The Analgesic Distribution of Thoracic Paravertebral Interfacial Plane Blocks is Patient Dependent and Clinically Variable
Jiang Wu*, Nina C Patel, Wil Van Cleve, Ryu Komatsu
Department of Anesthesiology, University of Washington, USA
Received Date: 12/12/2022; Published Date: 20/01/2022
*Corresponding author: Jiang Wu, MD, University of Washington, Department of Anesthesiology and Pain Medicine Box 356540, 1959 NE Pacific Street, RR-442A, Seattle Washington 98195, USA
Abstract
In this case report, by performing a fluoroscopically guided thoracic retrolaminar paravertebral block and an erector spinae plane block in the same individual, we demonstrate differences in the radiographic spread of contrast from these two distinct variants of the thoracic paravertebral interfacial plane block. The dermatosensory exam following each block demonstrated that these two block variants were clinically indistinguishable within a particular patient but variable across patients. We review the relevant anatomy for these blocks and discuss possible explanations for our findings in order to offer guidance for the rational clinical application of these blocks in the management of acute and chronic pain.
Keywords: Thoracic paravertebral interfacial plane blocks; Fluoroscopy guidance; Analgesic distribution
Introduction
Thoracic Retro Laminal Paravertebral Block (RLPVB) and Erector Spinae Plane Block (ESPB) are currently considered to be thoracic paravertebral interfacial plane blocks or compartment blocks, and have attracted substantial interest from regional anesthesiologists, purporting to offer the benefits of epidural / classic paravertebral analgesia with lower risk and greater ease of placement then the classical paravertebral or
thoracic epidural blocks [1-3]. The RLPVB and ESPB target the same musculofascial plane between the erector spinae muscles (ESM) and underlying posterior surfaces of the lateral thoracic vertebrae [4,5].
The two variants differ in that the RLPVB targets the dorsal aspect of the lamina (Point A in Figure 1), while the ESPB targets the dorsal aspect of the transverse process (Point B in Figure 1). Authors have noted substantial variability in the distribution of analgesia following RLPVB/ESPB, with two hypothesized pathways of local anesthetic spread being offered for this observation [3]. In this case report, we document the dermatosensory blockade achieved in three patients in which we performed both RLPVB and ESPB under fluoroscopic guidance. By examining the similarities and differences in contrast spread and dermatosensory blockade achieved in each block, we then propose a unified model which we believe explains the variability observed by other researchers who have studied these blocks.
Methods
University of Washington-approved Informed consent to report the outcomes of this standard of pain care was obtained from the patient. Both RLPVB and ESPB were performed under fluoroscopic guidance on two different sessions separated by several weeks. When performing the RLPVB, we targeted the dorsal aspect of the lamina (Point A in Figure 1) and when performing an ESPB, we targeted the dorsal aspect of the transverse process (Point B in Figure 1).
In both the ESPB and RLPVB, after the delivery of 10 ml of Omipaque, 20 ml of 0.25% bupivacaine was incrementally flushed in 5 ml dose via needle to observe the spread of local anesthetic based on the expansion of contrast (Figure 2 and 3).
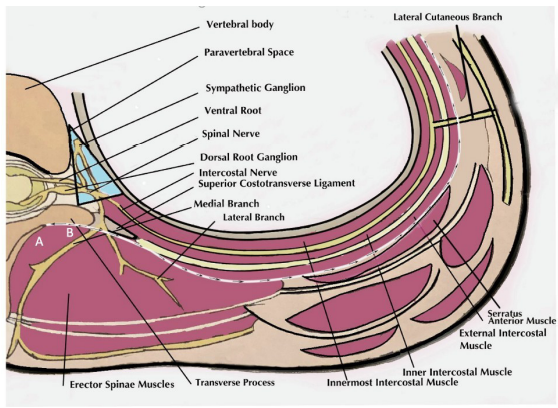
Figure 1: Schematic Illustration of the paraverebra fascial plane anatomy. Point A is needle placement for retrolaminar paravertebral block. Point B is needle placement for erector spinae plane block. The “paravertebral” pathway is highlighted by the blue triangle in the image. The “lateral” pathway is demonstrated by the arrows traveling through fascial plane bordering the external intercostal muscle anteriorly and serratus anterior muscle posteriorly.
