Inguinal Hernia: Diagnostic Trap
Bachar A, Fatine A, Eddaoudi Y*, Elabassi T and Lefriyekh MR
Department of visceral surgery, University Hassan II, Faculty of Medicine and Pharmacy of Casablanca, CHU Ibn Rochd, Morocco
Received Date: 07/07/2022; Published Date: 18/07/2022
*Corresponding author: Eddaoudi Yassine, Department of visceral surgery, University Hassan II, Faculty of Medicine and Pharmacy of Casablanca, CHU Ibn Rochd, Casablanca, Morocco
Abstract
Hernia is the most common parietal complication in cirrhotic patients. In the latter, it is ascites that explains why its prevalence is higher than in the general population. When a surgical treatment of the hernia is decided, control of the ascites is necessary and is essentially based on repeated punctures , Although the treatment of Hernia was long reserved for symptomatic forms, it is currently recommended to treat paucisymptomatic forms due to serious complications that could occur (rupture or strangulation) including , Emergency surgical treatment is accompanied by a high morbidity and mortality rate in cirrhotic patients. During repair, it is necessary to excise all necrotic tissue.
It is possible to use prosthetic material if the neck is wide without increasing the risk of secondary infection, provided sterile ascites is present. The advantage of the laparoscopic approach is to avoid dissection of superinfected skin. In case of small neck, a cure under local anesthesia is possible.
Keywords: Hernia; Cystic ascites; Emergency; Strangulation
Introduction
Cystic ascites is fluid effusion from the peritoneal cavity excluding purulent (peritonitis), purely bloody (hemoperitoneum) or bilious (choleperitoneum) effusions. [1,2].The clinical presentation is very polymorphic. The diagnosis is guided by imaging and can only be confirmed when carrying out the histological examination after the intervention to determine the origin of the ascites.This is a frequent reason for consultation in daily medical practice. The etiologies are numerous dominated in our country on the one hand by cirrhosis and on the other hand by peritoneal tuberculosis. The Prognosis: perhaps the translation of a serious condition involving the vital prognosis [3].
Material and Methods
This is a 44-year-old patient operated for right crural hernia in 2016 presented with a picture of a left inguinal hernia infatuated, made of pain in the left inguinal region evolving for 24 hours before admission. without concept of stopping materials and gases; the clinical examination objectified a painful mass of the inguinal region irreducible, not expansive to cough, a low inguinal incision on the right side, the rest of the somatic examination was without particularities, on the biological level the hemoglobin at 13 g /dl, white blood cells at 11,000 elements/mm³; a correct ionogram , Faced with the painful nature of the swelling, the patient was taken to the operating room and the surgical exploration objectified the presence of a cystic formation at the level of the inguinal region adherent to the neighboring structures with compartmentalized ascites liquid content with an inflammatory reaction. around this formation, a careful dissection was performed with resection of the cystic mass (Figure 1). The postoperative follow-up was simple and the patient was declared discharged on day 2 postoperatively. The patient was seen in consultation at three months postoperative with a control ultrasound of the inguinal region which did not show any abnormalities.
