Rhino-cerebral Mucormycosis
Mainak Datta*, Rupam Sinha, Soumyabrata Sarkar, Harshvardhan jha, Sayani Shome, Debarati Deb
Department of oral medicine and radiology, Haldia institute of dental sciences and research, India
Department of oral and maxillofacial Pathology, Haldia institute of dental sciences and research, India
Received Date: 23/03/2022; Published Date: 08/04/2022
*Corresponding author: Dr. Mainak Datta, Post graduate trainee, Department of oral medicine and radiology, Haldia institute of dental sciences and research, India
Abstract
Mucor mycosis is one of the most rapidly progressing, opportunistic fungal infection, predominantly involves nose and paranasal sinuses after inhalation of fungal spores. Main causative organisms are of the subphylum mucoromycete. The incidence of Mucor mycosis is approximately 1.7 cases per 1,000,000 inhabitants per year in worldwide scenario with no such gender predilection. The main pre-disposing factors includes poorly controlled diabetes, ketoacidosis, leukemia, Immunodeficiency states, prolonged steroid therapy etc. Mucor mycosis affecting the maxilla is less common due to its rich vascular supply. The common form of this infection is seen in the rhinomaxillary region and in patients. Here we have presented a case of Rhino-maxillary Mucor mycosis of 35 years old male patient. Hence, early-stage diagnosis of this potentially life-threatening clinical condition and start of treatment importance is of prime importance in reducing the mortality rate to any health care physician.
Keywords: Mucormycosis; Palatal perforation; Immuno-competent; Opportunistic infection
Introduction
Mucor mycosis also known as phycomycosis, zygomycosis is an opportunistic fungal infection caused by fungi belonging to the Mucorales order and the Mucoraceae family. This clinical entity was first described by Paultauf in the year 1885 [1]. It represents the third most common angio-invasive fungal infection after candidiasis and aspergillosis. The incidence rate of mucormycosis varies from 0.005 to 1.7 per million population in worldwide scenario. In India, prevalence of mucormycosis is estimated as 140 per million population, which is about 80 times higher than the prevalence in developed countries [2]. It usually affects the immune-compromised individuals and is rarely seen in apparently healthy individuals [3]. In the compromised host, mucormycosis infection results from altered immunity in which rapid proliferation and invasion of fungal organisms ensue in deeper tissues [4]. There is no age wise and gender wise disease predominance. The various predisposing factors for mucormycosis are uncontrolled diabetes (particularly in patients having ketoacidosis), malignancies such as lymphomas and leukemias, renal failure, organ transplant, long-term corticosteroid and immunosuppressive therapy, cirrhosis, burns, protein-energy malnutrition, and acquired immune deficiency syndrome (AIDS) [5]. Pathophysiology involves inhalation of spores through the nose or mouth or even through a skin laceration. Individuals with compromised cellular and humoral defense mechanisms may generate inadequate response. The fungus may then spread to the paranasal sinuses and consequently to the orbit, meninges, and brain by direct extension [6]. Successful management of this fatal infection requires early identification of the disease and aggressive and prompt medical and surgical interventions to prevent the high morbidity and mortality associated with this disease process [7]. We report here with a case of mucormycosis of 45 years old male patient with uncontrolled diabetes.
Case Report
A 45-year-old male patient reported to the department of oral medicine and radiology with a chief complaint of pain and swelling in the upper right side of the face since last 1 month. He was a known diabetic and hypertensive for last 10 years and takes medication regarding that. Patient also gave history of intermittent headache, brownish discharge from right nostrils. Patient also gave history of blurring of vision in right eye along with whitish discharge from eye. There was no associated fever history or taste or smell loss present as told by patient himself. Patient gave history of tobacco chewing habit from last 6 years.
On extra-oral examination a moderate diffuse swelling was seen on middle 3rd of the Right-side face. A diffuse swelling involving right peri-orbital area seen along with mild proptosis of eyeball with a haziness on sclera region. Patient had sufficient mouth opening and no cervico-facial lymphadenopathy.
On intraoral examination a round, irregular palatal perforation, approx. 1.5cm x1.5cm in diameter present in the right half of hard palate area, with a blackish granulation tissue base. Provisional diagnosis of Chronic osteomyelitis of maxilla was given with differential diagnosis like aspergillosis, Wegners granulomatosis, malignancy.
Hematological investigations showed increased blood sugar levels (FBS 158 mg/dl, PPBS 326 mg/dl), which gave a clue for considering Mucor mycosis in the diagnosis. IOPAR and Cross sectional maxillary occlusal radiograph showed definite palatal perforation area in right incisive fossa area, which is around 1.5 cm x 1.5 cm in diameter and around ovoid in shape. Contrast Enhanced Computed Tomography (CECT) showed destruction of part of antero-inferior wall right of maxillary sinus along with thickening of antral mucosal wall, discontinuation of continuity of right palatal floor, along with an irregular hyperdense mass seen involving whole right maxillary sinus. Pansinusitis or haziness of the right sided maxillary sinus also seen.