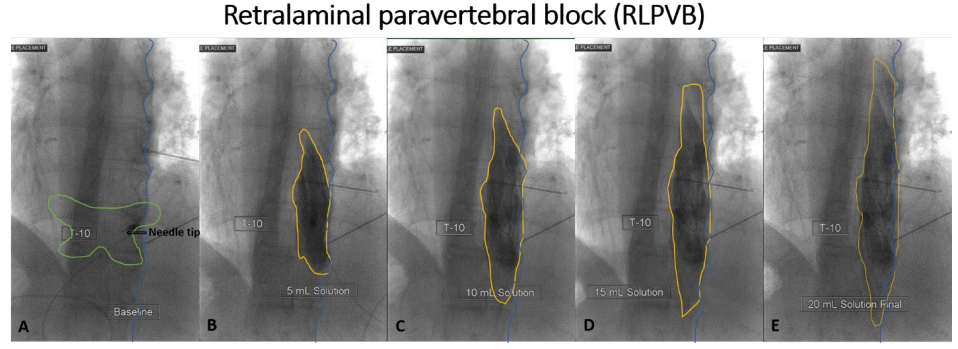
Figure 2: Local Anesthetic spread under fluoroscopy in retrolaminal paravertebral block (RLPVB).
A: The needle tip in RLPVB lands on the dorsal aspect of the lamina of T10; B: contrast spread (in yellow circle) following the delivery of 5 ml of local anesthetic after 10 ml of contrast in RLPVB; C: contrast spread following the delivery of 10 ml of local anesthetic; D: contrast spread following the delivery of 15 ml of local anesthetic; E: contrast spread following the delivery of 20 ml of local anesthetic; the blue line highlighted the right-side contour of facet line.
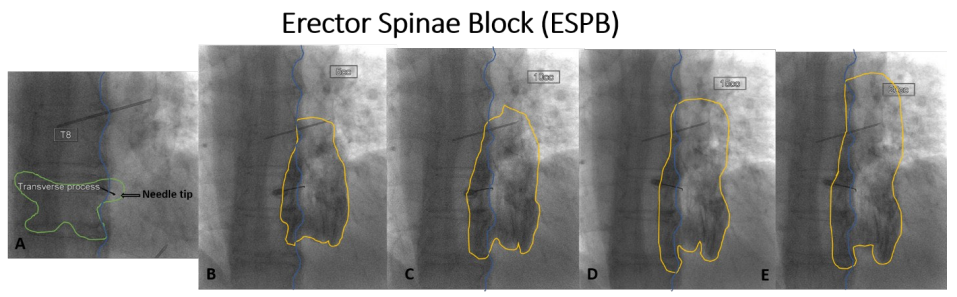
Figure 3: Local Anesthetic spread under fluoroscopy in erector spinae plane block (ESPB).
A: The needle tip in ESPB lands on the dorsal aspect of the transverse process of T9;
B: contrast spread (in yellow circle) following the delivery of 5 ml of local anesthetic after 10 ml of contrast;
C: contrast spread following the delivery of 10 ml of local anesthetic;
D: contrast spread following the delivery of 15 ml of local anesthetic;
E: contrast spread following the delivery of 20 ml of local anesthetic; the blue line highlighted the right-side contour of facet line.

Figure 4: The pre- and post-procedural dermatosensory assessments from ESB and RLPV blocks in 3 cases. Anteriorlateral and posterior-lateral views of analgesic distribution from ESB and RLPVB is depicted in blue. In case 1, postherpetic neuralgia is depicted in red area; In case 2, trigger points are depicted with red X. In Case 2, the thoracotomy incision is marked with a dark line and the post- thoracotomy pain is depicted in red area.
Prior to each procedure, the area of allodynia or trigger points were mapped (Figure 4 in red). 30 min following each block, the resulting analgesic distribution was mapped using pinprick/ice testing (Figure 4 in blue). Additionally, a 6-hour pain diary after the injection was recorded.
The following 3 patients approved reporting their cases.
Case 1:
A 60-year-old female with chronic post-herpetic neuralgia affecting the right-sided posterior lateral thoracic wall along the T10-11 dermatome underwent a right T10 RLPVB (Figure 2) and right T9 ESPB (Figure 3).
