A Perirenal Cystic Lymphangioma in an Adult
Hasan Aydın*, Onur Sımsek and Halil Basar
Department of Radiology, Ankara Oncology Education and Research Hospital, Turkey
Department of Urology, Ankara Oncology Education and Research Hospital, Turkey
Received Date: 13/03/2022; Published Date: 24/03/2022
*Corresponding author: Hasan Aydın, Department of Radiology, Ankara Oncology Education and Research Hospital, Turkey
Abstract
Lymphangiomas are rare, benign tumors mostly resulting from the obstruction of regional lymph drainage.Lymphangioma frequently occurs in the cervical neck and axilla, also in the retroperitoneum, mediastinum, mesentery, omentum, colon, and pelvis, rarely in the perirenal space.Renal lymphangiomas are also rare benign renal lesions which may present with the presence of renal cysts in both renal sinus and the renal parenchyma.Patients have often complaints of hematuria, flank pain, or abdominal pain.
Here,we report a case of perirenal Lymphangioma in an adult woman,found out incidentally in the Abdominal CT.
Keywords: Peri; Renal; Lymphangioma; CT; Abdomen
Introduction
Lymphangioma is a rare, benign mesenchymal neoplasm, which is characterized by numerous intercommunicating cystic spaces containing lymphatic fluid [1,2] They are mostly derived from the congenital malformations of the lymphatic system, most of the cases are presented in children as a soft, cystic mass in the neck and the axilla [1-3].
It is considered to be a congenital disease resulting from the obstruction of regional lymph drainage during the developmental period [1-4] Lymphangioma frequently occurs in the cervical neck and axilla, also in the retroperitoneum, mediastinum, mesentery, omentum, colon, and pelvis, rarely in the perirenal space, abdominal locations which represent less than 10% of the cases, preferentially involve the mesentery [4] Renal lymphangiomas are also rare benign mass-like renal lesions which may refer to the presence of renal cysts in both renal sinus and the renal parenchyma [4,5] The etiology is unknown, but it has been thought to be the result of lymphatic obstruction as seen in perirenal Lymphangiomas,majority of patients have renin-dependent hypertension as the presenting clinical complaint [4].
These tumors usually present in childhood, but they are exceedingly rare in adults Patients often complain of hematuria, flank pain, or abdominal pain. Complications of lymphangiomas have been reported as infection, rupture, or hemorrhage [2-4].
Here,we report a case of perirenal Lymphangioma in a 66 year old woman, found out incidentally with an history of left mastectomy and left axillary dissection.
Case Report
66 year old woman was operated at 25.08.2020 due to a left breast mass and left axillary lymph nodes after neoadjuvant chemotherapy.Histopathological diagnosis was invasive mixed type breast carcinoma(Invasive ductal % 90+ invasive micropapiller type%10) and metastatic lymph nodes.She received adjuvant chemoradiotherapy after mastectomy and discharged with total cure.However, she didn’t come to her follow-up controls during 2021 most probably due to Covid-19 pandemics.
She visited our medical oncology department at February 2022 for the first control after surgery and chemotherapy then referred to our Radiology department for Thorax and Abdominopelvic CT.
In the Thorax CT; Thoracic and mediastinal pathologic lymph nodes were not observed, three to four parenchymal and subpleural pulmonary nodules less than 4 mm in size were existed in both hemithoraxes without any infiltration. A few pleural adhesions were seen in both lung apexes.
In the laboratory analysis; BUN 21 mg/dL Uric acid 6.6 mg/dL Total cholesterol 252 mg/dL with LDL cholesterol 127 mg/dL TSH 0.1988 mg/dL, other biochemical blood profiles were almost normal
As a complete blood count, Hb 12.6 g/dL HTC %38 WBC 4.09 RBC 3.95 Platelet count 178.000 with slight lymphocytosis(%41), minimal neutropenia(%45.3)
In the US; she had no recurrence in the left mastectomy area without any mass lesion in the contralateral right breast and axilla.