Tissue swab was taken from palatal perforation area, granulation tissue swab sample taken for culture and sensitivity , cultured in KOH mount and Sabourose-Dextrose Agar (SDA) media which shows growth of fungal hyphe along with spoeres. Histopathological findings (HP) including H/E-stained slide showed presence of fibrovascular connective tissue stroma comprised of numerous mononuclear cronic inflammatory cells along with few multinucleated giant cells. There is also presence of slender, non-septae branched fungal hyphae along with numerous inflammatory cells. PAS-stained section confirms all previous finding along with presence of magenta-colored fungal hyphae.
Final diagnosis of Rhinomaxillary Mucormycosis (RCM) was considered as maxilla, associated sinuses and nasal fossa of right side were involved. The patient was kept under human mixtard insulin (SC), liposomal amphotericin B (IV 50 mg with 5% dextrose) and antibiotics for 1 week and later planned for surgery under GA. Debridement and irrigation of maxillary sinus, Repair of Palatal perforation surgically by by palatal tissue grafting, Oral prophylasis were done. Patient was called for follow up after 15day, 1month and 3 month which shows periodic improvement of condition.

Figure 1A, 1B: Front Profile and lateral profile view of the patient.
Figure 1C: Involvement of Right eye showing erythema, Discharge from eye.

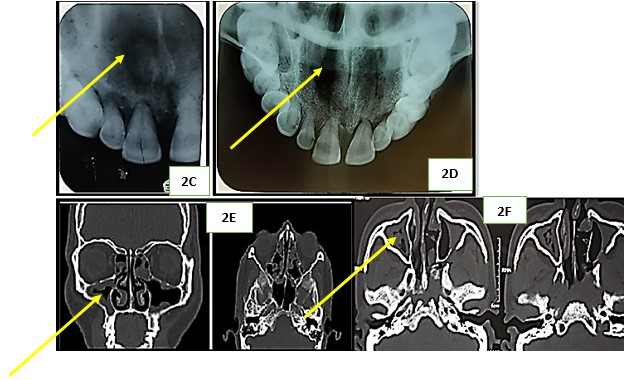
Figure 2A: Intra-oral view showing palatal perforation.
Figure 2B: Coated tongue.
Figure 2C: IOPAR showing palatal perforation at incisive fossa area.
Figure 2D: Maxillary cross sectional occlusal radiograph showing palatal perforation in right hard palatal half.
Figure 2E, 2F: CECT showing perforated palatal floor along with presence of hyperdense radio-opaque mass involving Right maxillary sinus.
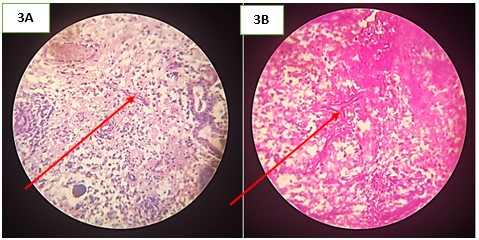
Figure 3A: PAS-stained histopathological slide showing fungal hyphae.
Figure 3B: H/E-stained section showing presence of fungal hyphae along with numerous inflammatory cells.
Discussion
Mucormycosis is an uncommon but fatal opportunistic infection caused by a saprophytic fungus ‘Phycomycete’ group that occurs in soil or as a mold on decaying food. This condition are also known as zygomycosis and phycomycosis [1,2]. Paltauf described the first case of mucormycosis in the year 1885 in human beings [1]. It is the third most common invasive fungal infection, following aspergillosis and candidiasis. It accounts for 8.3-13.0% of all fungal infections and swab commonly cultured from the nose, throat, mouth, and feces [3]. No specific racial or geographic distribution was seen; neither any specific gender or age predilection was noticed [4].
Five major clinical forms are described depending on the portal of entry and the predisposing risk factors of the patient. These are: Rhinocerebral/rhinomaxillary and pulmonary, being the most common forms, followed by the gastrointestinal, cutaneous, and disseminated types [5]. Rhinocerebral mucormycosis is usually caused by Rhizopus oryzae or Rhizopus arrhizus, and typically occurs in the nasal cavity or walls of paranasal sinuses. These fungi erode and invade small blood vessels, leading to thrombosis, ischemia, and tissue necrosis. Involvement of sinuses or spread into the oral cavity (hard palate) is common. Pain, nasal discharge, and foul smell with black necrotic oral ulceration are the common findings. [6] From the palate and nasal mucosa, the infection may progressively spread via the angular, lacrimal, and ethmoidal vessels, even extending into the retro-orbital region. It can further cause functional impairment of cranial nerve (mainly II, III, IV, and VI). Hematogenous spread to the cavernous sinus and cavernous sinus thrombosis also have been reported. [7]
It is most commonly seen in immunocompromised individuals, especially diabetics, or on prolonged steroid therapy. The present case of Mucor mycosis deals with patient with uncontrolled diabetes.
