Alagille syndrome - A Rare Clinical Entity in an Eight-Year-Old Girl Presenting in Hepatobiliary Clinic in Pakistan
Hina Ismail, Ghous Bux Soomro, Raja Taha Yaseen Khan*, Farrah Hanif, Arshad Ali Jariko, Mahboob Jan, Danish kumar and Nasir Hasan Luck
Department of Hepatogastroenterology, Sindh Institute of Urology and Transplantation, Pakistan
Received Date: 14/03/2022; Published Date: 25/03/2022
*Corresponding author: Raja Taha Yaseen Khan, Department of Hepatogastroenterology, Sindh Institute of Urology and Transplantation,Karachi, Pakistan
Abstract
Alagille Syndrome (AGS) is a rare multi-systemic genetic disorder affecting liver, face, eye, heart, skeleton, kidneys and blood vessels. A diagnosis of AGS is made on paucity of intrahepatic bile ducts on liver biopsy and the presence of three out of five clinical criteria’s i.e., cholestatic jaundice, congenital heart disease, characteristic facial facies, skeletal abnormalities and ocular abnormalities. Here, we have described a case of an eight-year-old girl presenting in the hepatobiliary clinic with jaundice and fulfilling four out of five major features of this syndrome.
Keywords: Alagille syndrome, genetic disorder, bile duct paucity
Introduction
Alagille Syndrome (AGS) is a rare disorder, inherited in an autosomal dominant fashion. It is also known as hepatic ductular hypoplasia. It is associated with a mutation in jagged -1 (JAG1) or notch-2(NOTCH2) [1-2]. AGS involves multiple system of the body including the heart, liver, eyes, bone, face and to a lesser extent also involves the kidneys and pancreas [3]. In most cases symptoms of AGS are usually manifested in pediatric group [4].
A diagnosis of AGS is made on paucity of intrahepatic bile ducts on liver biopsy and the presence of three out of five clinical criteria which includes cholestatic jaundice, congenital heart disease( primary pulmonary stenosis),characteristic facial facies ( broadened forehead, pointed chin, and elongated nose with bulbous tip ),skeletal abnormalities (butterfly shaped vertebrae), and ocular abnormalities( posterior embryotoxon,axenfeld anomaly) [1,5]. The frequency of AGS is 1 case in every 100,000 live births [6].
Here, we have described the case of an eight-year-old girl presenting with cholestatic jaundice in our paediatric hepatobiliary clinic.
Case Report
A 8 years old girl, presented with history of jaundice at birth which was resolved after one week. However, at 40 days of life she again developed jaundice associated with clay colored stool. She also had history of intermittent bleeding from nose for the past 3 years. On examination, she was icteric and pale, having characteristic facial features in the form of triangular face with broad forehead, pointed chin and elongated nose.
On abdominal examination liver is palpable below the right costal margin along the mid clavicle line with a span of 10cm. An eye examination revealed EUA (Posterior embryotoxon, fullness in both eyes, optic disc drusen, peripheral fundus appears as white without pressure). Neurological and respiratory findings were within normal limits. Her laboratory parameters at the time of presentation were Hemoglobin (Hb) of 9.6g/dl, Mean Corpuscular Volume (MCV) of 57fL, total leukocyte count (TLC) of 9.4x109/L and platelet count of 342x 109/l. Liver function test disclosed a total bilirubin of 22.2mg/dl, direct bilirubin of 14.7mg/dl, alkaline phosphatase of 685 U/L, alanine aminotransferase of 438 U/L, aspartate aminotransferase of 729 U/L and gamma glutamyl transferase of 229 U/L serum albumin of 3 g/DL. The international normalized ratio was 1.16. Viral markers were negative (HBsAg and HCV). Her ultrasound abdomen depicted slightly enlarged liver, coarse texture, regular margins with no space occupying lesion or intra hepatic ductal dilatation, normal spleen and no ascites. HIDA scan demonstrated reduced hepatocyte uptake and poor clearance with non-visualization of common bile duct, gall bladder and gut activity. Findings suggestive of reduced hepatocellular functions with non-visualization of biliary tree. She underwent liver parenchymal biopsy, which showed patchy area of both hepatocellular and canalicular cholestatsis in the form of bile plugs along with feathery degeneration of hepatocytes and mild focal septal fibrosis is seen with features suggestive of paucity of intrahepatic bile ducts (Figure 1). Two-dimensional echocardiography revealed peripheral pulmonary artery stenosis with small ASD with left to right shunt.
Based on the above findings, our patient was being managed as a case of AGS. She was treated with Ursodeoxycholic acid, vitamin D3, and multivitamins supplements, folic acid, vitamin A and multivitamins. Her parents were advised for regular follow-up appointments. She took proper treatment and is being followed up for 11 years. Her symptoms are markedly improved. Her current investigations are Hb of 10.3 g/dl, mean corpuscular volume of 59fL, TLC of 6.3x109/L and platelet count of 125 x 109/L. Total bilirubin of 2.71mg/dl, direct bilirubin of 1.27mg/dl, alkaline phosphatase of 538 U/L, ALT of 156 U/L, AST of 119 U/L, GGT of 184 U/L along with serum albumin of 3.39 g/dL. The international normalized ratio was 1.08.