In the Abdominopelvic CT; A left perirenal and periurethral 2.5x2 cm in size unilateral well-circumscribed cystic lesion was observed with10-15 Hounsfield Unit density beneath the left psoas muscle.A non-specific 2 cm Bosniac type 1 cortical cyst was seen in the right kidney.Other parameters were in normal range in the Abdominal CT(Figure 1,2).
After urological consultation, this cystic lesion was considered to be lymphangioma (Figure 3,4) with regard to radiological findings without any histopathological proof. Any surgical intervention and/or biopsy were not needed for the diagnosis.
She will be under routine control for her previously operated invasive ductal carcinoma and at the sametime under follow-up for her perirenal Lymphangioma.
Discussion
Three types of lymphangiomas are commonly identified: capillary, cavernous, and cystic. Cystic type is the one commonly found in the abdomen and/or retroperitoneal location, may also be uniloculated or multiloculated [1-4]
All these above mentioned perirenal lymphangiomas have a very low incidence which make them difficult to diagnose, these benign lesions have no sex predilection and have been reported at all ages, from birth to 90 years of age, mostly occur during childhood and over the age of 40 [1,3,5]. Renal lymphangiomas can be diagnosed incidentally by radiological imaging methods or patients may present themselves with lumbar pain or vague abdominal symptoms, other possible clinical manifestations are hypertension, hematuria, proteinuria, intracystic hemorrhage or chyluria [2,4,6]. Lymphangiomas may be widened and symptoms may become exacerbated during pregnancy but, however children may be presented with only nephromegaly and may be associated with obstructive uropathy, lymphangiomas in adults are usually characterized by peripelvic and perirenal thin-walled cysts [1-6].
Perirenal and peripelvic involvements are usually seen in most cases, although some of them may be exclusively perirenal as seen in our patient (Perirenal and periurethral localization).
Generally, diagnosis is acquired by ultrasound(US) and/or CT scan, which are both very sensitive and specific; CT and US show the discrete cystic nature of the lymphangioma with a smooth, thin wall and septa, but sometimes irregular appearance with calcifications, CT appearance of the cyst can vary from water density to higher densities representing an increased mucoid, hemorrhagic fluid and/or calcium [6,7]. At MRI, lymphangiomas appear heterogenous low signal intensity on T1-weighted images and high signal intensity on T2-weighted images with interseptated masses, but may present differentiating signals secondary to varying amounts of protein or hemorrhage [6-8].
The differential diagnosis of cystic lymphangioma includes:Policystic kidney disease, tumors such as liposarcoma,fibrosarcoma,leiomyosarcoma,malignant teratomas and multilocular cystic nephroma, which are predominantly cystic or necrotic, but these malignancies usually contain substantial solid components; abscess and urinoma may also produce a similar appearance, but almost all these conditions can be differentiated with the help of clinical history, normal biochemical parameters and with typical radiological imaging findings of perirenal and parapelvic involvement sparing the renal parenchyma [3,5,8-10] Endoscopic ultrasound guided fine needle aspiration is recommended in some previous reports, which may aid to the definitive diagnosis and further guide to the subsequent therapeutic strategies, the choice of treatment depends on type, size and location of the cyst.If lymphangiomas of the kidney are small and do not cause any symptoms, they don’t need to be surgically treated, because of their benign natures [2,5,9,11].
Surgery is often required to deteriorate symptoms and for definitive diagnosis, since radiological studies are often unable to differentiate lymphangiomas from other cystic tumoral growths.Nevertheless, the sacrifice of adjacent structures must be avoided, and in difficult cases surgical interventions and non-surgical methods such as sclerotherapy, may be combined together sequentially [2,9,11] Surgical excision can be performed via either laparotomy or laparoscopy and injection of sclerosing agents into lymphangioma has been indicated in the relevant literature for non-surgical candidates. The optimal satisfactory treatment is complete surgical excision,resulting an excellent prognosis [9,11].
In our case, A left perirenal and periurethral cystic lesion, named to be Lymphangioma was discovered incidentally in the Abdominal CT.She had no specific complaints for perirenal Lymphangioma and routine follow-up for this cystic lesion was recommended as uroradiological approach did not indicate any surgical methods and/or sclerosing therapy.