Case 2:
A 21-year-old female with extensive bilateral trigger point tenderness in the context of Tourette Syndrome affecting primarily in the area of the right flank and posterior thorax consented for a right T7 ESPB and T7 RLPVB.
Case 3:
A 42-year-old male with persistent left subcostal postsurgical incision pain at T9-T11 dermatome following a prior L2 corpectomy and L1-L3 interbody fusion via a left thoracotomy. The pain was both somatic and neuropathic in nature and radiated to the umbilicus. He received a left T11 ESPB and T11 RLPVB.
Results
In each case, local anesthetic diffused equally in the craniocaudal plane, but more medial to the ipsilateral facet line in the region of the paraspinal muscle in RLPVB (Figure 2B-2E), while spreading more laterally to the ipsilateral facet line over the lung field following the ESPB (Figure 3B-3E).
Local anesthetic injections in cases 1 and 2 were observed extensively spreading 2-3 levels above and below the target vertebrae, while the injection in case 3 demonstrated a more limited cranio-caudal spread (T9-T11). The analgesia distribution achieved in cases 1 and 2 revealed extensive posterior-lateral thoracic wall blockade in the territory of the dorsal ramus and the lateral cutaneous branch of spinal nerves between T3 and T12, but no significant sensory blockade was observed in the territory of the anterior cutaneous branch after either ESPB or RLPVB (Figure 4 Case 1 & 2). In contrast, in case 3, the postprocedural dermatosensory test demonstrated complete T9/T10/T11 dermatomal coverage, with trunk blockade in the territory of both dorsal and ventral ramus (Figure 4 Case 3).
In all cases, within the individual, the resultant dermatosensory blockade from the ESPB was identical to the RLPVB. Based on the pain diary of 6 hours after each injection, all patients reported similarly satisfactory, but partial (> 80%) pain relief from both the ESPB and the RLPVB.
Discussion
Although the ESPB and RLPVB differ slightly in the site of injection, they share the same musculofascial plane within which the injected local anesthetic spreads. Under fluoroscopic observation, these two variants differ primarily in the lateral-medial spread of local anesthetics. The ESPB results in contrast spread
laterally to the ipsilateral facet line over the lung field, whereas the spread following RLPVB in more medial to the ipsilateral facet line in the paraspinal muscle region. However, these two variants share the similarity in the cephalocaudal spread of local anesthetics, although the extensiveness of spread was variable inter-individually, but relatively consistent individually, possibly affected by individual differences in local anatomy.
Regardless of the difference in lateral-medial distribution patterns of injectate between these two variants, we observed that the resultant analgesic distribution was identical within each individual patient. As has been previously documented by other researchers studying dye spread in cadaveric models [6,7], we observed substantial inter-individual variability in the dermatosensory blockade following ESPB/RPLVB. While all 3 cases demonstrated posterior and lateral chest wall analgesia, anterior chest wall analgesia was achieved in Cases 1 and 2 but not in Case 3. Additionally, all three patients report similarly satisfactory, significant, but partial (> 80%) pain relief from either ESPB or RLPVB. Comparing the injection site on the dorsal aspect of transverse process in ESPB the injection site on the dorsal aspect of lamina in RLPVB is a much larger surface to target, which can be translated into a potentially greater safety margin and ease of performance with equivalent clinical effect.
Despite the belief on the part of enthusiasts that RLPVB and ESPB are equivalent alternatives to the classical paravertebral block, our observation of variable anterior analgesic distribution of these blocks is notable and consistent with the variability documented in the extant literature on this topic. Clinically, the ESPB and RLPVB have been reported to be most efficacious in posterior-lateral chest wall pathology and surgical incisions [8-14]. Some studies have claimed the complete effectiveness of these blocks [15-19], whereas other studies have reported failed analgesia for chest well coverage, such as in radical mastectomies [3,14,20]. Anatomically, the absence of anterior dye staining of the ventral ramus following ESPB has been reported in two cadaveric studies [6,21] but one recent cadaveric study demonstrated limited and variable spread to the paravertebral area and spinal nerves after both ESPB and RLPVB [5,21,22].
