A Giant Primary Intracranial Hydatid Cyst
Alngar DJIMRABEYE¹,†,*, Moussa ELMI SAAD¹,†, José DIMBI MOKOSSO¹, Yao Christian Hugues DOKPONOU¹, Azizi AYOUB¹, Adyl MELHAOUI¹ and Abdessamad ELOUAHABI¹
1Department of Neurosurgery, Hôpital des Spécialités, Rabat, Mohammed V University of Rabat, Morocoo
†Joint First Authorship
Received Date: 02/08/2022; Published Date: 23/09/2022
*Corresponding author: Alngar DJIMRABEYE, Department of Neurosurgery, Hôpital des Spécialités, Rabat, Mohammed V University of Rabat, Morocoo
Abstract
Back ground: Hydatid disease is a parasitic disease caused by the larval stage of Echinococcus granulosus. It’s commonly affects the liver and lungs but can rarely affect the brain.
Case Presentation: A 5-year-old boy from a rural area with no pathological history was admitted to pediatric emergency for sudden decreased level of consciousness with right‑sided hemiparesis and intermittent vomiting. On Physical examinations, he was disoriented with bilateral papilledema and right‑sided hemiparesis. Brain CT scan revealed a large cystic lesion in the left fronto‑parietal region with mass effect. There was no contrast enhancement, suggestive of hydatid cyst. Radiological investigations of thorax and abdomen disclosed no evidence of hydatid disease. The patient underwent craniotomy and the lesion was removed by irrigating saline between cyst wall and brain interface. Pathological examination confirmed hydatid cysts. Immediate improvement of the symptoms was observed and the patient was discharged on albendazole for 3 months.
Conclusion: The incidence of primary hydatid cyst of brain is very rare. The CT and MRI are the best diagnostic investigation and surgery extirpation of the intact cyst is the treatment of choice, resulting in complete recovery.
Keywords: Intracranial Hydatid Cyst; Echinococcus; Brain; Albendazole
Introduction
Hydatid disease is a parasitic disease caused by the larval stage of Echinococcus granulosus.
E. granulosus can be manifested in humans who act as intermediate host by the development of cysts in the liver, lungs, heart, and brain. Cerebral hydatid disease is very rare and occurs in about 2% of all echinococcal cases [1]. Primary cerebral hydatidosis generally occur as a single lesion. In the brain, it most frequently involves supratentorial region, mainly in the territory of the middle cerebral artery within the parietal lobe. Surgery remains the treatment of choice [2].
Here we report a case of giant primary intracranial hydatid cyst arising from the left frontal lobe, causing midline shift and compression of the contralateral ventricle without demonstrable involvement of other organs.
Case Description
History and Clinical Presentation
A 5-year-old boy from a rural area with no pathological history was admitted to pediatric emergency for sudden decreased level of consciousness with right‑sided hemiparesis and intermittent vomiting. His parents denied any history of trauma or previous surgery related to the brain. Past medical history revealed no drug use On Physical examinations, he was disoriented with bilateral papilledema and right‑sided hemiparesis.
Diagnosis Assessment
Brain Computed tomography (CT) scan revealed a single large spherical hypodense cystic lesion in the left fronto‑parietal region with mass effect and peripheral calcifications (Figure 1). There was no surrounding edema or contrast enhancement. In thorax and abdominal CT scans, there was no cystic lesion.
Laboratory investigations showed elevated white blood cells (leucocytosis) with significant eosinophilia. Liver and renal function tests were normal. Reactiv C-protein level was less than 5 mg/l.
A intracranial hydatid cyst diagnosis was considered.
Surgical Management
The surgical indication was retained and the patient was admitted to the operating room for early cyst extirpation. After skin incision and cutting the periosteum, a large craniotomy was performed. The bone was then carefully separated from the underlying dura mater, which can be very fragile. The pieces of cottonoid strips were gently inserted around the overlying cyst wall. Once the entire cyst wall had been exposed, silicone catheter is introduced between the cyst and the brain parenchyma. Saline solution was injected through this catheter to fascilitate the hydatid removal according to the technique of ARANA-INIGUEZ (Figure 2). After the removal of the hydatid cyst, the dura mater was closed in a watertight fashion.
