Exceptional Retroperitoneal Recurrence of an Unusual Ovarian Tumor 13 Years Later
Hajar El Agouri*, C. Mounjid, S. EchCharif and B. El Khannoussi
Pathology department, Oncology National Institute, Faculty of Medicine and Pharmacy, Mohammed V University, Morocco
Pathology department, Oncology National Institute, Faculty of Sciences, Mohammed V University, Morocco
Received Date: 17/01/2022; Published Date: 31/01/2022
*Corresponding author: EL AGOURI Hajar, Pathology department, Oncology National Institute, Faculty of Medicine and Pharmacy, Mohammed V University, 10100 Rabat, Morocco
Abstract
Sex Cord Tumor with Annular Tubules (SCTAT) is a rare special type of ovarian sex cord-stromal tumor, which has not achieved a standard treatment regimen currently (morphological features intermediate between that of granulosa cell and sertoli cell). Most of ovarian SCTATs are benign and strongly associated with Peutz–Jeghers syndrome (PJS). So far, malignant behavior in SCTAT has been reported only in sporadic cases.
Herein, we show a case of 63-year-old woman who had a history of a conservative surgery for unclassified sex cord-stromal tumor of left ovary. 13 years later, she presented a retroperitoneal metastatic and recurrent SCTAT, based on histopathological and immunohistochemical findings.
Keywords: Sex Cord Tumor with Annular Tubules (SCTAT), Recurrence; Peutz-Jeghers Syndrome (PJS); Malignant
Introduction
SCTAT refers to a rare type of ovarian neoplasm first described in 1970, and it account for only 6% of sex cord stromal tumors [1].
The pathogenesis of SCTAT is still not well-defined. However, PJS has been well-acknowledged as an important cause and reported in one third of cases [2].
Both sporadic and associated with PJS have been reported in patients ranging in age from childhood to old age, with symptoms of hyperestrogenism [3]. While most PJS-related SCTAT is benign, 20% of the sporadic subtype is malignant [2].
Surgery is the major treatment option for SCTAT associated with or without PJS.
Given its rarity, there remains no standard protocol for management of SCTAT, and surgical resection is known to be the cornerstone of treatment. Although unilateral salpingo-oophorectomy is curative, recurrence constitutes an important issue [4].
The aim of this case report is to provide criteria of pathological diagnose of SCTAT and highlight supervision of recurrent advanced malignant SCTAT.
Case Report
The patient was a 63-year-old woman, nulligest. Her surgical history included previous hysterectomy with bilateral salphingo-oopherectomy for fibroid uterus and malignancy of ovary 13 years back. Histopathological examination revealed leiomyoma of uterus with unclassified sex cord-stromal tumor of ovary. The tumor was staged as stage 1A by using the International Federation of Gynecology and Obstetrics (FIGO) staging system. No adjuvant treatment was administrated, and the patient was lost of view.
13 years following diagnosis, the patient presented to surgical department with abdominal and pelvic pain for 6 months. Clinical examination revealed abdominal distension without organomegaly. Ovarian serum tumor markers were normal. Abdominal and pelvic MRI showed a large retroperitoneal mass lateralized to the right, just below the right kidney, with a heterogeneous appearance and central necrosis. It measured 130x110x60mm, with no evidence of invasion of adjacent structures, suggesting primarily a retroperitoneal paraganglioma (Figure 1).
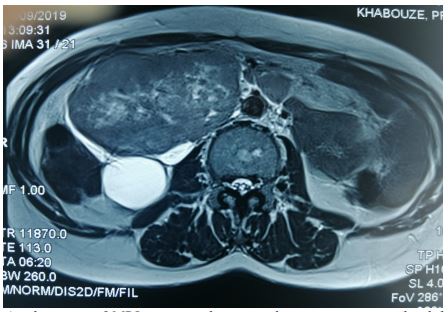
Axial section of MRI imaging showing a large retroperitoneal solid mass (130x110x60mm) with a heterogeneous appearance and no evidence of invasion of adjacent structures
The patient underwent a large excision of tumor. We discovered in laparotomy a voluminous retroperitoneal left encapsulated mass, intimately attached to the psoas major muscle, aorta, left kidney, and the left mesocolon, without invasion of these structures. The spleen and liver were normal. No ascites was objectified. We realized en bloc resection.
