Bilateral Ovarian Krukenberg Tumor in Pregnancy
Oumaima M’hamdi, Sarah Boujida, Aicha Kharbach
Department of Gynecology and Obstetrics, Maternity Souissi, University Hospital Center Ibn Sina, University Mohammed V, Rabat, Morocco
Received Date: 03/12/2022; Published Date: 05/01/2022
*Corresponding author: Oumaima M’hamdi, Department of Gynecology and Obstetrics, Maternity Souissi, University Hospital Center Ibn Sina, University Mohammed V, Rabat, Morocco
Abstract
The combination of pregnancy and ovaries cancer is rare and even more rare for Krukenberg tumor. Very few cases are reported in the litterature. The Krukenberg tumor is a mucinous ovarian metastasis of a digestive tumor. The prognosis is very poor. Most patients are diagnosed later or even on post-partum, others during an acute hemorrhagic. For these reasons, an early diagnosis is very important and challenging. We report the case of a 35 years old woman admitted at 34 weeks of pregnancy for pre-eclampsia and diagnosed with huge bilateral ovarian Krukenberg tumor. We should think about this diagnosis in patient with epigastralgia, nausea or bilateral ovarian mass. An early diagnosis leads to an early management and an improvement of the prognosis.
Keywords: Krukenberg; Ovarian tumor; Pregnancy
Introduction
During pregnancy, ovarian tumors are ranked second among gynecological tumors, right behind cervical cancer. Most of them are benign (teratoma, cystadenoma…). Only 2 to 5% are malignant [1]. Therefore, the combination of pregnancy and ovaries cancer is rare (only one case for 1000 pregnancies); and even more rare for Krukenberg tumor. Very few cases are reported in the litterature. The Krukenberg tumor is a mucinous ovarian metastasis of a digestive tumor, especially the gastric one (70%) [2]. Those tumors are even less common (1-2% of all ovarian tumors) due to the incidence of gastric cancer for women of reproductive age (0,4%) [1,3]. The prognosis is very poor. Most patients are diagnosed later or even on post-partum, others during an acute hemorrhagic. For these reasons, an early diagnosis is very important and challenging. We report the case of a 35 years old woman admitted at 34 weeks of pregnancy and diagnosed with huge bilateral ovarian krukenberg tumor.
Case Report
A 35 years old woman, gravida 2 para 2, was admitted in our hospital for severe pre-eclampsia. She was at 34 weeks of pregnancy at that moment.
4 weeks before her hospitalization, she had undergone a whole blood test for her pre-eclampsia and an ultrasonography. The ultrasound had shown a lateralized serous fibroid of 9 centimeters.
1 week before, she had developed epigastralgia radiating to the left hypochondria associated with nausea, a progressive increase in abdominal volume and oligoanuria.
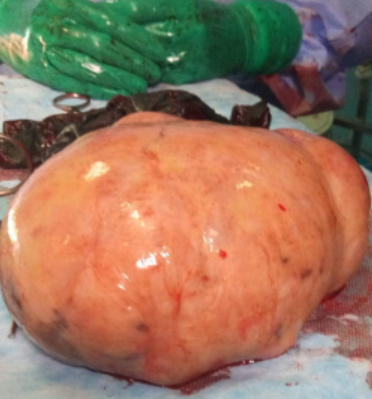
She was admitted in our hospital for severe pre-eclampsia with an arterial tension at 150/100 mmHg, epigastralgia and proteinuria in urine strips. The obstetrical exam showed no abnormalities and the abdominal one found ascites of medium abundance.After receiving first aid, 12 mg of dexamethasone and a full blood test that came back normal, an obstetrical ultrasound was performed and found an eutrophic baby. The tococardiography showed fetal heart rhythm abnormalities. Hence, a cesarean section was done, which allowed the birth of a newborn weighing 2500g, Apgar 10/10. The study found high abundance ascites (3L) with peritoneal carcinosis and two huge bilateral ovarian masses of 20 cm each. The surgical procedure consisted of a bilateral annexectomy with peritoneal biopsy. A hysterectomy was discussed for a long time but was not carried out.
The histological result came back in favor of ovarian metastases of a primitive probably of digestive origin. Fibroscopy confirmed the pyloric origin.
The scanner requested as part of the extension assessment had then objectified a left pleural effusion of low abundance associated with a peritoneal effusion of low abundance with a pre pyloric thickening without deep lymphadenopathy. The patient was given chemotherapy without any surgical supplement. After stabilizing the lesions, the patient died 8 months later.
