Kikuchi-Fujimoto Disease (KFD) in a Young Boy with Cervical Lymphadenopathy
Arshad Ali Jariko, Raja Taha Yaseen Khan*, Ghous Bux Somro, Shoaib Ahmed Khan,Hina Ismail, MuneerTareen, Muhammad Qaiser Panezai, Farina M Hanif, Abbas Ali Tasneem, Zain Majid, Nasir Hasan Luck and Muhammad Mubarak
Department of Hepatogastroenterology, Sindh Institute of Urology and Transplantation
Received Date: 14/03/2022; Published Date: 28/03/2022
*Corresponding author: Raja Taha Yaseen Khan, Department of Hepatogastroenterology, Sindh Institute of Urology and Transplantation, Karachi, Pakistan
Abstract
The disease Kikuchi-Fujimoto Disease (KFD) is a rare benign entity of necrotizing histiocytic lymphadenitis. A case
of a 7-year-old has been discussed in here. His presenting complaints were fever with chills associated with odynophagia and tender cervical lymph adenopathy. The diagnosis was made on the basis of cervical lymph node biopsy. Improvement in symptoms were noted with NSAIDs treatment. This is the first case which has been reported from Pakistan, especially in a young boy which is against the odds as it is the disease which is more common in females and has autoimmune etiology
Keywords: Kikuchi-Fujimoto Disease (KFD); Necrotizing histiocytic lymphadenitis
Introduction
One of the rare, idiopathic and generally self-limiting cause of lymphadenitis that is highly prevalent among Asians is Kikuchi-Fujimoto Disease (KFD), also called histiocytic necrotizing lymphadenitis. The incidence is high in Japanese population with only a few cases reported from Europe. It was first described in 1972 by the pathologists Kikuchi and Fujimoto, thus the disease name [1,2]. There is some uncertainty regarding its etiology, but likely causative agents seem to more than one, probably viruses, that activate the autoimmune inflammatory response in genetically predisposed individuals [3,4]. It most commonly affects young Asian women usually in the third decade of life and is usually responsive to the treatment [5]. This disease carries a long term of risk of recurrence or progression of Systemic lupus Erythematosis (SLE) [6]. The symptoms of KFD usually include symptoms of fever, upper respiratory tract infection and cervical lymphadenopathy. The less common presenting symptoms include chills, night sweats, arthralgia, rash, and weight loss. Clinically, splenomegaly or hepatomegaly along with tender lymphadenopathy have been reported. Histological analysis of an affected lymph node is needed to confirm the diagnosis of KFD [7] Laboratory investigations reveal raised inflammatory markers along with cytopenias [8,9].
Here we present for the first time a boy in 1st decade of life, diagnosed with KFD on cervical lymph node biopsy.
Case Report
A seven-year-old boy, presented to us with complaints of high-grade fever associated with rigors and chills since last 25 days. The fever was intermittent, mostly occurring in the evening associated with pain during swallowing (odynophagia). There is no history of associated nausea and vomiting, altered bowel habits, cough, headache or altered level of consciousness. He used tap water for drinking purposes and had no prior comorbidities. His mother denied family history of any chronic illness. On examination, he was alert and oriented but was febrile with temperature of 103-104 °F and left cervical lymph node was enlarged and palpable, which was tender to touch and matted. There was no jaundice, hepatosplenomegaly or palpable lymph node. Rest of the examination was unremarkable. On investigations, he was found to have normal complete blood count while his C-Reactive Protein (CRP) was 16mg/dl (0.8-1.8 mg/dl) along with Erythrocyte Sedimentation Rate (ESR) of 70mm/hour (0-10) and lactate dehydrogenase was also on slightly higher side i.e-650 IU/ml (normal range-<200). His PPD test was negative. and his viral serology including Varicella Zoster Virus (VZV) IgM, Cytomegalovirus (CMV) IgM, Epstein Bar Virus (EBV) IgM and Herpes Simplex Virus (HSV) IgM were negative. Chest Xray was normal. Ultrasonography (US) revealed a single set of enlarged left -sided hypoechoic posterior cervical lymph node (maximum size of 2 cm) with low peripheral flow on ultrasound Doppler along with eccentric cortical thickening hilar deviation. CT chest, abdomen and pelvis. Documented no other lymph node enlargement. Considering the diagnostic dilemma, he underwent excisional left posterior cervical lymph node biopsy which revealed fragments of lymph node tissue with a necrotizing lesion, composed of abundant karyorrhectic debris, fibrinoid necrosis of small arterioles and collection of large mononuclear cells. Features were suggestive of kikuchi`s lymphadenitis. The biopsy specimen was also sent for AFB smear and AFB PCR which came out to be negative. He was also tested to rule out autoimmune etiology (ANA, Anti dsDNA), which came out to be negative.
