Coronary Thrombosis in Coronary Ectasia During Asymptomatic SARS-COV-2 Infection
Tagueniti Jalal*, Choho Zakaria, Jaafari Mohamed and Goube Pascal
Department of Cardiology, South Francilien Hospital, Corbeil-Essonnes, France
Received Date: 09/09/2022; Published Date: 30/09/2022
*Corresponding author: Tagueniti Jalal, Department of Cardiology, South Francilien Hospital, Corbeil-Essonnes, France
Abstract
We know now that COVID-19 infection can be a precursor for athero-thrombotic events, even when asymptomatic, coronary ectasia and aneurysm can be also a precursor of thrombosis because of slow flow could lead to in situ thrombosis and causing myocardial damage.
We report a case of a patient admitted for a myocardial infarction during a asymptomatic infection of SARS-COV-2 causing by a massive thrombosis of a aneurysmal coronary artery with conserved flow treated with medical therapy with efficacy anticoagulation with P2Y12 inhibitor and aspirin with good outcomes.
Keywords: Coronary thrombosis; Coronary aneurysm; Ectasia; COVID-19
Introduction
The COVID-19 pandemic related to the SARS-COV-2 virus caused more than 6 million deaths up to August 2022 [1]. Cardiac involvement is multifactorial and determines the prognosis.
Cardiac damage has been reported in several series and may be related to complications of atherosclerotic or be of functional origin.
Ectasias and coronary aneurysms are uncommon coronary artery diseases, can coexist and are poorly known. Their principal etiology in adults is coronary atherosclerosis. It has been suggested that these abnormalities would have poor prognosis and that slow flow could lead to in situ thrombosis and distal embolization. However, ectasias and aneurysms are most often associated with coronary stenosis.
We describe a case of a patient who was admitted for coronary thrombosis of an ectasic artery during asymptomatic Covid-19 infection.
Case Report
It’s 75 years old men, he has hypertension treated by lifestyle and dietary measures alone, he is overweight (IMC 30 kg/m2), he has a history of prostatic carcinoma treated by radiotherapy in remission and an inguinal hernia surgery, vaccinated with 2 doses of Pfizer Biotech.
He consulted the emergency department for prolonged typical in factoid pain that did not yield to the usual analgesic treatment, The clinical examination was unremarkable with a heart rate of 88 beats/minute, blood pressure in both arms symmetrical at 140/100 mmhg, there were no signs of heart failure.
The ECG showed negative T waves in inferior leads DII and AVF, and the troponin dosage returned positive 689 pg/ml (47 times the normal value) with positive CPK 631 u/l (6 times the normal value) the rest of the biological workup: blood creatinine: 97 mmol/l, potassium 4.3 mmol/l, hemoglobin: 15 g/dl with discovery of diabetes with HBA1C at 7.1% and LDL-cholesterol at 1.2 g/l
CRP at 1.2 g/l, a systematic nasopharyngeal PCR on admission to the intensive care unit came back positive.
Cardiac echography shows a conserved ejection fraction with apical hypokinesis.
The patient was admitted to the Cath lab on the same day after having received 250 mg of aspirin and 9000 ui of unfractionated heparin.
