Effect of Deep Dry Needling on Spasticity in Traumatic Brain Injury
Olaf R. van Loon*, A.J. (Tom) van Loon, Peter S. Sándor
ZURZACH Care, Early Rehabilitation Department, Hospital Baden, Switzerland
Shandong University of Science and Technology, China
Department of Neurology, University Hospital Zürich, Switzerland
Received Date: 28/02/2022; Published Date: 15/03/2022
*Corresponding author: Olaf R. van Loon, ZURZACH Care, Early Rehabilitation Department, Hospital Baden, Im Ergel 1, 5400 Baden, Switzerland
Abstract
This observational case study was carried out to estimate the effect and document tolerability of a series of Deep Dry Needling (DDN) interventions on the spasticity of a 20-year-old man who suffered from brain injury after an accident that also had caused several fractures in the face region, the pelvis and his right femur. DDN treatment of a subject with such severe injuries at such an early stage of recovery had not been documented. A pre-intervention test was performed to record baseline values, and the same aspects were measured again during the treatment, directly after, and approximately one year after the last intervention. DDN was well tolerated and without complications. Outcomes of the DDN treatment were assessed via (i) the Tardieu scale and (ii) ROM measurements as well as close clinical monitoring to assess tolerability. The assessment showed - within 3 weeks - a decrease of spasticity of 1-2 points according to the Tardieu scale, and an increase in ROM in all treated joints, which lasted until an assessment after one year. We conclude that DDN was well tolerated and might have significantly contributed to recovery from the extension synergy, with long lasting benefit.
Keywords: Deep Dry Needling; Dry Needling; Spasticity; Early rehabilitation
Introduction
Spasticity is often a major problem in early rehabilitation. Pharmacological therapy can be limited by its sedative effects, interfering with a patient’s therapy. Deep Dry Needling (DDN) is an emerging non-pharmacological technique which can be applied to reduce spasticity without the side effects of pharmacotherapy, but has, to the best of our knowledge, not been reported before in the context of early rehabilitation. Here we describe how DDN was applied to effectively reduce spasticity with minimal interference with therapeutic activities in the case of an early rehabilitation patient with severe traumatic brain injury.
Case
The present study concerns a 20-year-old patient who suffered from severe traumatic brain injury and a number of other traumas due to a paraglider accident.
In addition to his severe brain injury (detailed below), there was a luxation of his anterior inferior shoulder, several fractures (orbital floor/blow-out fracture, fractures of the left maxillary sinus, left caput mandibulae, pelvis, and femur), and extension synergy with shortening of the extensor muscles (particularly of the triceps brachii, the rectus femoris, the gastrocnemius, soleus, and the flexion as well as extension muscles of the forearm and the fingers flexors). Furthermore, there were complications during the acute hospital stay such as trachea-bronchitis after ventilator treatment, and a proximal deep venous thrombosis in his left lower leg.
His brain injury included wide-spread shearing injuries and small bleeds including both hemispheres globally, but also the basal ganglia and the brainstem along with bihemispheric subacute ischemic lesions in mesiotemporal and temporo-occipital localization. The brain injury resulted in initial coma (with GCS of 5) while in the acute hospital and subsequently, with gradual transformation into the clinical picture of a minimally conscious state associated with severe autonomous dysregulation, including tachycardia, hypertension and hyperthermia in the context of phases of pronounced sympathetic activation. Symptomatic pharmacotherapeutic measures were effective, but associated with significant sedative side effects. In the course of early rehabilitation, stabilization could be achieved. The management of the chronic tracheostomy was largely uneventful.
Therapies and clinical course
The patient was treated according to standard care during early rehabilitation in our group of hospitals, ZURZACH Care. This included a minimum of two hours of direct therapeutic treatment as well as two hours of therapeutic care by nurses, fragmented into periods of 15 to 45 minutes. The direct therapeutic treatment consisted of at least two sessions a day from a physical therapist, commonly in the form of team treatment by two physical therapists or a physical and an occupational therapist; the latter was sometimes replaced by a speech/dysphagia therapist, mainly for chronic tracheostomy management.
After the transfer from the acute hospital to the early rehabilitation unit, moderate and increasingly severe spasticity became apparent, predominantly in his right triceps brachii, which was treated pharmacologically with antispastic agents but limited due to significant sedation.
Therefore, DDN treatment was started eight weeks after the accident in order to reduce spasticity and increase the passive range of movements (ROM) without the sedative side effects of antispastic medication. Tolerability of DDN was assessed by motor and verbal reactions and validated by the mother who was present during the initial therapy sessions. Once established, the treatment frequency for DDN was three times per week with a duration of about thirty minutes per session, for about four weeks.