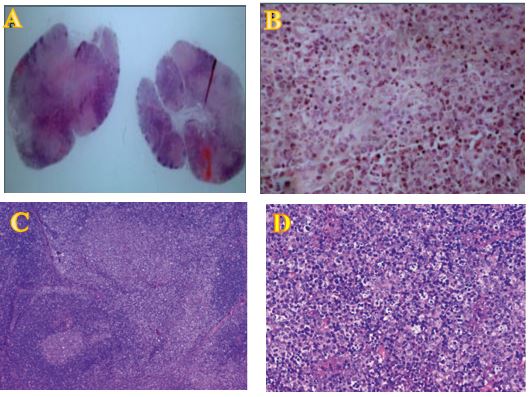
Figure1: (A) Gross view of the node shows hypercellular areas alternating with hypocellular areas. A few germinal centers and hemorrhage are evident. (B) Fragmented nuclei, many histiocytes, and necrosis without prominent neutrophils are evident in the hypocellular areas (x 400, H & E) Histopathologic examination showing patchy areas of necrosis, numerous histiocytes, and apoptotic cellular debris. (C) H&E, 20x. (D) H&E, 400x.
The patient was treated symptomatically with NSAIDs (Non-steroidal anti-inflammatory drugs), and his symptoms of malaise, fatigue and decreased appetite improved on follow up after 2 months. His mother denied fever and night sweats, and repeat ultrasonography of left cervical lymph node was normal. Laboratory parameters including ESR, CRP and LDH, that were initially deranged, were also within normal range. On 6 months follow up, the patient was asymptomatic.
Discussion
Kikuchi-Fujimoto disease is a rare benign disease which is associated with histiocytic necrotizing lymphadenitis. KFD is endemic in Asia, especially affects young women with only a few cases reported from Europe making its diagnosis very difficult. KFD is usually characterized by symptoms of fever, night sweats and tender lymphadenopathy. The other less common presenting clinical manifestations include generalized lymphadenopathy, weight loss, enlargement of spleen, skin rash, joint pain, decrease in weight, nausea, vomiting and central nervous system involvement. The most commonly involved lymph nodes are cervical, followed by axillary and other lymph nodes. The affected lymph nodes have the characteristic of been solid, mobile, and painful but not been suppurative [6,8]. It is a self-limiting disease which resolves within several months and has a recurrence rate of 3-4% [10]. It commonly affects females under 30 years of age (mean age-29) [11]. We present a case of 7year old boy with a single cervical lymph node presenting with constitutional symptoms.
Two possible etiologies of KFD have been identified: viral and autoimmune. The first one is the viral etiology which consists of a hyper-immune response in genetically susceptible patients. The second one is the autoimmune etiology likely because of the relationship between KFD and autoimmune diseases with many reports referring KFD as an early stage of SLE [6]. In our study, both viral as well as autoimmune serology was unremarkable (ANA=negative). There also have been implication of Bacteria and parasites have in the pathogenesis of KFD with controversial results [12,13].
No specific laboratory tests or instrumental examination can suggest a diagnosis of KFD. The usual laboratory alteration in KFD includes leukopenia occasionally with atypical peripheral blood lymphocytes, anemia, or increased inflammatory markers [14,15]. Rise in LDH and transaminases may rarely be seen. In our patient, we had increase in inflammatory markers such as ESR and CRP along with increase in LDH while Liver enzymes were normal.
