Adult Henoch Schonlein Purpura
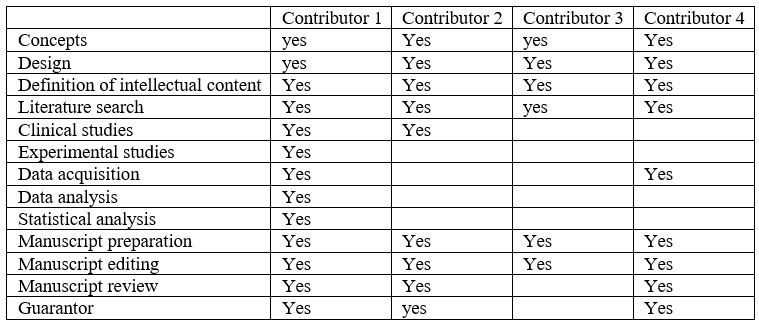
Fotedar Sanjay*, Atri Sudhir k DM, Mukhrjee Angshuman, Karthik A
Department of Internal Medicine Pt BDS PGIMS Rohtak, India
Received Date: 24/12/2021; Published Date: 10/01/2022
*Corresponding author: Sanjay Fotedar, Associate professor, Department of Internal Medicine Pt BDS PGIMS, Rohtak, India
Abstract
Henoch Schonlein Purpura (HSP), a IgA mediated small vessel vasculitis, characterized by the clinical trial of palpable purpura (non-thrombocytopenic), arthritis and abdominal pain and sometimes as tetrad with renal involvement as fourth presenting clinical feature. Pathologically it characterized by immune complex mediated leukocytoclastic vasculitis and clinically by dermatological and other organ/system involvement. Primarily seen in pediatric age group, it has been reported in adults albeit rarely.
Keywords: Adult purpura; Leukocytoclastic vasculitis; IgA nephropathy
Key Message: Henoch Schonlein purpura in adults often presents as a diagnostic challenge especially in the background of acute abdominal presentation. The diagnostic dilemma is compounded by the fact that HSP is classically considered as a vasculitis of children and thus is not considered in the differential diagnosis for adults.
Introduction
Henoch Schonlein Purpura (HSP) is an IgA mediated systemic vasculitis clinically characterised by the triad of abdominal pain, arthritis, non-thrombocytopenic purpuric rash in the lower half of the body, sometimes as a tetrad with renal involvement being additional feature as reported in medical literature1 . Though commonly a disease of children, it may present in adulthood; an incidence of 3.4 to 14.3/million has been reported in adults1,2, with a higher probability of more serious sequelae. Authors report a case of a young male presenting with fever, dermal rash and GI bleed diagnosed as a case of Adult HSP.
Case History
A 28-year-old male, non-smoker, chronic alcoholic, not a known case of any chronic disease presented with complaints of diffuse arthralgia associated with reddish brown rashes on lower extremities (Figure 1 Reddish brown raised purpuric spots on the anterior surface of lower limbs). General physical examination revealed only raised purpuric spots on the lower half of the body predominantly on the anterior aspect of the lower limbs and mild periorbital puffiness. Systemic examination was within normal limits. CBC, LFT and coagulation studies were within normal limits with RFT values being on the borderline (Hb 14, TLC 11200, APC 3 lakh, Blood Urea 80mg/dl, serum creatinine 1.5mg/dl, serum albumin 3.2mg/dl, INR 1.10, A:G ratio = 1). Urine dipstick examination revealed 1+ proteinuria. As per Dermatology opinion, a provisional diagnosis of small vessel vasculitis was made. Skin biopsy and renal biopsy carried out for histological confirmation. The patient was discharged on ramipril and diuretics and put on follow up. However, the patient presented within one week in the emergency again with five episodes of hematemesis and generalised facial puffiness. Patient had history of melena associated with abdominal pain for 3 days. General physical examination was within normal limits except for the persistence of the purpuric rash. Upper GI Endoscopy was performed which revealed no significant lesion, USG abdomen revealed mildly coarse echotexture of liver with no free fluid. However, this time investigations revealed increasing blood urea levels (80 mg/dl to 117 mg/dl) and increasing serum creatinine values (1.5 mg/dl to 1.8 mg/dl). c-ANCA and p-ANCA results (non-specific markers for vasculitis) were negative. The dermal biopsy was suggestive of leucocytoclastic vasculitis (Figure 2 Dermal biopsy showing leucocytoclastic vasculitis) and the renal biopsy for HPE and IFA was suggestive of mesangial proliferation with IgA deposits, suggestive of IgA nephropathy (Figure 3 Renal biopsy showing IgA deposits suggestive of IgA nephropathy). Based on the clinical history as well the supportive diagnostic evidence, a diagnosis of Adult HSP was made. The patient was started on pulse methylprednisolone therapy for 5 days and then switched to oral prednisolone. The facial edema began to resolve and the patient improved symptomatically. The palpable purpuric rashes gradually became macular and started disappearing and patient discharged on tapering steroids.
Discussion
HSP is systemic vasculitis characterized by IgA immune complex deposition in tissues with small vessel involvement. Immune complex deposits containing C3 and IgA is detected in the skin, mucosa of intestines, joints with kidney being the main organ involved although generally self-limiting. Adult disease is more commonly characterized by varied spectrum of renal involvement and may progress to chronic kidney disease and rarely to End Stage Renal [1,2] Disease.
