Idiopathic Lobular Panniculitis in a 9-Month-Old
Berfin Ö Özmen*, Mehtap Akça, Rabia Bozdoğan Arpacı and Necdet Kuyucu
Department of Pediatrics, Pediatric Infectious Diseases Unit, Mersin University Faculty of Medicine, Turkey
Department of Pathology, Mersin University Faculty of Medicine, Turkey
Received Date: 18/04/2022; Published Date: 28/04/2022
*Corresponding author: Berfin Ö Özmen, Department of Pediatrics, Pediatric Infectious Diseases Unit, Mersin University Faculty of Medicine, Turkey
Abstract
Panniculitis refers to a wide spectrum of diseases involving inflammation of the subcutaneous adipose tissue of the skin. Weber-Christian disease is a form of idiopathic nodular panniculitis characterized by subcutaneous nodules, inflammatory cells in fat lobules, and systemic symptoms. Panniculitis is an inflammation of the subcutaneous adipose tissue or hypodermatitis, which can be acute or chronic. Despite the similarity of the clinical manifestations of the different forms, several underlying causes have been identified depending on the type of histological involvement [1,2]. In the present case, idiopathic lobular panniculitis, which is rare in pediatric patients, is presented.
Keywords: Child; Nodule; Panniculitis
Case Report
A previously healthy 9-month-old female patient was admitted to our Pediatric Infectious Diseases Outpatient Clinic with fever and reddened swollen lesions on the abdomen, gluteal and inguinal areas, and, more prominently, the thighs. It was learned that her fever had started 3 days ago, that she was not resilient, and that she was taken to the hospital with the formation of rashes. In the patient’s anamnesis, it was stated that approximately 40 days before she was admitted to our outpatient clinic, swelling under the skin had started, accompanied by occasional fever and vomiting. The patient, who had no special conditions in her own or her family history except for the fact that her parents were second-degree cousins, had not been hospitalized until that day. Upon physical examination, it was seen that height and weight development was normal and vital signs were stable. On skin examination, there were subcutaneous lesions of 3×5 cm on the anterior surface of the abdomen, 0.5×0.5 cm in the left lumbar region, approximately 1×1 cm in the left inguinal region, and 1.5×1 cm nodule on an erythematous base in the right inguinal region. Other system examinations were unremarkable (Figures 1, 2, 3). The patient was admitted to the ward for further examination and treatment. According to laboratory tests, kidney and liver function tests, coagulation tests, and complete urinalysis (TIT), the patient was within normal limits. Tuberculin skin test, syphilitic and viral serologies, anti-DNA antibodies, and anti-nuclear antibodies were negative. Immunodeficiency evaluation was normal. No blasts, atypical cells, or Downey cells was seen in the peripheral blood smear. Stool microscopy was unremarkable. Stool Rota-Adeno antigen tests were negative. Immunoglobulin (Ig) E and IgG levels were at age-appropriate levels. Antinuclear Antibody (ANA) and anti-dsDNA were found to be negative. The PPD test for tuberculosis was evaluated as negative. In examinations for specific microbiological agents, the Brucella tube agglutination test and Rose Bengal, HbsAg, anti-HCV, anti-HIV, Toxoplasma, Cytomegalovirus, and EBV test results were found to be normal. There was no growth in blood, throat, urine, or stool cultures. The patient was followed with symptomatic treatment without persistent fever. Abdominal ultrasonography and echocardiography (ECHO) were evaluated as normal. No pathology was detected in an eye examination.

Figure 1: Hard and tender subcutaneous lumps of the lower extremities.

Figure 2: Evolution of nodules toward undulation.

Figure 3: Healing of lesions leaving hyperpigmentation and local skin depression.