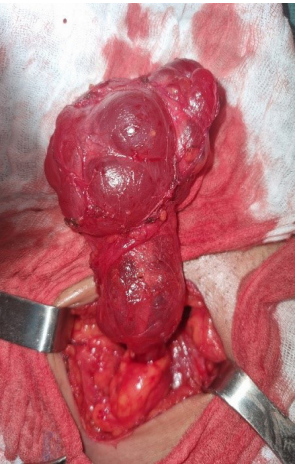
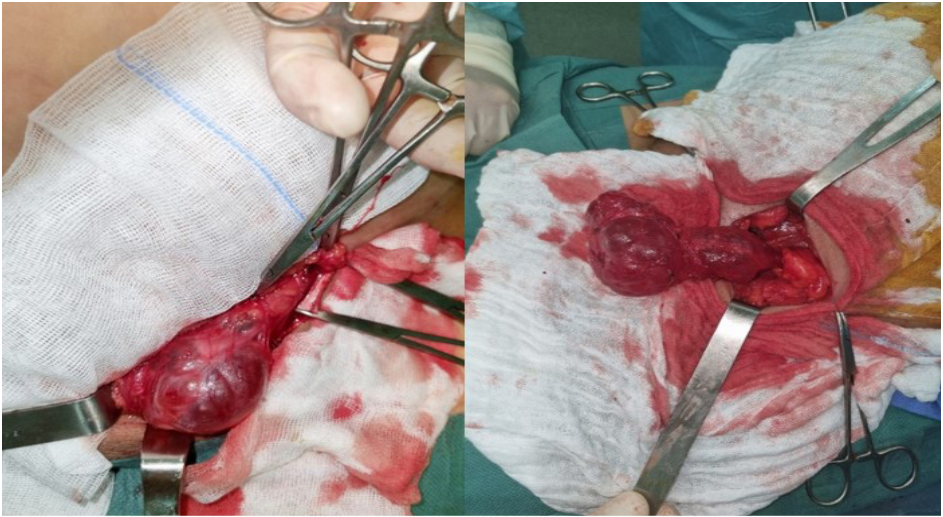
Figure 1: Inguinal Hernia: Diagnostic Trap (Cystic ascites).
Results and Discussion
Patients with cirrhosis are exposed to a significant risk of parietal complications dominated by umbilical hernia (OH), inguinal hernia and eventrations. Ascites causes an increase in intra-abdominal pressure which will push the peritoneum subcutaneously, the subcutaneous peritoneal sac containing ascites is then in direct contact with the skin, which will thin [4], The frequency of these hernias in a cirrhotic compared to the general population is not well known but it is probably lower than that of the umbilical hernia. It is more common in men (>90%), bilateral in 10% of cases and more often associated with the presence of ascites [12], Clinically, it is especially wide neck inguino-scrotal hernias with bursae filled with ascites that are the most troublesome. They can be complicated by strangulation, but trophic skin disorders are almost non-existent [12]. Treatment of symptomatic or complicated forms is indicated. This treatment is all the more indicated as it improves the quality of life of patients [13]. Emergency repair is also associated with a higher risk of morbidity and mortality, justifying elective repair [5]. This surgical treatment is associated with a low postoperative risk even in patients with advanced cirrhosis [12,14]. A repair on a prosthesis is to be recommended especially since the risk of parietal or infectious complications is low [13,14]. Even without a prosthesis, a low recurrence rate (2.3%) has been reported [12]. The ascites puncture which confirms the diagnosis is performed in a sterile manner by puncture in full dullness at the union of the outer 1/3 and the inner 2/3 of the line connecting the umbilicus to the left anterior superior iliac spine, the risk of Hernia increases with the number and duration of ascites attacks, the size of the hernia increases if the ascites persists and it decreases when the ascites disappears [3]. A sudden decrease in ascites can promote strangulation of a digestive loop that remains incarcerated. In some cases, after disappearance of ascites and when the hernial ring is very narrow, a small amount of ascites may persist which is encysted subcutaneously, mimicking strangulation with non-reducible hernia, during ascites flare-ups, vascularized adhesions may occur between the greater omentum which remains in the hernial sac, with an appearance of non-reducible hernia which, although not painful, may lead to the diagnosis of pseudo hernial strangulation. These pseudo strangulations must have a scanner performed to eliminate a real strangulated hernia, Trophic disorders are observed when the ascites is irreducible and they are most often associated with impaired hepatocellular function. The lack of management of ascites after surgical treatment exposes to a high rate of recurrence of hernia. The basis of ascites treatment is medical, combining fluid restriction and diuretics, but in 10% of cases it becomes refractory to medical treatment, leading to the consideration of more aggressive treatments ranging from evacuating puncture , To avoid renal failure, it is preferable, from 3 L of ascites evacuated, to transfuse a vial of 20% albumin for each 2 L evacuated. [11]. The risk of emergency surgery in cirrhotics, the occurrence of serious complications in the event of conservative treatment and a better risk analysis through very large studies of patients lead to consideration of elective repairs if the hepatocellular function is preserved and the controlled ascites [4-7].Morbidity of about 15% similar in cirrhotics and non-cirrhotics, while the risk is higher in the event of emergency surgery in cirrhotics: mortality is seven times higher (3.8% vs. 0.5%) in case of emergency repair [5]. These results encourage broadening the indications for surgery in paucisymptomatic patients.
