A Case of Mycobacterium Abscessus in an Immunocompetent Patient
Peter Leahy*
Department of Medicine, University Hospital Limerick, Ireland
Received Date: 05/01/2022; Published Date: 24/01/2022
*Corresponding author: Peter Leahy, Department of Medici, University Hospital Limerick, Raheen, Limerick, Ireland
Abstract
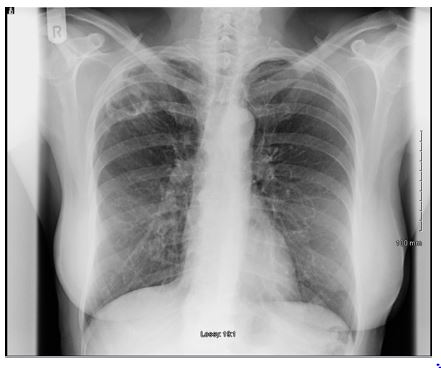
Presentation: A 71-year-old lady from the USA, presented with a four-week history of cough and dyspnoea with a cavitary lesion on her chest x-ray.
Diagnosis: Subsequent CT Thorax and bronchoscopy with bronchoalveolar lavage (BAL) and transbronchial needle aspirate (TBNA) biopsies confirmed a diagnosis of mycobacterium abscesses.
Treatment: Having initially been treated with anti-tuberculous therapy, this was ceased, and she completed a course of oral clarithromycin before being lost to follow-up on her return to the USA.
Discussion: She had no identifiable risk factors or underlying lung disease and work-up for immunosuppression was negative. It is very rare for m. abscesses to cause lung pathology in immunocompetent patients
Case Report
A 71-year-old American tourist from Florida on holiday in Ireland, presented to hospital with a 6-week history of persistent cough productive of green purulent sputum without haemoptysis.
Her background history was unremarkable; she had no underlying lung disease and was a non-smoker. She had never been admitted to hospital acutely before and had no recent courses of antibiotics or steroids. She was never ill as a child and had no significant family history. She is a retired schoolteacher and had no history of tuberculosis (TB) or TB exposure.
A chest radiograph was performed showing a 3 cm thin-walled cavity in the right upper lobe.
Sputum cultures were sent, and she was admitted to the ward in an isolation room and put on an IV penicillin-based antibiotic. She was referred urgently to the respiratory service and underwent a HRCT and bronchoscopy.

The CT showed an abnormal right upper lobe with a 6 cm slightly thick-walled cavity associated with local parabronchial thickening and multiple small soft nodular opacities in the right upper lobe.
A Transbronchial Biopsy (TBNA) and Bronchoalveolar Lavage (BAL) were taken and sent for TB culture and microscopy. She was commenced on quadruple TB therapy at that point and discharged from hospital. She was advised to refrain from flying.
She returned to the outpatient department 2 weeks later. Her FBC was normal, negative HIV screen and her immunoglobulins, complement levels, HbA1c and autoimmune screen all returned as normal.
The results of the sputum and bronchial washings returned a diagnosis of mycobacterium abscesses. It was resistant to ciprofloxacin, cotrimoxazole and doxycycline and sensitive to amikacin, clarithromycin, and linezolid.
Her TB therapy was stopped, and she was commenced on oral clarithromycin. She was lost to follow-up when she flew back home to the USA.
Discussion Mycobacterium Abscesses
Mycobacterium abscesses is a rapidly growing mycobacterium (RGM) distantly related to TB and Leprosy[i]. M. abscesses can cause a variety of clinical manifestations, mostly skin and soft tissue infections. Granuloma formation is the hallmark of its disease process.
Rarely, in individuals with underlying respiratory conditions or impaired immunity, m. Abscesses can cause lung infection. Host risk factors for disease include increased age, smoking/vaping, underlying cystic fibrosis or bronchiectasis, immunosuppression (HIV/AIDS, mutations in interferon gamma pathway or immunosuppressive drug therapy with TNF-alpha inhibitors) and broad-spectrum antibiotic use[ii]. It is even rarer for m. Abscesses to cause lung pathology in immunocompetent patients.
This case of mycobacterium abscesses infection occurred in a previously healthy lady without underlying lung disease or immunosuppressive disease. The secondary work up for underlying immunological deficiency was negative with a negative HIV screen, normal immunoglobulins and complement and she was never on immunosuppressive therapy. She had a negative sweat test and no evidence of underlying lung damage on CT scan or PFTs.
Is there a geographical component to this case? In a 2012 study by Adjemian et al[iii] identified Florida as a particular high-risk area for pulmonary NTM. A 2018 study of hospitalised patients with NTM based in Miami, Florida showed a similar pattern of resistance as in our case.
The literature for m. abscesses infection in immunocompetent hosts and those without underlying cystic fibrosis mainly deals with skin and soft tissue infections. The previously published case reports of immunocompetent patients with pulmonary mycobacterium abscesses infection identified previous pulmonary TB, COPD, pulmonary sequestration, and a new diagnosis of mild phenotypic cystic fibrosis as underlying risks. [iv]
Could this lady have an as-yet undiagnosed subclinical immunosuppressive disease? This is possible as new advances in throughput technology means an increasing recognition of subtle genetic mutations causing immune dysfunction. There is no family history whatsoever however this does not exclude de novo mutations. The mystery continues.
References
- https://www.cdc.gov/hai/organisms/mycobacterium.html.
- https://www.sciencedirect.com/topics/medicine-and-dentistry/mycobacterium-abscessus#:~:text=Predisposing%20conditions%20that%20are%20commonly,usually%20younger%20than%2040%20years.
- Adjemian J, Olivier KN, Seitz AE, Holland SM, Prevots DR. Prevalence of nontuberculous mycobacterial lung disease in U.S. Medicare beneficiaries. Am J Respir Crit Care Med, 2012; 185(8): 881-886. doi: 10.1164/rccm.201111-2016OC, PMID: 22312016; PMCID: PMC3360574.
- Wang PP, Bray CA, Lapierre SG, Soualhine H, Arbour F. Mycobacterium abscessus Lung Infection: A Case Report. Can J Hosp Pharm, 2016; 69(3): 238-243. doi:10.4212/cjhp.v69i3.1562.