Discussion
The diagnosis of the Krukenberg tumor during pregnancy is highly unlikely because of its rarity and its similarities with pregnancy signs. On the one hand, the association of ovarian tumor and pregnancy is exceptional. And among these tumors, only 2 to 5% are malignant [3,4]. Out of these 2-5%, only 2.4% is a krukenberg tumor. On the other hand, apart from pregnancy, this type of tumor represents 6% of the total of ovarian tumors and 0.4 to 0.5% for young women of childbearing age. Therefore, this explains the exceptional association of pregnancy with this type of tumor. Sex hormones during pregnancy promote the development and diffusion of gastric cancer by stimulating the underlying precancerous lesions. Placental growth factor levels are high in gastric cancer tissue [3]. Patients are generally asymptomatic. If there are symptoms, these are non-specific [4] such as weight loss, abdominal meteorism, hirsutism and virility… In addition, the signs of pregnancy often overshadow those of the tumor… Indeed, some signs are common to both [2] such as nausea, vomiting, increased abdominal volume, epigastralgia and dyspepsia. This results in delayed diagnosis, which is done at an advanced stage in 97% of cases or in the majority of cases in post-partum or in fatal conditions such as an appendix twist or hemoperitoneum secondary to cataclysmic hemorrhage due to an appendix rupture or as part of an impressive hirsutism. Despite the numerous ultrasounds performed on our patient, the diagnosis of an ovarian mass was not made. This is consistent with the literature and can be explained by the rapid evolution of the tumor over the last quarter. The quick progression may correlate with severe preeclampsia, which is predominantly caused by placental hypoxia ischemia [2]. Sure and exact diagnosis is histological [2-4] after resection of the mass or an endoscopic biopsy. These data pushed some authors to recommend gastroscopy in all the parturints with abdominal pain, weight loss and hematemesis during the 2nd trimester; while the American society of gastrointesinal endoscopy has limited this in parturints with high risk factors. In case of bilateral malignant tumor, the ideal treatment is total hysterectomy with bilateral adnexectomy, omentectomy, aortic cure. However, even in case of bilateral tumor, it is sometimes possible to not perform hysterectomy if the uterus is not reached to preserve pregnancy. This approach is supported by the possibility of platinium-based chemotherapy during pregnancy [1]. In addition, immediate intraperitoneal, per- or post-operative chemotherapy combined with radical therapy has improved prognosis [3]. Survival is low [1]. When the original cancer is the colon, the prognosis is better. When it’s gastric, the prognosis depends on stage and treatment. In case of carcinosis, the survival is about 6 months. In case of lymph node involvement, the stage is advanced and the prognosis is worse. Surgery and chemotherapy improve the survival, especially the intra-peritoneal one [3]. As far as pregnancy is concerned, it doesn’t affect the evolution, but the hormonal environment leads to an increase in gastric tumor and the occurrence of acute symptoms such as torsion or rupture.

Conclusions
In conclusion, Krukenberg tumor is very rare and difficult to diagnosis, especially during pregnancy. When a woman is suffering from epigastric pain or vomitting without any evident cause, or when there is bilateral ovarian mass, we must think about the Krukenberg tumor. An early diagnosis may improve the prognosis.
Authors Contribution:
M’hamdi Oumaima took part in the management of the patient, in the bibliographic research and wrote the article. Boujida Sarah and Kharbach Aicha participated in the therapeutic management of the patient. All authors read and approved the final version of the manuscript.
Competing of interests:
Authors do not declare any conflict of interest.
Grant Information:
The author(s) received no specific funding for this work.
References
- Omar Felipe Dueñas-García, Maricela Diaz-Sotomayor, Charu Chanana. Bilateral Ovarian Krukenberg Tumor in a Full-Term Pregnancy. ISRN Obstet Gynecol. 2011; 2011: 620380. 10.5402/2011/620380.
- Jie Zhang, Xinyu Cheng, Cha Han, Zengyan Li, Min Wang, Yue Zhu. Krukenberg tumor in a pregnant patient with severe preeclampsia. Exp Ther Med, 2014; 7(6): 1476–1480. 10.3892/etm.2014.1616.
- Felipe Mendoza-Rosado, Orlando Nunez-Isaac, Alan Espinosa-Marrón, Katheryn Lopez-Arjona & Fernando Davila-Martinez. Krukenberg tumor as an incidental finding in a full-term pregnancy: a case report. Journal of Medical Case Reports, 2021; 15: 304.
- Myung-Won You, Yoon Young Jung, Jung Hwan Shin, Young Ok Hong. Krukenberg Tumors Diagnosed during Pregnancy Simultaneously with Advanced Gastric Cancer: A Case Report. JKoreanSocRadiol, 2015; 72(6): 435-438.