The coronarography with femoral access shows a very huge thrombosis of the proximal left descending with aneurysmal coronary arteries with TIMI 3 flow (Figure 1)

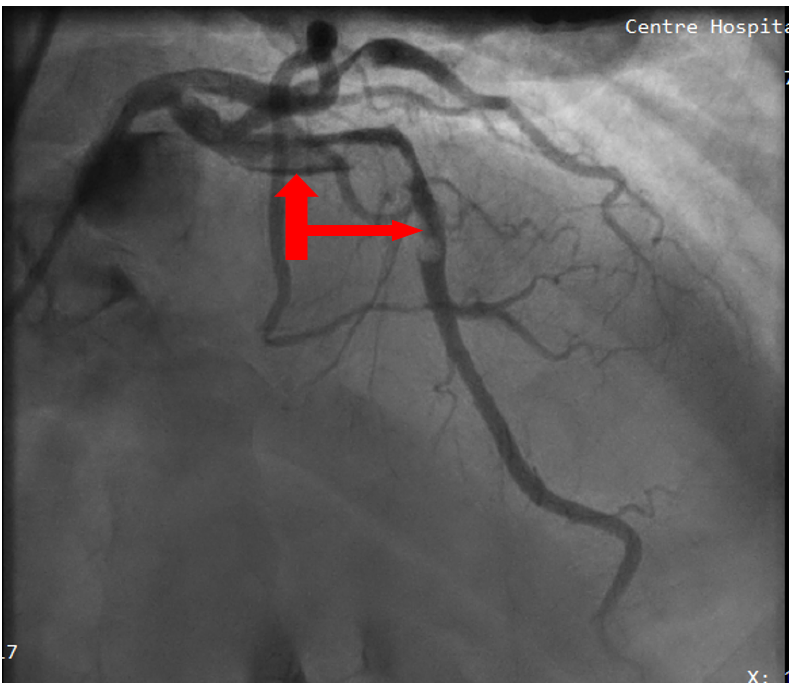
Figure 1: Coronary angiography showing a huge and massive thrombosis of the left descending coronary artery with TIMI 3 flow.
After medical discussion we decided to do initially a medical treatment alone with curative anticoagulation with enoxaparin 0.9 ml twice a day and to add Ticagrelor 90 twice a day with aspirin 75 mg, with Perindopril, Atorvastatin and Bisoprolol 7 days because of the massive thrombotic left descending coronary artery with monitoring of vital functions and electrocardiogram in the intensive care unit.
The evolution was great without any hemodynamic or ischemic or rhythmic events.
The troponin was decreasing 689à50 pg/ml with CPK negativation after one week.
The coronary control after one week of enoxaparin with radial access showed the complete disappearance of the coronary thrombus without significant atheromatous lesion.
It was decided to treat the patient with a double antiplatelet therapy (Asprin 75 mg + Ticagrelor 90mg twice a day) for 1 year.
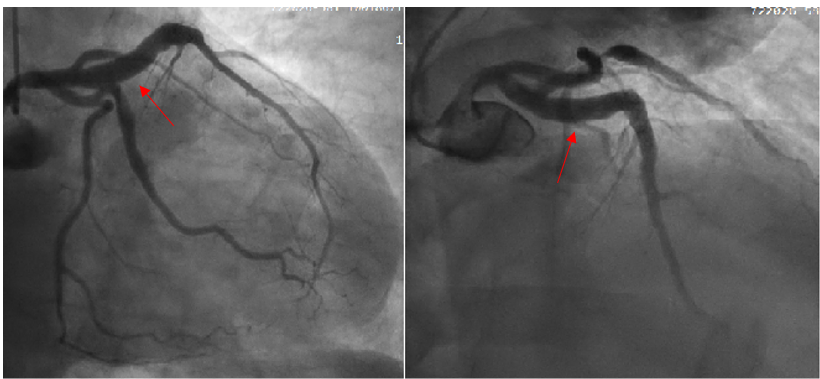
Figure 2: Coronary angiography showing the total regression of the left descending coronary thrombosis.
Discussion
Many possible biological factors related to the COVID-19 infection could be involved in the physiopathological cascade that could precipitate cardiovascular complications [2]:
- High levels of systemic proinflammatory cytokine and mediators of atherosclerosis may determine the plaque rupture through local inflammation.
- Procoagulant effects of systemic inflammation may cause coronary thrombosis: plaque thrombosis, stent thrombosis, and spontaneous thrombosis.
- Oxygen imbalance caused by pneumonia, with an infection-induced increase in metabolic demand and reduced cardiac reserve.
- Direct viral infection of myocardial and vascular cells.
In a observational study of 46 asymptomatic covid-19 patients, and 130 symptomatic covid-19 patients admitted with confirmed STEMI treated with primary percutaneous coronary intervention and thrombus aspiration, all patients had a nasopharyngeal PCR test as well as PCR in coronary thrombus obtained after thromboaspiration. This analysis demonstrates increased thrombus dimension in asymptomatic covid-19 STEMI patients compared with STEMI patients who are not infected. Interestingly, 39 (84.9%) of asymptomatic patients with SARS-COV-2 positive respiratory specimens also had coronary thrombus specimens positive for SARS-COV-2 [3].