Pathological examination of the specimen confirmed the diagnosis of hydatid cyst
Outcomes and Follow-up
Postoperatively, he did not present an aggravation of her neurological deficit. Albendazole 10 mg/kg twice daily was started and continued for four months. Pathological examination of the specimen confirmed the diagnosis of hydatid cyst The patient was discharged on fifth post‑operative day with close follow‑up. The patient has been followed 3 months without any neurological deficits.
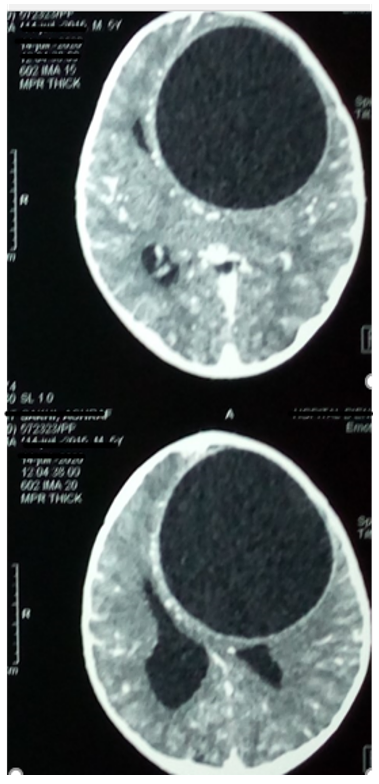
Figure 1: Computed tomography Image showing large single unilocular cystic lesion in left frontal region of brain.
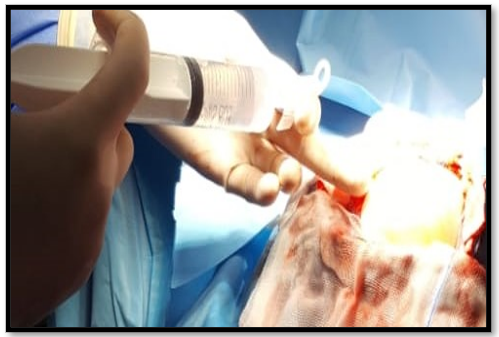
Figure 2: Peroperative photograph of the patient showing normal saline being pushed via a catheter between the cyst wall and brain parenchyma in order to deliver the cyst unruptured.
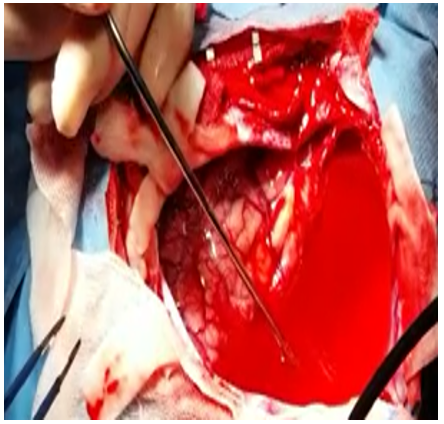
Figure 3: Intraoperative photograph of the patient showing the operative cavity after evacuation of the cyst wall of the cyst.
Discussion
Intracranial hydatid disease is rare, with reported incidence of 1–2% of all cases with hydatid disease. Hydatid disease is endemic in the Middle-East, Mediterranean countries, South America, North Africa and Australia [3]. The liver is the most common organ involved (77%), followed by the lungs (43%). Intracranial hydatid cysts are rare and occur in only 0.5–3% of all the cases of hydatid disease and is usually diagnosed during childhood [2].
A primary cyst is the most common type and is always solitary. It is formed as a result of direct infestation of the brain without demonstrable involvement of other organs [4].
Secondary hydatid cysts occur as a result of rupture of primary cysts in others organs and then reaching by embolization to the brain; they are usually multiple and infertile [1,4]. Our case was a child and have a solitary intrcranial cyst.
The most common presenting symptoms are headache and vomiting due to elevated intracranial pressure. Other common presentations include focal deficits, papilledema, ataxia, hemi-paresis, and disturbed conscious level [2-5].
Most of the cerebral cysts are located in supratentorial structures in the vascular territory of middle cerebral artery affecting parietal lobe [1,6].