The surgical resection specimen was processed routinely in the pathology department. Macroscopically, the tumor was multilobulated, tan-colored with a smooth capsule and areas of hemorrhage. The histopathological examination revealed a tumor proliferation characterized by complex annular tubules variably sized and coalescent nest of tumor cells. There were multiple intercommunicating rings around hyaline basement-membrane like material (Figure 2A and 2B).
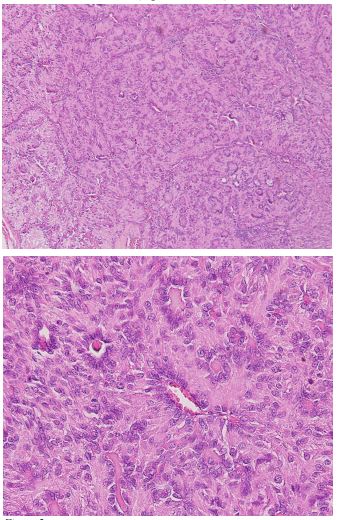
Figure 2:Photomicrograph showing tumor proliferation characterized by com- plex annular tubules with intercommunicating rings revolving around hyaline basement-membrane like material. (hematoxylin and eosin stain; original magnification ×100: Fig 2A, x400: Fig 2B)
The cytoplasm was eosinophile and granular. The nuclei were round or ovoid, showed antipodal distribution within the tubules, and containing pale chromatin, without pleomorphism or mitosis.
There was no germ cell component, tumor necrosis, or calcifications. The tumor capsule was not breached. The diagnosis of SCTAT recurrence was evoqued.
Immunohistochemical staining revealed that tumor cells were strongly positive for inhibin, and calretinin (Figure 3A and 3B). Thus, the diagnosis of retroperitoneal recurrence of SCTAT was made.
The patient was reexamined and reinvestigated to discard Peutz-Jeghers syndrome. There was no family history of PJS or gastrointestinal cancer. General physical examination and gastrointestinal endoscopy ruled out syndromic SCTAT.
The patient received postoperative chemotherapy, and did not show any other metastatic localization during 1 year of follow-up

Figure 3: Photomicrograph showing strong and diffuse staining of tumor cells to Inhibin (Fig 3A) and Calretinin bodies (Fig 3B)
Discussion
SCTAT has low malignant potential with late recurrence. It was first described by Scully in 1970 as a specific form of ovarian neoplasm, characterized by the coexistence of simple and complex annular tubules [1]. The predominant component of this tumor has intermediate morphologic features between granulosa cell tumors and Sertoli cell tumors with possible focal differentiation into either of these tumor types.
The classification of SCTAT is controversial. In the past, SCTAT have been placed in the category of unclassified sex cord-stromal neoplasms. In the recently published classification of tumors of female reproductive organs by WHO, SCTAT was classified as pure sex cord neoplasms [5].
Since Scully described it, numerous case reports and series have contributed to the better understanding of this unusual morphological entity. There are two forms of SCTAT, which differ in terms of association to PJS, the age of onset, initial presentation and its nature. Firstly, SCTAT related to PJS are usually benign with a genetic predisposition, in which the tumors usually showed small, bilateral, multifocal, and calcified lesions [6]. Secondly, sporadic SCTAT are not associated to PJS, in which the tumors generally present as large, unilateral, solitary, and non-calcified neoplasms. Based on the tumor characteristics and the absence of PJS features, our patient likely harbored sporadic SCTAT.
Recurrence of sporadic SCTAT ranges from 8.5% to 46.2% [7]. The latency period ranges from 3 months to 20 years. Most recurrence occurs at pelvic, para-aortic and supraclavicular lymph nodes and metastasize to retroperitoneum, parietal and visceral peritoneum, lung, liver, and kidney [10].
In our reported case, the disease spread through retroperitoneum 16 years after initial diagnosis.
The majority of SCTAT arise in reproductive age patients [2]. Rare pediatric cases have been reported [8,9].
The most frequent clinical manifestations of SCTAT relate to estrogen-progesterone secretion like: menorrhagia, postmenopausal bleeding, precocious puberty, and sterility. In the present case, the patient was in reproductive age group and though did not have any clinical features of high estrogen production; she had symptoms related to the voluminous retroperitoneal mass.
SCTAT’s have been rarely reported in literature. It remains a clinical complexity and preoperative diagnosis is difficult. Although most of the SCTAT are picked up by advanced imaging, the diagnosis is ultimately made by pathological examination.