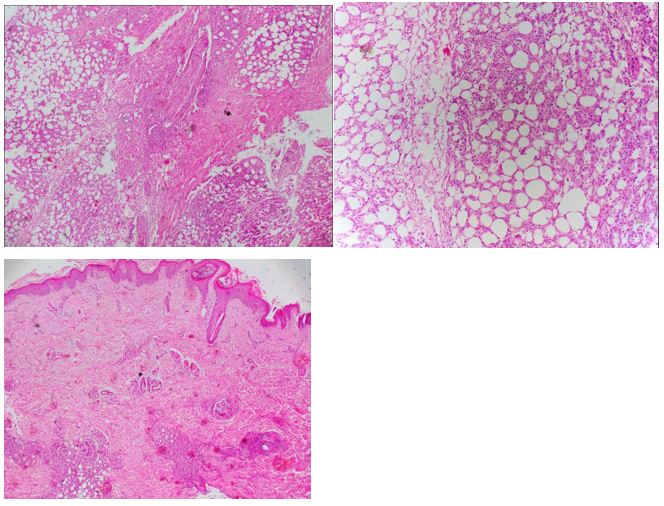
Figures 1, 2, 3: Skin nodule biopsy showing adipose tissue infiltration (H&E, ×70).
In an incisional skin biopsy, neutrophilic leukocytes under the epithelium and around the vessels, mixed-type inflammatory cell infiltration around the skin appendages, and fibrin deposition in the lumen of some vessels were detected in the tissue covered with stratified squamous epithelium with basket-weave orthokeratosis. Panniculitis findings stood out in subcutaneous adipose tissue. Fat necrosis was observed. In some areas, myxoid changes were observed around the skin appendages. In the prepared sections, fibrovascular tissue samples showed a mixed type of pronounced inflammatory cell infiltration, areas suggesting fat necrosis, and macrophage accumulation that was partially lipidized in some regions. Atypically for granulomatous lesions, an infectious agent was not observed in these samples. In differential diagnosis, lobular panniculitis and erythema nodosum and vasculitis were primarily considered. Specific or typical morphological features could not be determined for sclerema neonatorum, lupus panniculitis, Langerhans cell histiocytosis, nodular fasciitis, or inflammatory myofibromatosis, which were included in the differential diagnosis. Bacteriological examination was negative due to the absence of acute lobular hypodermitis with non-vasculitis cystosteatonecrosis, neutrophilic polynuclear infiltrates, and malignant and histiocytic cells. The diagnosis of Weber-Christian disease with multisystem involvement was upheld. The patient was started on hydroxychloroquine. She was discharged on the 8th day of hospitalization due to her good general condition and nutrition, regression of the lesions, absence of fever, and no additional complaints. She was followed as an outpatient and was started on prednisone at 2 mg/kg/day when subcutaneous swelling recurred.
Results and Discussion
Weber-Christian disease, or idiopathic panniculitis, is a rare disease that was first discovered by Pfeifer in 1892 and later better described clinically and histologically by Weber and Christian in 1925 and 1928 [3]. It mainly affects adults and predominantly females. Clinically, it is characterized by recurrent episodes of fever and painful subcutaneous nodules with recurrent purplish lesions of small diameter, usually 1 to 2 cm, on an erythematous base, mainly located on the lower limbs (thighs, legs, and hips). The lesions soon become softer, forming cysts that leave an atrophic hyperpigmented scar [4]. In the present case, lesions were more frequently located on both thighs, the hips, and the lower abdomen. Multisystem involvement, respiratory problems (cough, dyspnea, chest pain), cardiac or renal problems (proteinuria, hematuria), hepatosplenomegaly, digestive system problems (abdominal pain and bloating, diarrhea, digestive bleeding, mesenteric involvement), and rarely neurological (cerebellar) bleeding are associated with high morbidity and mortality rates [5].
The patient in the present case was diagnosed with Weber-Christian disease after neutrophil infiltration and all etiologies of lobular panniculitis (enzymatic causes, antitrypsin α1 deficiency, infectious panniculitis) were excluded.