The therapies to treat spasticity included mobilization both at bedside and in a passive wheelchair, and subsequently also in a functional standing frame [1], as well as additional muscle tone reducing measures by both the physical and occupational therapists.
Before our therapies, the patient had extension synergies, and the extremities could be taken out of the extension only for 10-20° from the fully extended joints; abduction of 30° was the maximum for the glenohumeral joint. Within the extension synergy, the joints allowed movement of both arms for some degrees (Table 1). Extension synergy was stronger whenever too much input took place, or when a sudden movement or noise was made within a few meters of the patient. The spasticity was measured according to the Tardieu scale (Table 2).
As assessments like the Fugl-Meijer Analysis (FMA) and the Box and Blocks (B&B) tests for the assessment of function were too time-consuming in the clinical context, we used the Tardieu scale and ROM to assess spasticity and the passive ROM before and after treatment.
Table 1: Baseline data of the ROM of the patient before start of the treatment.

Table 2: Baseline data of the patient according to the Tardieu scale before treatment.
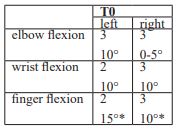
* Exact measurement of all finger joints was impossible; the values indicate best possible estimates when the catch or the clonus started.
Methods
Design and assessment
To provide a measure of the amount of improvement, a pretest-posttest evaluation was designed with assessment at 2-4 points for both arms (T0). Measurements were performed after the first week of treatment (T1) which dealt only with the right side, after the second week of treatment (T2), which dealt only with the left side, and directly after the last intervention (T3). The opportunity to measure the same values about a year after the treatment had finished (T4), was used to quantify the long-term clinical course. All measurements were performed under the same conditions.
Clinical and functional assessment
The clinical assessment was performed for the shoulder abduction (by goniometer measurement). The extension of the elbow, wrist and fingers was measured following the Tardieu scale [2-3]. The ROM of the elbow, wrist and the finger joints was also measured using a goniometer [4-5] (Tables 1, 3); the values for the fingers represent the average values of all finger digits.
Intervention
Dry needling was performed for 30-45 seconds at all points with severe high tone/spasticity, particularly of the taught bands. Most of the points were typically trigger points, but also other points were treated when they showed a severe, high tone. The duration of the total treatment period was four weeks (during the fourth week, the patient was transferred to another rehabilitation center, specialized in long-term care).
Before the actual DDN treatment started, two localizations, one in the right biceps brachii and another in the right triceps brachii were treated (because the traumas of the right side were most severe) to test for both tolerability and local response to DDN treatment. The biceps were chosen because this muscle is easily accessible, and the triceps as this muscle was the most affected by spasticity. As these tests resulted in fast reduction of muscle tension, and because no negative effect was observed by the therapists, the test treatments were followed by the actual, more extensive treatment.
This actual treatment started within the first week with three days (separated by a day of rest) of dry needling treatments of the triceps brachii and the flexors and extensors of the lower arm, only of the right side. This DDN treatment was administered in addition to the daily therapy treatments according to standard care. In the following week, the treatment regime was adapted, after consultation with the head of the department and the family, from exclusively the right side to exclusively the left side. The objective was to validate the results of the treatment of the left side with treatment of exactly the same muscles; it should be noted that the locations of the maximum tones in the left arm were commonly not the same as in the right arm, but the differences were maximally 1-2 cm.
During the final treatment phase (almost two weeks), dry needling treatment was administered again, as in the first week, during three days (again separated by one day of rest). The treatment involved the triceps brachii, the flexor muscles of the lower arm, and the adductor pollicis of both arms.
Results
After the first week (three treatments of the triceps and two treatments of the adductor pollicis; each with two needles), the right arm had become more relaxed; there was less tension, and the ROM in the elbow, the hand and the fingers had improved as compared to the baseline values (Table 3). Also, the shoulders showed an improved range of movement: both shoulders could be abducted for about 90°, and an external rotation of over 30° became possible. The elbows could be flexed to the maximum, but it must be noted that - because of a fracture - the difference in the maximally possible flexion between the left and the right elbows was small. Both pro- and supination were, although rigid in movement, possible to the maximum ROM.
Table 3: Changes in ROM (in degrees) of the patient’s joints before (T0), during (T1 and T2) and after (T3) treatment and one year after treatment (T4).
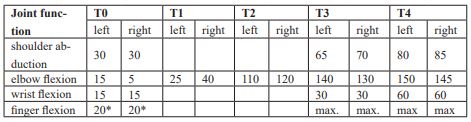
* Exact measurement of all finger joints was impossible; values indicate the best possible estimates.
Table 4: Tardieu measurements before (T0), during (T1 and T2) and after (T3) treatment and 1 year after last treatment (T4).