Intraorally, this disease entity clinically presents as a palatal ulcer with raised erythematous borders. Surface of the ulcer appears black and necrotic with areas of denudation coved with granulation tissue sough. [7] It can also present with a palatal swelling, rather than the ulcer, and is associated with adjacent bony/alveolar denudation. In the present case, a mild diffuse swelling in the anterior hard palate region was observed along with ulceration and perforation of palatal floor, with generalized periodontal pockets and compromised oral health. Other associated signs and symptoms are nasal obstruction, blood-tinged blackish nasal discharge, facial pain and headache, visual disturbances involving right eye, but no sign of facial paralysis. In cases of cranial base involvement, blindness, lethargy, seizures, or even death may occur [8].
PA skull or paranasal sinus view may demonstrate sinus mucosal thickening, sinus opacification without fluid levels, and spotty destruction of the bony walls of the paranasal sinuses. CT scan or Magnetic Resonance Imaging (MRI) are helpful tools to delineate the extent of the disease [9] In the present case. CT scan helps to reveal the extent of the underlying destruction by the lesion.
Histopathologically, mucormycosis is characterized by numerous large non-septate hyphae (budding, non-dichotomous branching) approximately at 90° angle with extensive tissue necrosis. Angioinvasion by the fungi and neutrophilic infiltrate in the necrotic tissue can also be appreciated [10]. Definitive diagnosis of mucormycosis is only made histopathologically. The fungus can further be demonstrated by use of a special stain, such as Grocott-Gomori methenamine silver stain, periodic acid Schiff, or calcofluor stain [11]. The Gomori's silver methenamine stain was used to demonstrate the fungal hyphae in the present case.
Successful treatment of mucormycosis requires early diagnosis. There are two primary aspects of the management of the rhinomaxillary mucormycosis for an immunocompetent host: Systemic antifungal therapy in the form of amphotericin-B or the more effective liposomal amphotericin-B and the surgical debridement of the dead, infracted, or infected tissue. The primary aspects of the management of the rhinomaxillary mucormycosis are reversal of the underlying risk factors (immunosuppression), prompt administration of antifungal therapy, and surgical debridement of the dead, infracted, or infected tissue. Primary antifungal therapy can be administered in the form of conventional amphotericin-B or lipid formulations of amphotericin (1 mg/kg/day) or in combination with echinocandin, posaconazole, or deferasirox (salvage therapy) [12].
Conclusion
The incidence of development of Mucor mycosis, even in immunocompetent individuals, is on the rise. Characteristic clinical feature of ulceration or necrosis can sometimes be absent in the early stages of the infection. Advanced radiological techniques such as CT are helpful in its early detection. The infection can only be diagnosed histopathologically. Management of the rhinomaxillary Mucor mycosis for an immunocompetent host includes systemic antifungal therapy in the form of amphotericin-B or the more effective liposomal amphotericin-B and the surgical debridement of dead, infracted, or infected tissue. Early diagnosis is of paramount importance which can prevent fatal potential systemic complications.
References
- Garg R, Gupta VV, Ashok L. Rhinomaxillary mucormycosis: A palatal ulcer. Contemp Clin Dent, 2018; 2: 119-123
- Scully C, de Almeida OP. Orofacial manifestations of the systemic mycoses. J Oral Pathol Med, 2019; 21: 289-294.
- Prabhu RM, Patel R. Mucor mycosis and entomophthoramycosis: A review of the clinical manifestations, diagnosis and treatment. Clin Microbiol Infect, 2014; 10(Suppl 1): 31-47.
- Pandey A, George J, Rao NN. Mucormycosis causing extensive destruction of maxilla. Indian J Dent Res, 2016; 15: 74-77.
- Hauman CH, Raubenheimer EJ. Oro-facial Mucor mycosis. Oral Surg Oral Med Oral Pathol, 2013; 68: 624-627.
- Goel S, Palaskar S, Shetty VP, Bhushan A. Rhinomaxillary Mucor mycosis with cerebral extension. J Oral Maxillofac Pathol 2019; 13: 14-17.
- Mignogna MD, Fortuna G, Leuci S, Adamo D, Ruoppo E, Siano M, et al. Mucor mycosis in immunocompetent patients: A case-series of patients with maxillary sinus involvement and a critical review of the literature. Int J Infect Dis 2018;15: e533-e540.
- Jayachandran S, Krithika C. Mucor mycosis presenting as palatal perforation. Indian J Dent Res, 2016; 17: 139-142.
- Ribes JA, Vanover-Sams CL, Baker DJ. Zygomycetes in human disease. Clin Microbiol Rev, 2010; 13: 236-301.
- Sun HY, Singh N. Mucor mycosis: Its contemporary face and management strategies. Lancet Infect Dis, 2011; 11: 301-311.
- Del Valle Zapico A, Rubio Suárez A, Mellado Encinas P, Morales Angulo C, Cabrera Pozuelo E. Mucor mycosis of the sphenoid sinus in an otherwise healthy patient. Case report and literature review. J Laryngol Otol, 2016; 110: 471-473.
- Sridhara SR, Paragache G, Panda NK, Chakrabarti A. Mucor mycosis in immunocompetent individuals: An increasing trend. J Otolaryngol, 2015; 34: 402-406.