In both syndromic and non-syndromic cases, the distinctive histologic findings of SCTAT include the presence of simple and complex annular tubules encircling central hyaline cores, and antipodal arrangement of the nucleus 5, as it was objectified with our patient. Nuclear atypia and mitotic figures are otherwise not common features. In PJS lesions, extensive calcifications may be seen. On immunochemistry, the tumor cells are typically positive for calretinin, inhibine, and WT1. On the other hand, they are typically negative for EMA and CD10 [5].
A number of sex cord-stromal tumours including granulosa cell tumour, Sertoli–Leydig cell tumour, and gonadoblastoma should be taken into account for differential diagnosis of SCTATs [8]. However, these tumors may share some of the components that are found in SCTATs.
Given its rarity, there is no standardized management algorithm worldwide, and the surgical total resection (with preservation of fertility if possible) is known to be the only way to influence positively the prognosis and save patient lives [10]. The role of adjuvant treatment is reported for disease control, but preventing recurrence is still unproven [9].
In the present case, hysterectomy with bilateral salphingo-oopherectomy was performed (stage 1) and was apparently well on 6 months follow-up period for after which she was lost to follow-up.
The prognosis is excellent because most of patients have stage I disease at presentation as our patient. But Long-term follow-up is mandatory in such type of tumor because of the high risk of recurrence [7].
Conclusion
SCTAT is a slow-growing ovarian tumor that may exhibits malignant behavior with recurrent and metastatic potential, although many years following initial diagnosis. The anatomopathological diagnosis is the key and it should be included in the differential diagnosis of sex cord tumors.
The exact behavior and long-term prognosis in these patients are almost unknown. Thus, a long-term follow-up is highly recommended.
Author’s Contributions
All authors read and approved the final manuscript and were involved in the review and editing of the manuscript.
Grant Information
The authors received no specific funding for this work.
Informed Consent
Written and Verbal consent was attained from the patient for this manuscript.
Conflicts of Interest
The authors declare that there is no conflict of interests regarding the publication of this paper.
References
- Scully RE, Sobin LH. Histological typing of ovarian tumors. In: (World Health Organization international histological classification of tumors.). 2nd ed. Berlin: Springer, 1999.
- Young RH, Welch WR, Dickersin GR, Scully RE. “Ovarian sex cord tumor with annular tubules. Review of 74 cases including 27 with Peutz-Jeghers syndrome and four with adenoma malignum of the cervix,” Cancer, 1982; 50(7): pp.1384–1402.
- Kulkarni N. Recurrence of Non-Syndromic Sex Cord Stromal Tumor with Annular Tubules of Ovary: Case Report. Iran J Pathol, 2015; 10(1): 61-64.
- Li C, Aishajiang R, Teng Y, Xu T, Ding L, Dong L. Non-Peutz-Jeghers syndrome-associated ovarian sex cord tumor with annular tubules treated by radiotherapy: a case report and literature review. J Int Med Res, 2021; 49(3).
- WHO classification of tumours of female reproductive organs. 5eme edition: International Agency for Research on Cancer; 2020.
- Pesce F, Devouassoux-Shisheboran M. Les tumeurs héréditaires de l’ovaire vues par le pathologiste [The pathology of hereditary ovarian tumors]. Ann Pathol, 2020; 40(2): 85-94.
- Qian Q, You Y, Yang J, et al. Management and prognosis of patients with ovarian sex cord tumor with annular tubules: a retrospective study. BMC Cancer, 2015; 15: 270.
- Yahaya JJ, Mshana D, Mremi A. Ovarian sex cord tumour with annular tubules in a 13-year-old female: a case report. Oxford medical case reports, 2020; 2020(4): omaa024.
- Kwong LT, Kwok YF, Hui HF, Wong LM, Tina WS Lau. Ovarian sex cord stromal tumor with annular tubules in a 7-year-old child: A case report, Gynecologic Oncology Reports, 2019; 30.
- Zheng Ping, et al. “A recurrence of advanced malignant sex cord tumor with annular tubules: case report.” Translational cancer research, 2020; 9: 2089-2094.
- Slimane M, Gadria S, Hadidane M, et al. Recurrence of sex cord tumor with annular tubules in young patient with Peutz-Jeghers syndrome. J. Case Rep. Images Oncol, 2016; 2: 74–78.

