A Case of Prurigo Nodularis in an Unlikely Setting
Andrew Kim1, Amanda Levy1 and Michael Poulose2
1New York Institute of Technology College of Osteopathic Medicine, USA
2Saint Joseph Hospital of Long Island, USA
Received Date: 13/08/2022; Published Date: 09/09/2022
*Corresponding author: Andrew Kim, B.S., OMS-III, New York Institute of Technology College of Osteopathic Medicine, USA
Abstract
Prurigo Nodularis (PN) is a rare, chronic dermatologic disease that causes an intense pruritus that can lead to significant physiological and psychological discomfort that may impact quality of life. It is typically characterized by multiple symmetrically-distributed, firm pruritic nodules that spread as the patient scratches them. As a result, individuals with PN can experience pruritus with nodules and excoriations covering their whole body. The exact pathogenesis of PN is unclear, though it is hypothesized that it may possibly be due to increased number of nerve fibers in the papillary dermis or cutaneous small fiber neuropathy. There is no proven cure for PN, and success of management varies by case. There are no US FDA approved treatment options for PN, but Photochemotherapy (PUVA) has been used with promising results.
Keywords: Prurigo Nodularis; Itch; Pruritus; Medical Dermatology; Case Reports
Introduction
Prurigo Nodularis (PN) is a rare, chronic dermatologic disease that causes intense pruritus, leading to significant physiological and psychological discomfort and a diminished quality of life. The estimated prevalence of PN is 72 per 100,000 Americans, and most often presents later in adulthood, between the ages of 51-65, with African-American patients 3.4 times more likely to have PN than white patients [1,2]. The typical clinical presentations of this dermatological disorder are intensely pruritic papules, plaques, and nodules that are multiple in number, firm, and flesh to pink colored. As the individual scratches, the pruritis intensifies and the nodules progressively spread all throughout the body [3]. Currently, diagnosis of PN is entirely clinically based, making it difficult to properly identify and treat, especially due to its rarity.
Methods
Search engines PubMed and Google Scholar were used to obtain information on PN. Keywords included “Prurigo Nodularis”, “Prurigo Nodularis Diagnosis” and “Prurigo Nodularis Treatment”.
Case Presentation
A 48-year-old African American male with a past medical history significant for End Stage Renal Disease (ESRD) diagnosed in 2014, hypertension, diabetes mellitus, neuropathy, prostate cancer, and asthma presented to the emergency department for involuntary blinking and all over sensation of itching. He reported his symptoms began approximately 8 months ago, but became unbearable over the last 2 weeks. He describes the involuntary blinking due to a sensation of something touching his eye, making it impossible for him to keep it open for more than a minute at a time. He also admits to experiencing bilateral facial and ear tingling sensations, whole-body pruritus, and intermittent pain and discomfort worsening over the last year. He describes the pain as a sharp, shooting sensation that occurs at various parts of his body. This patient stated that he had sought treatment in the past, receiving Benadryl and hydroxyzine cream, which had not improved his symptoms. Furthermore, he added that dialysis treatment for his ESRD would exacerbate symptoms. He reported that he had a skin biopsy, which was inconclusive. It was also noted that the patient had a history of non-compliance with treatments or medications. His past surgical history included renal transplant thirteen years prior in 2008 and cardiac bypass. Pertinent positive review of systems included chest pain and pruritus.
On the physical exam, the patient appeared in significant distress due to itching and pain. His skin showed numerous excoriations throughout his entire body. Darkened, hyperpigmented nodules were noted throughout his body, which he noted were pruritic in nature. His vitals included blood pressure of 182/119, heart rate of 88, respiration rate of 22, and temperature of 97.9°F.
The initial plan for this patient was to do blood work, provide the patient with antihistamine for pruritus relief, benzodiazepine for pain relief, Wood’s lamp examination, air puff tonometry, and nephrology consult.
Table 1: Complete blood count and differential indicating of anemia.
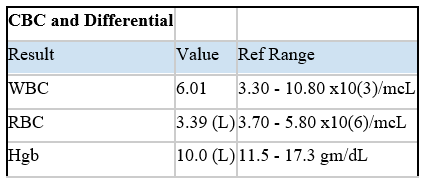
Table 2: Comprehensive metabolic panel showing signs of ESRD and poor glycemic control.
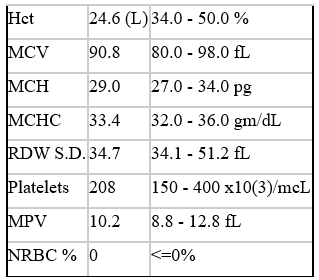
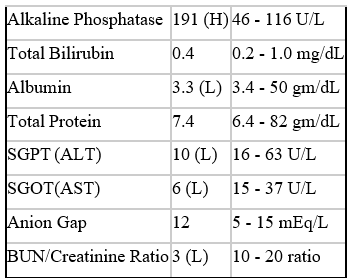
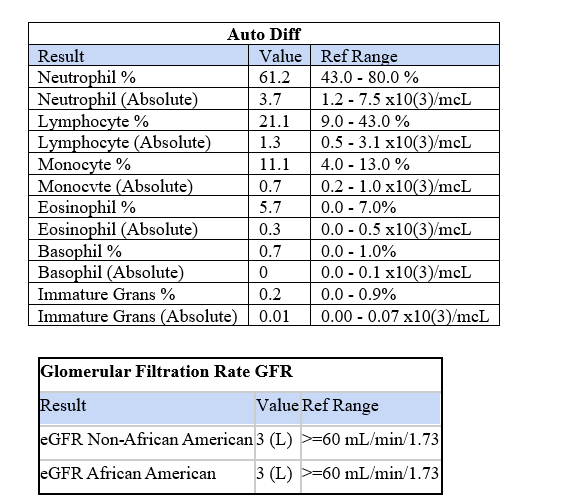
Table 3: Blood differential test showing normal results.