Magnetic Resonnace Imaging (MRI) and Computed Tomography (CT) scan are the investigations of choice for radiological diagnosis with MRI being superior for surgical planning. A CT scan characteristically shows hydatid cyst as a well circumscribed spherical or ovoid, hypodense, non‑enhancing cystic lesion with no pericystic edema. On MRI it appears hypointense on T‑1 weighted image and hyperintense with a hypointense halo around the cyst on T‑2 weighted image [2,7].
The definitive management of a cerebral hydatid cyst is surgical removal of the entire cyst without rupture to prevent recurrence and anaphylactic reaction [8,9].
The timing of surgery was based on the neurological and neuroimaging findings in patients. Early cyst extirpation (within 24 hours) was reserved for giant hydatid cysts that caused severe neurological deficits [8].
The most commonly utilised surgical procedure designed to remove the intact cyst completely without rupture is by irrigating saline into the interface between cyst wall and brain [10,11].
Postoperative complications include seizure, subdural effusion, porencephalic cyst, hemorrhage, pneumocephlous, hydrocephalus and transient neurological deficits [2].
Additionnaly, preoperative and postoperative Albendazole may be administered for a number of reasons including; to sterilize the cyst, decrease the risk of anaphylaxis, decrease the tension in cyst wall and reduce the rate of recurrence [4].
Conclusion
Incidence of primary intrcranial hydatid cyst is very rare. The diagnosis should be specifically considered in endemic region. For the treatement, surgical removal with utmost care followed by medical treatment with Albendazole seems to be the most effective treatment.
Compliance with Ethical Standards
Conflict of interest statement
The authors did not receive any funding for the preparation of this case report.
Funding
This work did not receive any grant from funding agencies in the public, commercial, or not-for-profit sectors.
References
- Bhandari Sudhir, Naval CL, Gupta Vishal, et al. Intracranial hydatid cyst-A rare manifestation of Echinococcus infestation. Indian Journal of Medical Specialities, 2015; 6(4): p. 170-172.
- Umerani Muhammad Sohail, Abbas Asad, Sharif Salman, et al. Intra cranial hydatid cyst: A case report of total cyst extirpation and review of surgical technique. Journal of Neurosciences in Rural Practice, 2013; 4(S 01): p. S125-S128.
- Binesh Fariba, Mehrabanian Mohamadreza, Navabii Hossein et al. Primary brain hydatosis. Case Reports, 2011; 2011: p. bcr0620103099.
- Gok Haydar, Başkurt Ozan, et al. Giant Primary Intracranial Hydatid Cyst in Child with Hemiparesis. World Neurosurgery, 2019; 129: p. 404-406.
- Mala Ramanjulu, Ananth ML, Nagaraju BN, et al. Intracranial hydatid cysts-some rare presentations of cases. Journal of Dr. NTR University of Health Sciences, 2014; 3(4): p. 263.
- Arora Shilpa Khanna, Aggarwal Anju, Datta Varsha, et al. Giant primary cerebral hydatid cyst: A rare cause of childhood seizure. Journal of Pediatric Neurosciences, 2014: 9(1): p. 73.
- Wani Nisar A, Kousar Tasleem L, Gojwari Tariq, et al. Computed tomography findings in cerebral hydatid disease. Turkish Neurosurgery, 2011; 21(3): p. 347-351.
- IZCI Yusuf, TÜZÜN Yusuf, SEÇER Halil Ibrahim, et al. Cerebral hydatid cysts: technique and pitfalls of surgical management. Neurosurgical focus, 2008; 24(6): p. E15.
- Senapati Satya Bhusan, Parida Deepak Kumar, Pattajoshi AS, et al. Primary hydatid cyst of brain: Two cases report. Asian journal of neurosurgery, 2015; 10(2): p. 175.
- Reddy D Raja, et al. Managing cerebral and cranial hydatid disease. Neurology India, 2009; 57(2): p. 116.
- Duishanbai Sailike, Dangmurenjiafu Geng, Chen Liu, et al. Clinical Experience-Treatment of intracranial hydatid cysts. Chinese Medical Journal-Beijing, 2011; 124(18): p. 2954.

