena cava correspond to the persistence of a large vena cava due to the presence of an organic vascular system in 0.3% to 0.4% of the subjects. It may be either a duplication of the upper cava or, more commonly, a single left upper cava. The diagnosis is easily made in case of association with a cyanotic heart defect. In contrast, isolated forms are recognized later, as shown by the reported observations. The fact that they are usually perfectly tolerated does not justify their being ignored, because of the risks they entail during certain diagnostic or therapeutic procedures like ion implantation of pacemaker leads.
Keywords: Leads; Persistent left superior vein cava; Complete heart block
Introduction
In mythology, as well as in thoracic surgery or interventional radiology, the implantation of pacemaker is a routine practice. however, the practitioner may be confronted with many challenges related to the venous access and the difficulties of positioning the probes.
The persistence of the superior vena cava is a rare anatomical variation; besides it represents the first congenital malformation of the thoracic venous system. This clinical case illustrates the difficulty of implanting a pacemaker in patients with anomaly of persistence of the left superior vena cava.
Case Report
We report the case of a 60-year-old patient, hypertensive under treatment, admitted for an episode of lipothymia without other accompanying signs, in particular no chest pain. The clinical examination found a patient with bradycardia at 38 bpm and a BP at 160/70, no murmur on the cardiovascular examination, the rest was unremarkable.
The EKG shows a complete BAV with junctional escape rhythm at 38 cpm (Figure 1), the biological assessment and the chest X-ray were without anomalies
The echocardiography objectified a concentric LVH with normal kinetics of the LV (FE 55%).
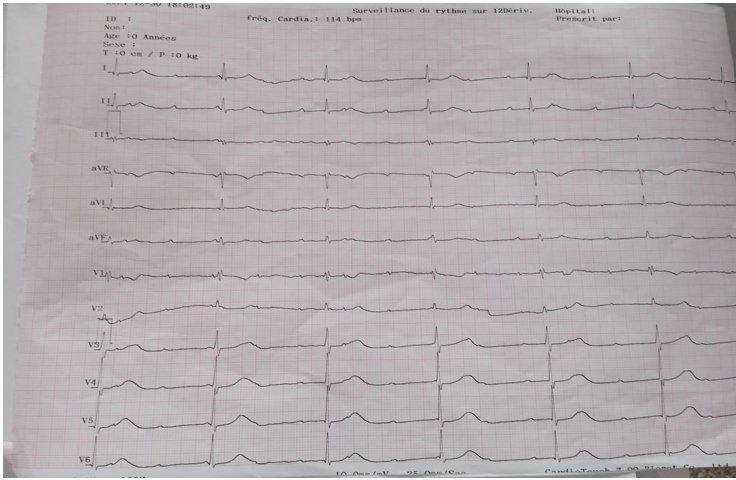
Figure 1: The electrocardiogram of our case, showed a complete BAV with junctional escape rhythm at 38 cpm.
It was therefore decided to implant the patient with a dual-chamber pacemaker. We make our incision at the level of the left deltopectoral groove we puncture the left subclavian vein, it turned out that the introduction of the guide is impossible. We inject the contrast product to better visualize the venous anatomy and the cause of the no - passage of the guide, it is discovered that the patient has a persistence anomaly of the left superior vein cava (figure 2). We again inject the contrast product from the right femoral venous route, we make sure that the right subclavian vein is of normal caliber and flows correctly into the brachiocephalic trunk then into the right atrium.
Our patient is implanted with a dual-chamber pacemaker on the right side.

Figure 2: radioscopy with contrast product showing the persistence of the left superior vein cava.
Discussion
The persistence of the superior vena cava is often asymptomatic, incidental discovery. The incidence of this malformation is estimated at 0.3 – 0.5% in the general population [1,2], and at 12% [3] in patients with documented congenital heart disease
During embryogenesis, the 2 right and left common cardinal veins, arising from the union of the right and left superior and inferior cardinal veins, ensure the venous return of the cranial part of the embryo, and flows into the venous sinus.
During the 8th week of embryonic life, an anastomosis forms between the 2 superior cardinal veins (innominate venous trunk) and the portion of the left superior cardinal vein will regress.