* A measurement of 0-5° means that the tremor started within a few degrees after starting the movement.
** Exact measurement of all finger joints was impossible; the values indicate the best possible estimates when the catch or the clonus started.
*** During this last assessment, no extension synergy was present anymore. Although there still were differences between left and right, tension was present in the flexor muscles; contracture occurred in the right hand and the lower arm with extension deficits, whereas more muscle activity was present in the left flexion muscles, but without contractures.
With respect to the right arm, it seemed that movements were somewhat more rigid in all joints. Even though no perfect measurement with a goniometer was possible because of the sudden increases in extension synergy, it seemed that a movement of somewhat less than 5° was possible for both arms, but that the ROM of the right arm was smaller than in the left arm.
Maximal finger extension was possible after the last treatment, but dorsal extension together with wrist extension was still less than maximal. The decrease of the muscle tone on the Tardieu scale was still present on the day when the patient was transferred to the subsequent institution - two days after the last treatment (T3).
Discussion
This is the first case describing DDN in a patient with polytrauma including severe traumatic brain injury. Patients with severe injuries are commonly treated according to the national healthcare rules. After a certain degree of recovery, they are treated in a rehabilitation setting. Recently, rehabilitation may include DDN if patients suffer from spasticity, which has shown to be particularly effective in the case of neurological patients. Such DDN treatments are typically started in the course of the rehabilitation process. Currently, DDN treatment is the exception rather than the rule.
In the case of the patient described here, it was decided, after getting informed consent of the family, and in consultation with the Head of Department, to start DDN treatment as soon as the physical examination indicated that DDN treatment could be beneficial for the patient. Studying the outcome and tolerability of such a treatment procedure is important because it might deepen the insight into the possibilities of using DDN to treat spasticity of severely injured patients suffering from brain damage. To assess the effects of the treatment, systematic baseline measurements were followed by measurements after one week and after two weeks, and by final measurements at the end of the treatment period, which lasted almost four weeks. Finally, a follow up took place after a year in order to investigate the long-term effects of the DNN treatment in the context of the clinical course.
Based on the available observations it cannot be decided whether the approach followed was optimal. Nor should it be concluded that the long-term effects must be ascribed exclusively or predominantly to DDN treatment, as the ongoing rehabilitation procedure and the natural course have contributed significantly. It can be concluded, however, that the treatment was very well tolerated without the sedative effects of antispastic pharmacotherapy and that it seemed to have significant positive effects
Therefore, further studies including systematic evaluations seem worthwhile and necessary to estimate the possibilities and limitations of the method. Further, they could contribute toward the development of a practice-based, optimized DNN treatment to be used for severely injured patients with brain damage.
Conclusion
A patient with severe injuries, including severe brain damage, has been treated with DDN in a very early stage of rehabilitation, in order to reduce muscle spasticity. DDN treatment was very well tolerated and without complications. The clinical results were better than expected, with a significant to maximum increase of the ROM of the various joints after a treatment period of four weeks. Spasticity of the various muscles decreased, as expressed by an increase on the Tardieu scale of 1-2 points.
Since no comparable studies have ever been documented, it is still uncertain whether even better results might be obtained by adaptations of the approach followed in the present study, but the results show that DDN is well tolerated and probably helpful for the rehabilitation of severely injured patients with brain damage who suffer from severe spasticity.
Acknowledgements
We thank the patient and his family for permission to publish the case, including the above mentioned details.
References:
- Logan A, Freemam J, Kent B, Pooler J, Creanor S, Vickery, J, et al. Standing practice in rehabilitation early after stroke (SPIRES): a functional standing frame programme (prolonged standing and repeated sit to stand) to improve function and quality of life and reduce neuromuscular impairment in people with severe sub-acute stroke - a protocol for a feasibility randomised controlled trial. Pilot and feasibility studies. 2018; 4: 66.
- Mehrholz J, Wagner K, Meissner D, Grundmann K, Zange C, Koch R, et al. Reliability of the Modified Tardieu Scale and the Modified Ashworth Scale in adult patients with severe brain injury: a comparison study. Clinical rehabilitation. 2005; 19: 751-759.
- Banky M, Williams G. Tardieu scale. Journal of physics. 2017; 63: 126.
- Gajdosik R, Bohannon R. Clinical Measurement of Range of Motion Review of Goniometry Emphasizing Reliability and Validity. Physical therapy., 1988, 67, 1867-1872.
- Van Rijn SF, Zwerus EL, Koenraadt KL, Jacobs WC, Van den Bekerom MP, Eygendaal D. The reliability and validity of goniometric elbow measurements in adults: A systematic review of the literature. Shoulder & elbow. 2018; 10: 274-284.