The diagnosis of HSP as per the European League against Rheumatism (EULAR) criteria is based on Purpura (mandatory criterion): commonly palpable and in crops or petechiae, with lower limb predominance, non-thrombocytopenic with at least one of the four criteria [2,3] as (a). Diffuse abdominal colicky pain with acute onset assessed by history and physical examination. May include intussusception and gastrointestinal bleeding, (b). Histopathology revealing typically leucocytoclastic vasculitis with predominant IgA deposit or proliferative glomerulonephritis with predominant IgA deposit (c). Arthritis of acute onset defined as joint swelling or joint pain with limitation on motion and/or Arthralgia of acute onset defined as joint pain without joint swelling or limitation on motion (d). Renal involvement with Proteinuria >0.3 g/24 h or >30 mmol/mg of urine albumin/creatinine ratio on a spot morning sample or haematuria or red blood cell casts: >5 red blood cells/high power field or red blood cells casts in the urinary sediment or ≥2+ on dipstick. Joint involvement is characterized by arthralgias/arthritis which is usually the second common clinical manifestation. Joint involvement is transient, oligoarticular, nondeforming and migratory associated with tenderness and periarticular swelling with effusion [1,4].
Kidney involvement, mainly in adults, usually manifests as mild glomerulonephritis with dysmorphic haematuria on microscopy and non-nephrotic proteinuria5.GI involvement is relatively less common in adults. When present, it may present as acute progressive abdominal pain 7mimicking surgical abdomen requiring laparotomy and/or GI bleeding. Case reports of spontaneous resolution of intussuception with high dose corticosteroid therapy do exist [6-8].
Diagnosis of HSP is clinical with signs and symptoms of organ/system involved. Skin biopsy is useful in confirming leucocytoclastic vasculitis and renal biopsy in some cases to rule out other causes of glomerulonephritis [1,2,9].
Adults in comparison with children often require more aggressive therapy. The choice of drug varies in with respect to the severity of the renal versus extra renal manifestation. While corticosteroid therapy was associated with earlier resolution of renal features, its benefit in maintaining long term remission is questionable. Corticosteroid therapy is however associated with early resolution of extrarenal manifestations. The drugs used for severe renal involvement include cyclosporine, mycophenolate mofetil and rituximab especially in refractory and steroid dependant cases where rituximab therapy was associated nearly full resolution of symptoms [1,4]. Plasmapheresis has been tried for refractory HSP with near full recovery especially in patients with rapidly progressive AKI [10].
Conclusion
HSP in adults thus often presents as a diagnostic challenge especially in the background of acute abdominal presentation as HSP is classically considered as a vasculitis of children. On top of that, the range of renal involvement, the lack of a classical histological picture makes the clinical picture indispensable in the diagnosis and further therapy of such patients.
Conflicting of interest: None
Acknowledgement: None
References
- Gunturu SG, Sohagia AB, Tong TR, Hertan HI. Henoch-schonlein purpura-A case report and review of the literature. Gastroenterol Res Pract, 2010.
- Jithpratuck W, Elshenawy Y, Saleh H, Youngberg G, Chi DS, Krishnaswamy G. The clinical implications of adult-onset henoch-schonelin purpura. Clin Mol Allergy [Internet]. 2011; 9(1): 9.
- Ozen S, Pistorio A, Iusan SM, Bakkaloglu A, Herlin T, Brik R, et al. EULAR/PRINTO/PRES criteria for Henoch-Schönlein purpura, childhood polyarteritis nodosa, childhood Wegener granulomatosis and childhood Takayasu arteritis: Ankara 2008. Part II: Final classification criteria. Ann Rheum Dis, 2010; 69(5): 798–806.
- Hetland LE, Susrud KS, Lindahl KH, Bygum A. Henoch-schönlein purpura: A literature review. Acta Derm Venereol, 2017; 97(10): 1160–1166.
- Pillebout E, Thervet E, Hill G, Alberti C, Vanhille P, Nochy D. Henoch-Schönlein Purpura in adults: Outcome and prognostic factors. J Am Soc Nephrol, 2002; 13(5): 1271–1278.
- Blanco R, Martinez-taboada VM, Rodriguez-valverde V, Garcia-fuentes M, Gonzalez-gay MA. Two Different Expressions of the Same Syndrome. Arthritis Rheum, 1997; 40(5): 859–864.
- McPartland K, Wright G. Acute abdominal pain: Henoch-Schönlein purpura case in a young adult, a rare but important diagnosis. Clin Med J R Coll Physicians London, 2019; 19(1): 77–79.
- Krishnan M, Nahas J. Adult Onset Henoch-Schonlein Purpura and Intussusception: A Rare Presentation. Case Rep Rheumatol, 2016; 2016: 1–3.
- Kamath N, Rao S. Henoch-Schonlein purpura: An update. Indian J Rheumatol [Internet], 2012; 7(1 SUPPL): 92–98.
- Chaudhary K, Shin JY, Saab G, Luger AM. Successful treatment of Henoch-Schonlein purpura nephritis with plasma exchange in an adult male. NDT Plus; 2008; 1(5): 30.

