CHILAIDITI Syndrome: About a Case in Togo
Tamassi Bertrand ESSOBIYOU*, Kodjo Abossisso SAKIYE, Fousseni ALASSANI, Alexandre Palissam Keheou, Mohamed ISSA and Boyodi TCHANGAI
Department of surgery and surgical specialties, University of Lomé, Togo
Received Date: 07/08/2022; Published Date: 29/08/2022
*Corresponding author: Dr ESSOBIYOU Tamassi Bertrand, Department of surgery and surgical specialties, University of Lomé, Togo
Abstract
Introduction: Chilaiditi syndrome is a rare condition in which a portion of the intestine is interposed between the liver and the diaphragm. It occurs preferentially in elderly men. Its diagnosis is radio clinical and treatment is usually conservative. We report a case diagnosed in an elderly man in Togo with good remission under medical treatment.
Case Report: This was a 69-year-old chronically constipated patient admitted with abdominal pain and distension. An unprepared abdominal X-ray showed an interposition of a digestive structure between the liver and the diaphragm. The diagnosis of Chilaiditi syndrome was made. The patient was treated with fluids and laxatives and progressed.
Conclusion: Because of its rarity and diagnostic difficulties, the approach must be rigorous to avoid the trap of pneumoperitoneum. The evolution is often favourable under non-operative treatment.
Keywords: Syndrome; Sign; Chilaiditi; Pneumoperitoneum; Treatment
Introduction
Chilaiditi syndrome is a phenomenon of radio-clinical description [1]. It is a rare syndrome characterised by segmental interposition of the colon between the liver and the diaphragm [1-3]. It was reported by a Greek radiologist in 1910: Demetrius CHILAIDITI [2]. Its incidence in the world population is between 0.025 and 0.28% [2-3]. Chilaiditi syndrome is predominantly male, with a sex ratio of 4, and it is the preserve of the elderly [3]. The syndrome may be symptomatic (Chilaiditi sign), incidental or accompanied by clinical signs (Chilaiditi syndrome) [1,3]. These signs can be both digestive and thoracic [2]. The pitfall of this syndrome is that it can be distinguished from pneumoperitoneum [1]. The management of this syndrome may be conservative or may require surgical intervention [2]. We report a case of Chidailiti syndrome discovered in an elderly subject in Togo, which had a favourable evolution under conservative treatment.
Case Report
This was a 69-year-old patient with a history of gamma nail osteosynthesis of the proximal end of the left femur, admitted to the surgical emergency room for abdominal pain and abdominal distension. On examination, intermittent abdominal pain in the epigastrium and right hypochondrium, recurrent eructation, progressive distension of the abdomen and cessation of bowel movements for 5 days were noted. Gas emission was preserved. In addition, the patient reported recurrent episodes of constipation (1 to 2 episodes of stool per week). We also noted that the patient was bedridden with a Parker score of 4 and a diet rich in residue and poor in fibre. On examination, we found abdominal distension with the tenderness of the right hypochondrium and generalized tympany. On rectal examination, the rectal ampulla contained soft stools. Due to the patient's difficulties in paying for the CT scan, an unprepared abdominal X-ray was performed (Figure 1). This showed significant aerogrelia with the presence of a clearness interposed between the liver and the right diaphragmatic dome. This crescent-shaped clearness was crossed by linear opacities related to a digestive structure. The diagnosis of Chilaiditi syndrome was made and conservative treatment was indicated. The patient was put on a diet and a nasogastric tube was inserted. The patient was given crystalloids (isotonic saline, isotonic glucose, and lactated ringer) at a rate of 3 litres per day. An evacuating enema based on sorbitol citrate and sodium laurilsufoacetate was performed. The outcome was favourable with discharge from the hospital on the 12th day. The patient was advised to follow a dietary regime with a high fibre diet and home mobilisation. Paraffin oil was added to the treatment. Follow-up was satisfactory on the 30th day of hospital discharge.
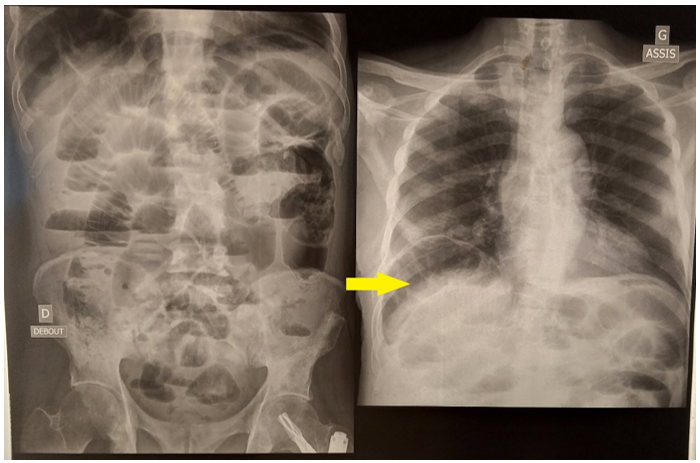
Figure 1: Radiographic appearance of a large aerograft with digestive clarity between the liver and the right diaphragmatic dome (arrow).
Discussion
It is a rare condition with a worldwide incidence of between 0.025 and 0.28% [1-2,4]. Demetrius Chilaiditi, a Greek radiologist, was the first to describe this condition in 1910 [3-4]. This was initially a description of the purely radiological Chilaiditi sign, which was discovered incidentally [4]. When clinical signs are associated with this Chilaiditi sign, it is called Chilaiditi syndrome [1-2,4]. It occurs when a portion of the intestine (mainly the colon) is interposed between the liver and the diaphragm [2-4].