Neutrophilic Panniculitis (NP) is a clinical-histological entity that is grouped together with several dermatoses characterized by similar clinical manifestations, presenting commonalities and possibly being associated with systemic diseases and hemopathies. In fact, NP may precede the possibility of an underlying Myelodysplastic Syndrome (MDS), which may be detected even during clinical follow-up, or may be a warning sign of progression to acute myeloid leukemia [6]. The rate of association between NP and MDS was found to be significantly higher, reaching 75% in a series of 8 cases [7]. Weber-Christian disease or idiopathic recurrent febrile lobular panniculitis is more frequently noted in the literature in adults and is rarely observed in children, but according to most authors it is a nonspecific entity, possibly encompassing other more specific types of panniculitis [8].
The incidence and prevalence of Weber-Christian disease are unknown, both in the United States and internationally. Weber-Christian disease is rare in adults and even rarer in children. However, albeit rarely, it does occur in children. It has been most commonly reported in people in the fourth to seventh decades of life, with 75% of cases occurring in women after the second decade of life [9]. For example, in a review of children and adolescents in Brazil over a 20-year period (1983-2002), 35 cases of pediatric and adolescent panniculitis were identified, with only 6 cases meeting the criteria for Weber-Christian disease [9].
As in the present case involving the follow-up of a patient with a second attack of Weber-Christian disease, cutaneous findings may be an indicator of an underlying malignant disease. The preferred treatment for idiopathic panniculitis is corticosteroid therapy [10]. In most cases, it will help control exacerbation and dissolve skin lumps, but starting this treatment may mask any underlying disease for a while. In patients with mainly isolated skin manifestations, the clinical course may be characterized by exacerbations and remissions of cutaneous lesions for several years before the disease subsides.
References
- Levine N, Lazarus GS. Subcutaneous fat necrosis after paracentesis: Report of a case in a patient with acute pancreatitis. Arch Dermatol, 1976; 112(7): 993-994. doi:10.1001/archderm.112.7.993.
- Wick MR. Panniculitis: A summary. Semin Diagn Pathol, 2017; 34(3): 261-272. doi: 10.1053/j.semdp.2016.12.004.
- Christian HA. Relapsing febrile nodular nonsuppurative panniculitis. Archives of Internal Medicine, 1928; 42(3): 338-351.
- Ivkov simi M, Jovanovi M, Polja M, Verica Uran KI, Milan M A T I. Livedoid vasculitis idiopathica. skin, locomotor and soft tissue pathology, 2001; 9(1); 141-142.
- Wu F, Zou CC. Childhood Weber-Christian disease: clinical investigation and virus detection. Acta Paediatr, 2007; 96(11): 1665-1669. doi:10.1111/j.1651-2227.2007.00498.x
- Avivi I, Rosenbaum H, Levy Y, Rowe J. Myelodysplastic syndrome and associated skin lesions: a review of the literature. Leuk Res, 1999; 23(4): 323-330. doi:10.1016/s0145-2126(98)00161-1
- Agarwal A, Barrow W, Selim MA, Nicholas MW. Refractory Subcutaneous Sweet Syndrome Treated with Adalimumab. JAMA Dermatol, 2016; 152(7): 842-844. doi:10.1001/jamadermatol.2016.0503.
- White JW Jr, Winkelmann RK. Weber-Christian panniculitis: a review of 30 cases with this diagnosis. J Am Acad Dermatol, 1998; 39(1): 56-62. doi:10.1016/s0190-9622(98)70402-5.
- White JW Jr, Winkelmann RK. Weber-Christian panniculitis: a review of 30 cases with this diagnosis. J Am Acad Dermatol, 1998; 39(1): 56-62. doi:10.1016/s0190-9622(98)70402-5.
- Moraes AJ, Soares PM, Zapata AL, Lotito AP, Sallum AM, Silva CA. Panniculitis in childhood and adolescence. Pediatr Int, 2006; 48(1): 48-53. doi:10.1111/j.1442-200X.2006.02169.x
- Saghir S, Meskini T, Ettair S, Erreimi N, Mouane N. La maladie de Weber-Christian: s'agit-il d'un état pré-leucémique? [Weber-Christian's disease: a preleukemic disorder?]. Pan Afr Med J, 2019; 32: 127. Published 2019 Mar 18. doi:10.11604/pamj.2019.32.127.16106