Figure 1: In the contrast-enhanced axial CT; A cystic mass lesion was seen on left perirenal space beneath the left psoas muscle.
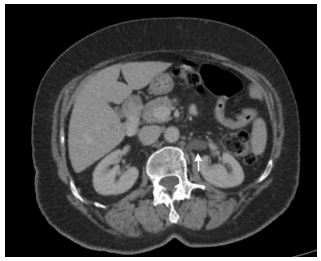
Figure 2: In the consecutive slice, same cystic lesion was identified on the left retroperitoneal area.

Figure 3: 0/-15 HU density was measured inside the cystic lymphangioma in the axial CT.
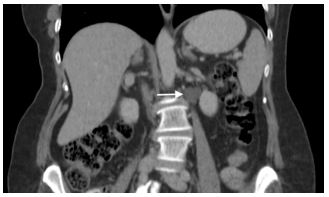
Figure 4:Left cystic lymphangioma was visualized in the left paravertebral space, superposing to the left psoas muscle in the coronal CT.
Conclusion
Lymphangiomas are rare, benign tumors mostly resulting from the obstruction of regional lymph drainage They frequently occur in the cervical neck and axilla, also in the retroperitoneum, mediastinum, mesentery, omentum, colon, and pelvis, rarely in the perirenal space.
Our case is a perirenal cystic Lymphangioma, diagnosed incidentally by Abdominal CT, surgical excision is not needed, conservative follow-up of lesion is recommended as a therapeutic choice in this patient.
References
- Honma I, Takagi Y, Shigyo M, Sunaoshi K, Wakabayashi J, Harada O, et al. Lymphangioma of the kidney. Int J Urol, 2002; 9(3): 178-182.
- Chaabouni A, Rebai N, Fourati M, Rekik S, Chabchoub K, Slimen MH, et al. Cystic lymphangioma of the kidney: Diagnosis and management. Int J Surg Case Rep, 2012; 3(12): 587-589.
- He W, Hao YC, Xia HZ, Ma RZ, Yang B, Lu J. Perirenal cystic lymphangioma in an adult: a case report and literature review]. Beijing Da Xue Xue Bao Yi Xue Ban, 2017; 49(4): 730-732.
- Yamaguchi Y, Kinouchii T, Yasuhara Y, Kakimoto K, Ono Y, Meguro N, et al. Renal lymphangioma: report of a case. Hinyokika Kiyo, 2007; 53(2): 113-115.
- Liedtke KR, Käding C, Döring P, Bekeschus S, Glitsch AS. A case of giant retroperitoneal lymphangioma and IgG4-positive fibrosis: Causality or coincidence? SAGE Open Med Case Rep, 2021; 9: 2050313X211016993. doi: 10.1177/2050313X211016993
- Chua N, Wolfe K, Mehta S, Lodge RN, Liyanage SH. Triparametric ultrasound in differentiating multicystic renal masses: a rare presentation of unilateral focal renal lymphangioma. Radiol Case Rep, 2017; 12(4): 731-737.
- Sarikaya B, Akturk Y, Bekar U, Topaloglu S. Bilateral renal lymphangiomatosis mimicking hydronephrosis: multidetector CT urographic findings. Abdom Imaging, 2006; 31(6): 732–734.
- Rezaee ME, Alexakos SG, Taylor CE, Santis WF. A rare case of a retroperitoneal lymphangioma causing chronic flank pain in an adult..Urol Case Rep. 2020; 33: 101408. doi: 10.1016/j.eucr.2020.101408.
- Wadhwa P, Kumar A, Sharma S, Dogra PN, Hemal AK. Renal lymphangiomatosis: imaging and management of a rare renal anomaly. Int Urol Nephrol, 2007; 39(2): 365-368.
- Jung HI, Ahn T, Son MW, Kim Z, Bae SH, Lee MS, et al. Adrenal lymphangioma masquerading as a pancreatic tail cyst.World J Gastroenterol, 2014; 20(36): 13195-13199.
- Kumar N, Yadav P, Ansari MS, Lal H. Surgical management of giant retroperitoneal lymphangioma in a child..BMJ Case Rep, 2020; 13(2): e234447.