The symptoms associated with Chilaiditi syndrome are many and varied [2-3,5]. Two groups of symptoms stand out: thoracic symptoms and abdominal symptoms [2-3,5]. Abdominal symptoms include nausea, abdominal pain and constipation [2-3,5]. These abdominal signs are the most common in Chilaiditi syndrome [2-3,4-5]. Thoracic signs include dyspnoea and pain mimicking angina pectoris [2-3,5].
Diagnostic certainty is provided by radiology [5]. CT scans are more sensitive than unprepared abdominal X-rays [4-5]. Radiologically it is the distinction with pneumoperitoneum that is the pitfall [4-5]. In Chilaiditi's syndrome, thick linear opacities (colonic haustrations) are present in the suprahepatic clearness [2-3,5-6]. In case of doubt, dynamic films with position change can help: the clarity remains stationary at case change in this syndrome while a pneumoperitoneum moves [1-2,4-5].
Risk factors for Chilaiditi syndrome have been described. Anatomical factors such as laxity of the means of liver fixation and cirrhotic liver atrophy have been implicated [1,3,4-5]. Diaphragm elevation due to phrenic palsy may also be the cause of this condition [1-2,4-5]. Elsewhere, megacolon and colonic hypermobility related to chronic constipation, multiple pregnancies and obesity have been implicated [4-8]. Certain conditions including pulmonary, colonic, rectal and gastric neoplasia may also be the cause [3-5]. In addition, men and the elderly are more likely to present this syndrome [1-4]. Iatrogenic origin has also been reported by some authors in the aftermath of bariatric surgery and colonoscopy [2-3].
The evolution of this disease can lead to complications (occlusion, perforation), which require appropriate management [1,3-5]. The therapeutic management of Chilaiditi syndrome consists of a medical (conservative) and a surgical component [5]. Conservative treatment includes diet, parenteral fluids and intestinal softeners [1-2,4-5,8]. Gastric emptying by tube may be indicated if necessary [2-4]. The indications for surgery are failure of medical treatment and the occurrence of complications [1-2,4-5]. The operative procedures are colectomy and hepatopexy as appropriate [1,3,9]. In patients at risk, a diet rich in dietary fibre and the fight against a sedentary lifestyle should be prescribed [4].
Conclusion
Chilaiditi syndrome is a rare disease of radio clinical description. Abdominal symptoms are the main manifestations of discovery. It affects mostly elderly males. The diagnostic approach must be rigorous to avoid the trap of pneumoperitoneum and unnecessary laparotomies. Factors associated with laxity of the means of hepatic fixation, hypermobility of the intestinal coves and diaphragmatic elevation are at the origin of this disease. The incidence of this condition can be reduced by addressing these known risk factors. The treatment of Chilaiditi syndrome is usually conservative. Surgery is only rarely used.
Conflicts of Interest: The authors have no financial, consultative, institutional, or other relationships that might lead to bias or conflict of interest.
Sources of Funding: The authors declare they have received no funding for the preparation of this document.
Ethical Approval: The study protocol fulfilled the requirements of the Hospital Ethics Committees and was approved.
Consent: Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Author’s Contribution: The study design and data acquisition were done by ETB. IM and KAP carried out the literature review. The manuscript was written by ETB, PE and KAP. All the authors participated in the revision of the manuscript.
Guarantor: ESSOBIYOU Tamassi Bertrand
Provenance and peer review: Not commissioned, externally peer-reviewed
References
- Aqdas AAO, Arwa HI, Ameera SB. Chilaiditi syndrome: an unusual presentation in elderly man. J Surg Case Rep, 2020; 7: 1-3.
- Wei-Hong W, Da-Ren L, Cheng-Cheng F, Ri-Sheng Q. Colonic interposition between liver and left diaphragm-management of chilaiditi syndrome: a case report and literature review. Oncology Letters, 2014; 7: 1657-1660.
- Fiordaliso M, Constantini R, Sanchez SD, Ngjelina J, Surajevs V, Mevlut K. Management of chilaiditi syndrome: our experience and literature review. J Surg Res, 2021; 4(2): 270-277.
- Moaven O, Hodin RA. Chilaiditi syndrome: a rare entity with important differential diagnoses. Gastroenterol Hepatol, 2012; 8: 276-278.
- Farhan A, Sowmya S, Hafiz MAK, Dayakar R. Chilaiditi syndrome : a rare cause of chest pain due to colonic interposition. Cureus, 2020; 12(7): e9288.
- Cawich SO, Spence R, Mohammed F, Gardner MT, Sinanan A, Naraynsingh V. The liver and Chilaiditi's syndrome: significance of hepatic surface grooves. SAGE Open Med Case Rep, 2017; 5: 1-4.
- Krzemiński S. Chilaiditi syndrome: a case report. Pol Merkur Lekarski, 2017; 42: 170-172.
- Karaman O, Kahyaoglu M, Alpay E, Kalaycı A, Gecmen C. Chilaiditi syndrome. Korean J Intern Med, 2018; 33: 1255.
- Zvezdin B, Savić N, Hromis S, Kolarov V, Tausan D, Krnjajić B. Chilaiditi's sign and syndrome: theoretical facts and a case report. Vojnosanit Pregl, 2016; 73: 277-279.