Based on the post-procedural analgesia mapping in conjunction with the fluoroscopic observation of injectate spread, our data agrees that both ESPB and RLPVB primarily behave as interfacial plane blocks with variable clinical effects, which can be explained by the hypothesis that they exert their clinical effect via two potential pathways [3]. We hypothesize that, in the “lateral” pathway, local anesthetic deposited under the ESM flows laterally along the erector spinae plane bordering the external intercostal muscle anteriorly and serratus anterior muscles posteriorly (Figure 1 travel in arrows) and reliably and predictably blocks the dorsal ramus and lateral cutaneous branch of each spinal nerve.
However, in the “paravertebral” pathway, local anesthetic flows anteriorly, diffusing through the superior costotransverse ligament/foramen into paravertebral space to cover the ventral ramus (Figure1, the blue triangle). We further hypothesize that the “paravertebral” pathway may be dependent on the local anatomic variability surrounding the superior costovertebral ligament/foramen the potentially key anatomic barrier in anterior spread of local anesthetics into paravertebral space. Our findings suggest that the availability of the paravertebral pathway is not predictable at the time the block is placed. After a review of the recent literature, we believe that our study is the first in vivo comparison study on ESPB and RLPVB in the same patient. By conducting pre- and post-procedural dermatosensory assessments in nonsurgical patients, we avoided the complicating factors of surgery or superimposed multimodal analgesia. Similarly, our use of fluoroscopic guidance minimized the impact of technical variation in block placement and ensured appropriate interfacial local anesthetic spread. Our observations support the contention that significant but partial pain relief can be provided by these two block variants for trunk analgesia. In cases wherein anterior chest wall analgesia is essential, we advise caution about the utility of either ESPB or RLPVB. Additionally, given the clinical equivalence of these variants, RLPVB might have better clinical utility given easy technical performance and larger safety margin. Certainly, given the enthusiasm for these new blocks, and the variability in their observed analgesic distribution, we support the need for larger clinical trials to establish their appropriate application in clinical practice.
Declarations
Ethics approval and consent to participate: Patient’s consent was obtained.
Consent for publication: Consent for publication from both authors and patient were obtained.
Availability of data and material: Yes
Competing interests: The authors declare no conflicts of interest.
Funding: This study did not receive any funding in any form
Authors' contributions:
Jiang Wu: This author designed the study, provided clinical care, analyzed, and prepared the radiographs and drawings, conducted literature search, and finalize manuscript.
Nina Patel: This author conducted literature review, drafted manuscript, and prepared the drawings.
Wil Van Cleve: This author drafted manuscript and prepared the drawings. Ryu Komatsu: This author helped write manuscript.
Acknowledgements: None
References
- Tsui BCH, Fonseca A, Munshey F, McFadyen G, Caruso TJ. The erector spinae plane (ESP) block: A pooled review of 242 cases. J Clin Anesth, 2019; 53: 29-34. doi:10.1016/j.jclinane.
- Damjanovska M, Stopar Pintaric T, Cvetko E, Vlassakov K. The ultrasound-guided retrolaminar block: volume-dependent injectate distribution. J Pain Res, 2018; 11: 293-299. doi:10.2147/ JPR.S153660.
- Onishi E, Toda N, Kameyama Y, Yamauchi M. Comparison of Clinical Efficacy and Anatomical Investigation between Retrolaminar Block and Erector Spinae Plane Block. BioMed Res Int, 2019; 2019: e2578396. doi:10.1155/2019/2578396.
- Adhikary SD, Bernard S, Lopez H, Chin KJ. Erector Spinae Plane Block Versus Retrolaminar Block: A Magnetic Resonance Imaging and Anatomical Study. Reg Anesth Pain Med, 2018; 43(7): 756-762. doi:10.1097/AAP.0000000000000798.
- Yang H-M, Choi YJ, Kwon H-J, O J, Cho TH, Kim SH. Comparison of injectate spread and nerve involvement between retrolaminar and erector spinae plane blocks in the thoracic region: a cadaveric study. Anaesthesia, 2018; 73(10): 1244-1250. doi:10.1111/anae.14408.
- Ivanusic J, Konishi Y, Barrington MJ. A Cadaveric Study Investigating the Mechanism of Action of Erector Spinae Blockade. Reg Anesth Pain Med, 2018; 43(6): 567-571. doi:10.1097/ AAP.0000000000000789.