Conclusion
Hernia is common in cirrhotic patients with ascites.The treatment of ascites participates in the treatment of hernia. The operative risk has become lower in the event of elective repair justifying the treatment of paucisymptomatic forms. The treatment of ascites is based on evacuating punctures. A cure under local anesthesia is indicated for small hernias or if liver disease is advanced. In the absence of ascites infection, laparoscopic treatment with the use of the plate is necessary for wide neck hernias.
References
- Fakhfakh H, Bouhlel A, Ketata H, Sahnoun A, Bahloul A, Mhiri M. Le lymphangiome kystique scrotal. À propos d´un cas. Andrologie, 2005; 15(2): 242-244.
- Umbilical hernias and cirrhose Dokmak S, Aussilhou B, Belghiti J.Service de chirurgie hépatobiliaire et pancréatique, hôpital Beaujon, 100, boulevard duGénéral-Leclerc, 92110 Clichy, France, 2012; 11.
- Carbonell AM, Wolfe Luke LG, DeMaria EJ. Poor outcomes in cirrhosis-associated hernia repair: a nationwide cohort study of 32,033 patients. Hernia, 2005 ;9: 353-357.
- Hansen JB, Thulstrup AM, Vilstup H, Sorensen HT. Danish nationwide cohort study of postoperative death in patients with liver cirrhosis undergoing hernia repair. Br J Surg, 2002; 89: 805-806.
- Carbonell AM, Wolfe Luke LG, DeMaria EJ. Poor outcomes in cirrhosis-associated hernia repair: a nationwide cohort study of 32,033 patients. Hernia, 2005; 9: 353-357.
- Xiao J, Shao Y, Zhu S, He X. Characteristics of adult abdominal cystic Lymphangioma: a single-center Chinese cohort of 12 cases. BMC Gastroenterol, 2020; 244.
- Telem DA, Schiano T, Divino CM. Complicated hernia presentation in patients with advanced cirrhosis and refractory ascites: management and outcome. Surgery, 2010; 148(3): 538-543.
- Marsman HA, Heisterkamp J, Halm JA, Tilanus HW, Metselaar HJ, Kazemier G. Management in patients with liver cirrhosis and an umbilical hernia. Surgery, 2007; 142: 372-375.
- Gorincour G, et al. [Percutaneous treatment of cystic lymphangiomas]. Ann. Chir. Plast. Esthet, 2006; 51: 423–428.
- Eker HH, van Ramshorst GH, de Goede B, et al. A prospective study on elective umbilical hernia repair in patients with liver cirrhosis and ascites. Surgery, 2011; 150(3): 542-546.
- Bezzola T, Bühler L, Chardot C, Morel P. Le traitement chirurgical du lymphangiome kystique abdominal chez l´adulte et chez l´enfant. Journal de Chirurgie, 2008; 145(3): 238-243.
- Zekri B, et al. Lymphangiome kystique rétropéritonéal. Journal Africain d’Hépato-Gastroentérologie, 2010; 4: 260–262.
- Bajaj JS, Varma RR. TIPSS as therapeutic modality for umbilical hernia in patients with advanced liver disease. Liver Transpl, 2004; 10(1): 159-160.
- Oh HK, Kim H, Ryoo S, Choe EK, Park KJ. Inguinal hernia repair in patients with cirrhosis is not associated with increased risk of complications and recurrence. World J Surg, 2011; 35(6): 1229-1233.
- Patti R, Almasio PL, Buscemi S, Famà F, Craxì A, Di Vita G. Inguinal hernioplasty improves the quality of life in patients with cirrhosis. Am J Surg, 2008; 196(3): 373-378.
- Lawson EH, Benjamin E, Busuttil RW, Hiatt JR. Groin herniorrhaphy in patients with cirrhosis and after liver transplantation. Am Surg, 2009; 75(10): 962-965.