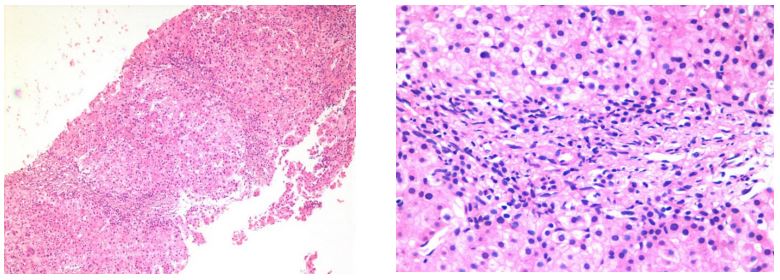
Figure 1: showing paucity of intrahepatic bile ducts (A): Low power scanner view (B): High power view showing patchy area of both hepatocellular and canalicular cholestasis in the form of bile plugs and feathery degeneration of hepatocytes with mild focal septal fibrosis.
Discussion
AGS also known as hepatic ductular hypoplasia is a rare disorder with an incidence rate of nearly 1 in every 100,000 live birth [6]. The diagnostic criteria of AGS are fullfiled if three or more of the below mentioned major features are seen i.e. characteristic facial appearance, posterior embryotoxon, butterfly shaped vertebrae, bile duct paucity on liver biopsy, cardiac murmurs and renal abnormalities.5 Around 500 cases have been reported since now. No case report has been reported from this part of the world. Although, there are few cases that have been reported from neighboring countries [7]. AGS is inherited in an autosomal dominant pattern, caused by defects in the NOTCH signaling pathway, which affects multiple organs of the body [1,2]. Most children are presented in early infancy with either cardiac murmur or neonatal jaundice; but afterwards they may be evaluated for ocular abnormalities, linear growth, dysmorphic faces, skeletal and renal manifestations, but hepatic disorders being the most common presentation in AGS [5]. Mental retardation is also seen in certain cases [8].
Our case had four out of five major features of the syndrome with no vertebral defect. She had characteristic facies (triangular face with broad forehead, pointed chin and enlongated nose), cholestatic jaundice, bile duct paucity on histology, cardiac murmur. Our limitation was that she did not undergo genetic testing for JAG1 and NOTCH2 receptor gene due to unavailability of genetic testing in our setup.
Conclusion
Alagille syndrome is a rare systemic disorder causing paucity of interlobular bile ducts. The involvement of multisystem has made it necessary for all clinicians to be aware of this rare disease as this can help in timely referral of this grave disease to a tertiary care center for multidisciplinary approach involving hepatologists, ophthalmologists and surgeons with expertise in hepatobiliary diseases.
References
- Krantz ID, Colliton RP, Genin A, et al. Spectrum and frequency of jagged1 (JAG1) mutations in Alagille syndrome patients and their families. Am J Hum Genet. 1998; 62(6): 1361-1369.
- Li L, Krantz ID, Deng Y, et al. Alagille syndrome is caused by mutations in human Jagged1, which encodes a ligand for Notch1. Nat Genet. 1997; 16(3): 243-251.
- Alagille D, Estrada A, Hadchouel M, Gautier M, Odièvre M, Dommergues JP. Syndromic paucity of interlobular bile ducts (Alagille syndrome or arteriohepatic dysplasia): review of 80 cases. J Pediatr, 1987; 110: 195–200.
- Vajro P, Ferrante L, Paolella G. Clin Res Hepatol Gastroenterol, 2012; 36(3): 275-277.
- Studies of the aetiology of neonatal hepatitis and biliary atresia. Danks DM, Campbell PE, Jack I, Rogers J, Smith ALArch Dis Child, 1977; 52(5): 360-367.
- Emerick KM, Rand EB, Goldmuntz E, Krantz ID, Spinner NB, Piccoli DA. Features of Alagille syndrome in 92 patients: frequency and relation to prognosis. Hepatology, 1999; 29: 822–829.
- Studies of the aetiology of neonatal hepatitis and biliary atresia. Danks DM, Campbell PE, Jack I, Rogers J, Smith AL Arch Dis Child, 1977; 52(5): 360-367.
- Pati GK, Singh A, Nath P, Narayan J, Padhi PK, Parida PK, et al. A 10-year-old child presenting with syndromic paucity of bile ducts (Alagille syndrome): a case report. J Med Case Rep, 2016; 10(1): 342.
- Helps, S; Caulfield, C; Chadwick, O; Baker, a cognitive and academic status of children with Alagille syndrome, Journal of Pediatric Gastroenterology & Nutrition: 1998; 26(5): p 576.