Coronary aneurysm ectasia is defined as localized or diffuse dilatation of the coronary arteries more than 1.5 times the diameter of and adjacent healthy reference segment on coronary angiography [4].
Ectasias and coronary aneurysms are uncommon coronary artery diseases, can coexist and are poorly known. Their principal etiology in adults is coronary atherosclerosis. It has been suggested that these abnormalities would have poor prognosis and that slow flow could lead to in situ thrombosis and distal embolisation. However, ectasias and aneurysms are most often associated with coronary stenosis [5].
A Turkish study of 4,119 patients undergoing elective coronary angiography between 2003 and 2005, 173 patients (139 males, 34 females; mean age 61+/-11 years) had CAE, with a prevalence of 4.2%. Distribution of CAE was made according to the classification of Markis et al. The results were compared with those of 145 control patients (115 males, 30 males; mean age 61+/-10 years) who had CAD but not CAE. Following coronary angiography, treatment was designed as aortocoronary bypass (n=3), percutaneous coronary intervention (n=36), and medical therapy (n=98). The mean follow-up was 34.2+/-2.5 months [6].
Our case associated two throbogenic factors (Covid-19, and Ectasias)
Optical coherence tomography (OCT) has emerged as the most accurate method for intracoronary evaluation. Owing to a resolution of 10 to 20 μm, OCT is more accurate than intravascular ultrasound (IVUS) and is useful for the evaluation and characterization of plaque features, both in stable and acute coronary artery disease [7]. Unfortunately, due to the large size of the affected vessel, OCT was not feasible.
When treated by primary percutaneous coronary intervention, the existence of a massive intracoronary thrombus may lead to increased incidence of adverse outcomes. During balloon dilatation or stent implantation, the thrombus was crushed. This procedure could have subsequently caused the thrombus to embolize distally. The dislodged thrombus further activated platelets and this resulted in no reflow in the infarct-related artery [8]. In our case, we did not perform a balloon dilatation because of the absence of flow reduction and because of the risk of no-reflow.
We don’t make thrombectomy because of the massive thrombosis and the risk of the distal embolization and stroke and because of the conserved flow in the artery.
The effective anticoagulation was not prolonged due to the total regression of the thrombus and the conclusion that it was a complication of atherosclerotic plaque, which remains the primary etiology of coronary aneurysms.
Conclusion
SARS-COV-2 infection can be complicated by myocardial infarction. Coronary aneurysms related infarct is often associated with high-burden thrombus formation and has a significantly lower rate of successful reperfusion. Our experience has shown that in coronary artery aneurysm, patients presenting with AMI and evidence of a large thrombus burden effective anticoagulation without angioplasty can give good results if initially we have a normal flow (TIMI3) without any complications.
References
- World Health Organization. Coronavirus Disease (COVID-19) Weekly Epidemiological Update and Weekly Operational Update, 2022; 25.
- Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol, 2020; 5(7): 802- 810.
- Marfella et al. Crit Care, 2021; 25: 217.
- Swaye PS, Fisher LD, Litwin P, et al. Aneurysmal coronary artery disease. Circulation, 1983; 67: 134–138.
- Pinar Bermúdez E1, López Palop R, Lozano Martínez-Luengas I, Cortés Sánchez R, Carrillo Sáez P, Rodríguez Carreras R, et al. Revista Espanola de Cardiologia, 2003; 56(5): 473-479.
- Yilmaz H, Sayar N, Yilmaz M, Tangürek B, Cakmak NUfuk Gürkan, Turk Kardiyoloji, et al. Derneginin Yayin Organidir, 2008; 36(8): 530-535.
- Swanton RH, Thomas ML, Coltart DJ, et al. Coronary artery ectasia—a variant of occlusive coronary arteriosclerosis. Br Heart J, 1978; 40: 393–400.
- Yip HK, Wu CJ, Chang HW, et al. Comparison of impact of primary percutaneous transluminal coronary angioplasty and primary stenting on short-term mortality in patients with cardiogenic shock and evaluation of prognostic determinants. Am J Cardiol, 2001; 87: 1184–1188.