No imaging feature is diagnostic of KFD and it is sometimes difficult to distinguish KFD from lymphoma and other nodal diseases with necrosis. The finding of distinctive lymphadenopathy pattern consisting of many small clustered lymph nodes can be noted on ultrasounds, CT scan, and magnetic resonance with a carefully interpretation [9,16,17]. There is limited diagnostic accuracy when it comes to Fine-Needle Aspiration Cytology (FNAC) in diagnosing KFD which is approximately 56% [18-20]. Hence, lymph node biopsy is the only way to reach a correct diagnosis of KFD. In our case, we had painful and tender cervical lymphadenopathy, so we suspected glandular fever and other viral etiologies. Ultrasound showed matted lymph node so initially we suspected TB lymphadenitis as well as we live in TB endemic area. Workup for tuberculosis was negative in our case with unrevealing CT Chest, abdomen and pelvis. So, we decided to go for excisional cervical lymph node biopsy which revealed features of Kikuchi`s lymphadenitis that necrotizing tissue, composed of abundant karyorrhectic debris, fibrinoid necrosis of small arterioles and collection of large mononuclear cells.
Despite of advances in medical sciences, no definitive treatment for KFD has been discovered up to date. KFD is usually a self-limiting condition; however, milder disease can be controlled by NSAIDs and antipyretics. Reports also suggest that the use of corticosteroids in case of persistent or more severe symptoms, as in patients with extra nodular involvement, such as the Central Nervous System (CNS) and lungs. The symptomatic patients usually improve with short pulses of corticosteroids with hydroxychloroquine or IV corticosteroids reserved for unresponsive patients or patients with complicated diseases. The best treatment options include alternating high-dose corticosteroids and IV immunoglobulin .5 In our case, treatment with NSAIDs was commenced after the histological results were obtained because of persistence of fever, fatigue, and night sweats. At 2 months follow up, the patient demonstrated improvement in clinical and laboratory parameters while at six-month follow-up, the patient was asymptomatic.
So, we highlight here that KFD is a rare disease that sometimes proves to be a diagnostic dilemma. It should be kept in mind in the differential diagnosis of lymph node enlargement because it has an altogether different therapeutic approach as compared to other entities and misdiagnosis can lead to polypharmacy or unnecessary treatment [9,21]. Various differential diagnosis should be considered along with KFD which include infections, Granulomatous lymphadenitis, connective tissue diseases, and lymphoproliferative disorders [9,22].
This is the first case which has been reported from Pakistan, especially in a young boy which is against the odds as it is the disease which is more common in females and has autoimmune etiology
Conclusion
In conclusion, we report a case of 7 years young boy diagnosed with KFD on cervical lymph node biopsy and was treated with Non Steriodal Anti-Inflammatory Drugss (NSAIDs) and was symptom free at 6 months interval.
So, KFD can be a diagnostic dilemma and therefore a wide range of other differentials should be kept in mind while considering KFD as a diagnosis.
Conflict of Interest: None
References
- Kikuchi M. Lymphadenitis showing focal reticulum cervical hyperplasia with nuclear debris and phagocytes. Acta Hematol Jpn, 1972; 35: 379–380.
- Fujimoto Y, Kojima Y, Yamaguchi K. Cervical subacute necrotizing lymphadenitis. Naika, 1972; 30: 920-927.
- Sopena B, Rivera A, Vazquez-Trinanes C, Fluiters E, Gonzales-Carrero J, Del Pozo M, et al. Autoimmune manifestations of Kikuchi disease. Semin Arthritis Rheum, 2011.
- Chiu CF, Chow KC, Lin TY, et al. Virus infection in patients with histiocytic necrotizing lymphadenitis in Taiwan. Detection of Epstein-bar virus, type I human T cell lymphotropic virus, and parvovirus B19. Am J Clin Pathol, 2000; 113: 774–781.
- Deaver D, Horna P, Cualing H, Sokol L. Pathogenesis, diagnosis, and management of Kikuchi-Fujimoto disease. Cancer Control, 2014; 21: 313–321.