Any anomaly of this phase could be responsible for this malformation, with or without persistence of the superior right vena cava.
The right superior vein cava has a caliber inversely proportional to that of the left superior vein cava, and may be totally absent. Three anatomical forms are described [3] the double superior vena cava (90% of cases) with or without the presence of an innominate venous trunk (40% of cases), the single superior left vena cava (10% of cases).
Drainage of the left superior vein cava is done in 80% of cases in the right atrium via a dilated coronary sinus and remains totally asymptomatic. In 20% of cases, it ends up in the LA, and leads to a right-left shunt with hemodynamic repercussions requiring surgical correction.
The diagnosis of persistent superior vena cava is most often fortuitous, during a pacemaker procedure, or the placement of a Swan Ganz probe through the left subclavian vein or the jugular vein. Transthoracic echocardiography makes it possible to evoke the diagnosis in front of a dilated coronary sinus, and the diagnosis is confirmed by contrast echocardiography, CT angio graphy, angio- MRI or venography.
40% of patients with persistent superior vein cava have an associated congenital heart disease [4], most frequently CIA, bicuspid aortic valve, coarctation of the aorta, atresia of the ostium of the coronary sinus.
In radioscopy, the guide introduced through the left vein travels along the right edge of the spine and descends obliquely towards the right heart. This anatomical particularity complicates the operative gesture, which can lengthen the intervention time as well as the irradiation time.
The difficulty lies in the implantation of the right ventricular lead which arrives through the left superior vein cava in the right atrium, in a direction opposite to the tricuspid valve. A preformed guide or a large loop formed in the right atrium makes it possible to redirect the tip of the lead into the right ventricle and solve the problem as in our case. Actively fixed probes should be used to prevent displacement. The atrial lead is easier to implant, the guide enters the right atrium via the coronary sinus and the lead is screwed onto the free wall of the right atrium.
In case of preoperative diagnosis of a left superior vein cava and in the absence of right superior vein cava. it is recommended to avoid the approach by the cephalic vein, the leads may then be too short and not reach the targeted implantation site.
In practice, the persistence of left superior vein cava is suspected on transthoracic ultrasound in front of a dilated coronary sinus and can be confirmed by CT angiography, angio-MRI, or venography. The injection of contrast product through a vein in the left arm also makes it possible to visualize the course of the left superior vena cava [5].
Conclusion
Persistent left vein cava is rare during the implantation of a pacemaker. It is important to know how to recognize this anatomical particularity in order to anticipate the difficulties related to the positioning of the probes.
The main disadvantage is the angle formed by the coronary sinus with the tricuspid valve. The placement of the atrial lead is limited to the lateral wall of the right atrium. An alternative to the right ventricular lead is the implantation of a left ventricular lead via the coronary sinus or even the epicardial pathway.
Persistence of left superior vein cava may result in longer procedure times and greater risk of lead displacement.
The stimulation parameters are not modified in the long term when these are within the normal limits during the operation.
References
- Paul Wood’s diseases of the heart and J R Coll Gen Pract, 1968; 16(4): 320.
- Buirski G, Jordan SC, Joffe HS, Wilde P. Superior vena caval abnormalities: their occurrence rate, associated cardiac abnormalities and angiographic classification in a paediatric population with congenital heart disease. Clin Radiol, 1986; 37(2): 131‑138.
- Couvreur T, Ghaye B. Left Superior Vena Cava. In : Rémy-Jardin M, Rémy J, éditeurs. Integrated Cardiothoracic Imaging with MDCT [Internet]. Berlin, Heidelberg: Springer; 2009. 2022; p. 289‑305. (Medical Radiology).
- Sarodia BD, Stoller JK. Persistent left superior vena cava: case report and literature review. Respir Care, 2000; 45(4): 411‑416.
- Bashour'it, Antonin1c Sr, Antonin1c jr, Dukel. Left sidedsuperiorveDacava: a rare anomalyprecludingtrans- venous implantation of a permanent pace maker. Cathet Cardiovasc Diagn, 1987; 13: 356-357.