- Dautzenberg KHW, Zegers MJ, Bleeker CP, et al. Unpredictable Injectate Spread of the Erector Spinae Plane Block in Human Cadavers. Anesth Analg, 2019; 129(5): e163-e166. doi:10.1213/ ANE.0000000000004187.
- Nandhakumar A, Nair A, Bharath VK, Kalingarayar S, Ramaswamy BP, Dhatchinamoorthi D. Erector spinae plane block may aid weaning from mechanical ventilation in patients with multiple rib fractures: Case report of two cases. Indian J Anaesth, 2018; 62(2): 139-141. doi:10.4103/ija.IJA_599_17.
- Balaban O, Aydın T. Ultrasound guided bi-level erector spinae plane block for pain management in Herpes Zoster. J Clin Anesth, 2019; 52: 31-32. doi:10.1016/j.jclinane.2018.08.016.
- Kelava M, Anthony D, Elsharkawy H. Continuous Erector Spinae Block for Postoperative Analgesia After Thoracotomy in a Lung Transplant Recipient. J Cardiothorac Vasc Anesth, 2018; 32(5): e9-e11. doi:10.1053/j.jvca.2018.04.041.
- Yoshida H, Yaguchi S, Chiba N, Kitayama M, Hanada H. Ultrasound-guided lumbar retrolaminar block for acute lumbar trauma. Anaesth Intensive Care, 2015; 43(4): 528-529.
- Calandese F, Adduci A. Erector spinae plane block for acute postoperative pain management after anterior thoracolumbar spine surgery. J Clin Anesth, 2019; 52: 55-56. doi:10.1016/j.jclinane.
- Nath S, Bhoi D, Mohan VK, Talawar P. USG-guided continuous erector spinae block as a primary mode of perioperative analgesia in open posterolateral thoracotomy: A report of two cases. Saudi J Anaesth, 2018; 12(3): 471-474. doi:10.4103/sja.SJA_755_17.
- Ueshima H, Hiroshi O. Transapical transcatheter aortic valve implantation performed with a retrolaminar block. J Clin Anesth, 2016; 35: 274. doi:10.1016/j.jclinane.
- Petsas D, Pogiatzi V, Galatidis T, et al. Erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: a case report. J Pain Res, 2018; 11: 1983-1990. doi:10.2147/JPR. S164489.
- Restrepo-Garces CE, Chin KJ, Suarez P, Diaz A. Bilateral Continuous Erector Spinae Plane Block Contributes to Effective Postoperative Analgesia After Major Open Abdominal Surgery: A Case Report. Case Rep, 2017; 9(11): 319-321. doi:10.1213/ XAA.0000000000000605.
- Chin KJ, Adhikary S, Sarwani N, Forero M. The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia, 2017; 72(4): 452-460. doi:10.1111/anae.13814.
- Chin KJ, Malhas L, Perlas A. The Erector Spinae Plane Block Provides Visceral Abdominal Analgesia in Bariatric Surgery: A Report of 3 Cases. Reg Anesth Pain Med, 2017; 42(3): 372-376. doi:10.1097/AAP.0000000000000581.
- Bonvicini D, Tagliapietra L, Giacomazzi A, Pizzirani E. Bilateral ultrasound-guided erector spinae plane blocks in breast cancer and reconstruction surgery. J Clin Anesth, 2018; 44: 3-4. doi:10.1016/j.jclinane.
- Ueshima H, Otake H. Limitations of the Erector Spinae Plane (ESP) block for radical mastectomy. J Clin Anesth, 2018; 51: 97. doi:10.1016/j.jclinane.
- Forero M, Adhikary SD, Lopez H, Tsui C, Chin KJ. The Erector Spinae Plane Block: A Novel Analgesic Technique in Thoracic Neuropathic Pain. Reg Anesth Pain Med, 2016; 41(5): 621-627. doi:10.1097/AAP.0000000000000451.
- Sabouri AS, Crawford L, Bick SK, Nozari A, Anderson TA. Is a Retrolaminar Approach to the Thoracic Paravertebral Space Possible?: A Human Cadaveric Study. Reg Anesth Pain Med, 2018:1. doi:10.1097/AAP.0000000000000828.