- Bosch X, Guilabert A, Miquel R, Campo E. Enigmatic Kikuchi-Fujimoto disease: a comprehensive review. Am J Clin Pathol, 2004; 122: 141–152.
- Longaretti P, Savasta S, Caimmi D, et al. Kikuchi-Fujimoto Disease Complicated by Peripheral Neuropathy. Pediatr Neurol, 2012; 46(5): 319–321.
- Kukukardali Y, Solmazgul E, Kunter E, et al. Kkikuchi-Fujimoto disease: analysis of 244
cases. Clin Rheumatol, 2007; 26: 50–54. - Bosch X, Guilabert A, Miquel R, Campo E. Enigmatic Kikuchi Fujimoto disease: a comprehensive review. Am J Clin Pathol, 2004; 122: 141–152.
- Hutchinson CB, Wang E. Kikuchi-fujimoto disease. Arch Pathol Lab Med, 2010; 134(2): 289–293.
- Menasce LP, Banerjee SS, Edmondson D, Harris M. Histiocytic necrotizing lymphadenitis (Kikuchi-Fujimoto disease): continuing diagnostic difficulties. Histopathology 1998; 33: 248–254.
- Bosch X, Guilabert A. “Kikuchi-Fujimoto disease,” Orphanet Journal of Rare Diseases, 2006; 1(1): p. 18.
- Chong Y, Kang CS. “Causative agents of Kikuchi Fujimoto disease (histiocytic necrotizing lymphadenitis): a meta-analysis,” International Journal of Pediatric Otorhinolaryngology, 2014; 78(11): pp. 1890–1897.
- Lin YW, Horiuchi H, Ueda I, Nambu M. “Recurrent hemophagocytic lymphohistiocytosis accompanied by Kikuchi’s disease,” Leukemia and Lymphoma, 2007; 48(12): pp. 2447–2451.
- Cheng CY, Sheng WH, Lo YC, et al. “Clinical presentations, laboratory results and outcomes of patients with Kikuchi’s disease: emphasis on the association between recurrent Kikuchi’s disease and autoimmune diseases,” Journal of Microbiology, Immunology and Infection, 2010; 43(5): pp. 366–371.
- Bennie MJ, Bowles KM, Rankin SC, “Necrotizing cervical lymphadenopathy caused by Kikuchi-Fujimoto disease,” British Journal of Radiology, 2003; 76(909): pp. 656– 658.
- Kwon SY, Kim TK, Kim YS, Lee KY, Lee NJ, Seol HY. “CT? findings in Kikuchi disease: analysis of 96 cases,” American Journal of Neuroradiology (AJNR), 2004; 25(6): pp. 1099–1102.
- Miller WT Jr, Perez-Jae LA, “Cross-sectional imaging of Kikuchi disease,” Journal of Computer Assisted Tomography, 1999; 23(4): pp. 548–551.
- Tong TR, Chan OW, Lee KC. “Diagnosing Kikuchi disease on one needle aspiration biopsy: a retrospective study of 44 cases diagnosed by cytology and 8 by histopathology,” Acta Cytologica, 2001; 45(6): pp. 953–957.
- Das DK, Haji BI, Al-Boijan RA, et al. “Kikuchi-Fujimoto disease in one needle aspiration smears: a clinico-cytologic study of 18 pediatric cases and correlation with 68 adult patients,” Indian Journal of Pathology and Microbiology, 2012; 55(3): pp. 333–338.
- Kodet R, Campr V, Kalinova M, Kamaradova K, Mrhalova M, Soukup J. Histiocytic necrotizing lymphadenitis/KikuchiFujimoto disease (HNL/K-F) and its differential diagnosis: analysis of 19 patients. Cesk Patol, 2012; 48: 198–206.
- Uslu E, Gurbuz S, Erden A, Aykas F, Karagoz H, Karahan S, et al. Disseminated intravascular coagulopathy caused by Kikuchi-Fujimoto disease resulting in death: first case report in Turkey, Int Med Case Rep J 2014; 7: 19–22.