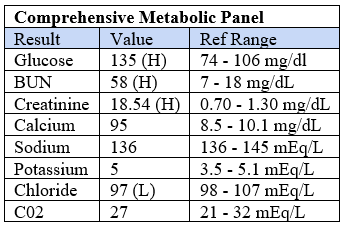
Table 4: Glomerular filtration rate (GFR) showing signs of ESRD.
The patient had nonspecific lab results and his intraocular pressure was 25 according to air puff tonometry. He also had a negative Wood’s lamp examination. Furthermore, symptoms improved minimally on Benadryl and lorazepam. Subsequently, nephrology evaluated the patient and provided the diagnosis of prurigo nodularis. This patient was recommended for PUVA therapy and outpatient management by ophthalmology, rheumatology, and dermatology.
Discussion
PN is a rare, poorly understood condition, making it difficult to identify and diagnose in the emergency department setting. It has been found that repeated scratching due to chronic pruritus leads to an increased pruritic reaction, with further formation of nodules and lichenification of skin [3]. Moreover, there is some evidence for association with various comorbidities, such as hepatitis C, Heliobacter pylori, Strongyloides sterocoralis, mycobacteria, and Human Immunodeficiency Virus (HIV). An increase in the number of sensory structures such as merkel cells and papillary dermal nerves within the epidermis and dermis, respectively, were identified histologically, as well as increased levels of nerve growth factor and its receptor, tyrosine kinase A [ 3]. Laboratory tests will show an increased level of mast cells and neutrophils, as well as interleukin 4 and interleukin 31, suggesting T helper 2 (Th-2) involvement [4]. These all present potential areas for further research in discovering a consistently effective treatment option.
Currently, first line therapy includes a combination of antihistamines, oral steroids, and topical antipruritics or topical corticosteroids [5]. Despite this first line therapy, there is not much research published on the topic during literature review on this topic. There was more research noted on PUVA therapy and Dupixent as a therapy for PN. Arrieta et. al found that phototherapy with UV-B or combination UV-B and UV-A was a suitable treatment as both monotherapy or used in combination with other forms of treatment, especially when PUVA therapy was frequent [6]. Romano researched use of Dupilumab, a medication used in allergic asthma, atopic dermatitis, and chronic rhinosinusitis with nasal polyps, as a treatment of PN. Dupilumab has the ability to block IL-4, IL-13, and possibly Th2 [7]. In previous studies, Dupilumab has been found to lead to complete remission in 50% of PN patients [8]. Co-therapy of Dupilumab and PUVA therapy have also shown promise as a treatment option.
Limitations
There are limited cases and literature on PN, as research is restricted due to the rarity of the condition and limited population size. For example, Arrieta et. al’s sample size only included 44 participants, 30 of which were women and 14 were men [6]. PN is a rare disease, so the limitation of small sample size is understandable; however, it is something future researchers should be aware of. In addition, these therapies typically are temporary and not curative of the disease symptoms. Furthermore, our case represents only one encounter in an emergency department setting.
Conclusion
Although PN is a rare diagnosis and typically one that will not present to the emergency department, this case demonstrates the importance of being cognisant of this condition, as it can cause significant discomfort for the patient and confusion for the healthcare provider. Awareness of PN and knowledge of clinical manifestations, as well as associated conditions allows for a faster diagnosis, maximized care, and knowledge of where to refer patients to help minimize their distress. With no definitive treatment option, further research into the condition is needed to better understand and potentially prevent the exacerbation of symptoms, as well as to discover more effective treatment options.
Conflicts of Interest: No conflict of interest from the main authors, who are osteopathic medical students at NYITCOM.
References
- Huang AH, Canner JK, Khanna R, Kang S, Kwatra Real-World Prevalence of Prurigo Nodularis and Burden of Associated Diseases. J Invest Dermatol, 2020; 140(2): 480-483.e4. doi:10.1016/j.jid.2019.07.697.
- Boozalis E, Tang O, Patel S, et Ethnic differences and comorbidities of 909 prurigo nodularis patients. J Am Acad Dermatol, 2018; 79(4): 714-719.e3. doi:10.1016/j.jaad.2018.04.047.
- Mullins TB, Sharma P, Riley CA, Sonthalia Prurigo Nodularis. In: StatPearls. Treasure Island (FL): StatPearls Publishing, 2021.
- Lee MR, Shumack Prurigo nodularis: A review. Australasian Journal of Dermatology, 2005; 46: 211-220. doi.org/10.1111/j.1440-0960.2005.00187.x.
- Leis M, Fleming P, Lynde Prurigo Nodularis: Review and Emerging Treatments, Skin Therapy Lett, 2021; 26(3): 5-8.
- Arrieta A, Jaka A, Del Alcázar E, Blanco M, Carrascosa JM. Phototherapy for Prurigo Nodularis: Our Experience and a Review of the Literature. Fototerapia en el prurigo Experiencia propia y revisión de la literatura. Actas Dermosifiliogr (Engl Ed), 2021; 112(4): 339-344. doi:10.1016/j.ad.2020.11.007.
- Romano Safety and Effectiveness of Dupilumab in Prurigo Nodularis. J Investig Allergol Clin Immunol, 2021; 31(2): 162-163. doi:10.18176/jiaci.0550.
- Lim VM, Maranda EL, Patel V, Simmons BJ, Jimenez A Review of the Efficacy of Thalidomide and Lenalidomide in the Treatment of Refractory Prurigo Nodularis. Dermatol Ther (Heidelb), 2016; 6(3): 397-411. doi:10.1007/s13555-016-0122-9.

