Disseminated Sporotrichosis in an Immunocompetent Patient: An Unusual Presentation
Chu Ee SEOW, Wan Syazween Lyana WAK, Adawiyah JAMIL, Norazirah MD NOR, Wan Syahira Ellani WAN AHMAD KAMMAL, Chuan Hun DING
Dermatology Unit, Department of Medicine, Faculty of Medicine, Universiti Kebangsaan Malaysia Medical Centre
Dermatology Unit, Internal Medicine Department, Faculty of Medicine and Health Sciences, Universiti Putra Malaysia
Department of Medical Microbiology & Immunology, Faculty of Medicine, Universiti Kebangsaan Malaysia
Received Date: 07/12/2021; Published Date: 30/12/2021
Abstract
Systemic sporotrichosis with cutaneous and pulmonary involvement in an immunocompetent patient is rare. We herein report a case of a 50-year-old man who presented with fever and multiple painful nodules for 1-month duration. On examination, there were hyperpigmented fluctuant subcutaneous nodules with hemorrhagic crusts on the face, trunk and extremities. Skin biopsy revealed acute suppurative granulomatous inflammation and panniculitis with budding yeasts. Chest x-ray demonstrated multiple centrilobular lung nodules at right upper lung zone and CT scan of the thorax showed consolidation over the peribronchovascular of right upper lobe, irregularity of the apical branch of right upper lobe bronchus and right hilar lymphadenopathy. Fungal culture from the skin nodule and bronchoalveolar lavage yielded Sporothrix schenckii. All investigations for immunocompromised state was negative. He was commenced on oral itraconazole which resulted in improvement of his symptoms. This case report highlights the rarity of sporotrichosis affecting the skin and lung simultaneously in an individual with a competent immune response.
Keywords: Disseminated Sporotrichosis; Sporothrix Schenckii; Immunocompetent
Introduction
Systemic sporotrichosis with cutaneous and pulmonary involvement in immunocompetent individual is uncommon. Previous literatures reported that sporotrichosis usually seen as isolated cutaneous form or at a non-pulmonary site such as osteoarticular, neurological or ocular [1-4]. Systemic presentation typically occurs in individuals with impaired immunity such as in diabetes mellitus, immunosuppressant use, HIV infection, malignancy and connective tissue disease [5]. Sporotrichosis is caused by the fungal Sporothrix, in which the pathogenic taxons in human are S.brasiliensis, S.schenckii, S. globose and S. luriei [6]. It is usually found in contaminated plants or in the mouth, nasal cavity, nails and feces of infected cats [4]. Systemic sporotrichosis is believed to be transmitted either via inhalation of Sporothrix propagules or via hematogenous spread [6]. Cutaneous lesion presents as ulcerated papules or nodules while pulmonary sporotrichosis presents with cough, hemoptysis, anorexia and fever. Clinically, cutaneous sporotrichosis can mimic other diseases such as tuberculosis and non-tuberculous mycobacterium, nocardiasis, chromomycosis, leishmaniasis, pyoderma gangrenosum and cutaneous tumors.6 Skin biopsy is warranted in order to rule out these differentials. Typical histopathological findings are diffuse chronic granulomatous dermatitis with a central abscess [6]. Pulmonary involvement can display two different patterns on radiology which are diffuse or bibasal reticulonodular infiltrate pattern, or cavities in the upper lobe [5-7]. Recommended treatment is amphotericin B, given until a favorable response has been achieved. Thereafter, therapy is changed to oral itraconazole 200mg BD for at least 1 year [8].
Case Report
A 50-year-old man with underlying non-alcoholic steatohepatitis and ischemic heart disease presented with fever and multiple painful nodules on trunk and upper limbs for 1-month duration. He denied loss of appetite, loss of weight, prolonged cough or history of contact with ill animals or tuberculosis patients. Occasionally, he did some gardening and cleaned feces from stray cats in housing compound. On examination, there were hyperpigmented fluctuant subcutaneous nodules with hemorrhagic crusts on the face, trunk, upper and lower extremities (Figure 1). Otherwise, examination of other organ systems and lymph nodes were unremarkable.

Figure 1: (a) Multiple erythematous tender ulcerated papules on the cheek, (b) ulcerated nodules on left upper limb (c) abdomen and (d) right lower limb
Blood investigations revealed raised erythrocyte sedimentation rate at 111mm/hour and C reactive protein at 5.79mg/ml. Full blood count, renal profile, liver function test and hemoglobin A1c were within normal range. Autoimmune disease and Human Immunodeficiency Virus (HIV) screening were also negative. He was initially treated with intravenous piperacillin-tazobactam for multiple skin abscesses. However, he remained febrile with formation of more skin nodules. Thus, a skin biopsy was performed to rule out differential diagnoses of infectious panniculitis such as subcutaneous fungal infection, tuberculous and non-tuberculous mycobacterium infection. Histopathology revealed acute suppurative granulomatous inflammation with panniculitis. Periodic acid-Schiff (PAS) and Grocott’s Methenamine Silver (GMS) stains exhibited budding yeasts of approximately 8μm in size, suggestive of sporotrichosis (Figure 2). Fungal culture of the skin identified Sporothrix schenckii (Figure 3). Culture of bacteria and mycobacterium, as well as polymerase chain reaction (PCR) of mycobacterium were negative.
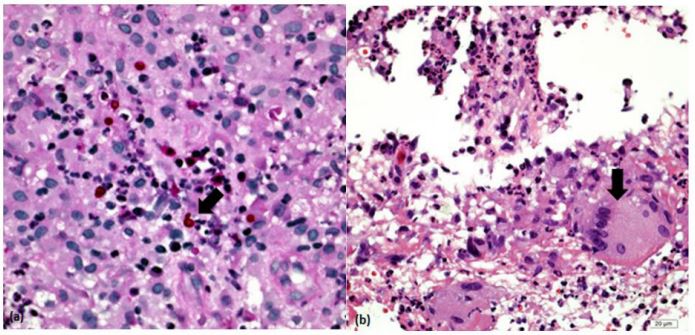
Figure 2: Skin biopsy HPE (a) PAS stain shows presence of budding (arrow) (b) Perivascular infiltration of inflammatory cells and multinucleated giant cell (arrow)
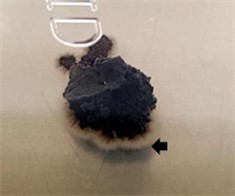
Figure 3: Macromorphology of Sporothrix schenckii, creamy colonies (arrow) forming brown-black color colonies.
Chest x-ray demonstrated multiple centrilobular lung nodules at right upper lung zone (Figure 4). CT scan of thoracic, abdomen and pelvis showed consolidations over peribronchovascular right upper lobe, irregularity of the apical branch of right upper lobe bronchus and right hilar lymphadenopathy (Figure 5) Otherwise, there was no intraabdominal collection. Bronchoscopy revealed swollen, irregular and inflamed mucosa over segmental bronchus of right upper lobe. Fungal culture from bronchoalveolar lavage also grew Sporothrix schenckii. Hence, diagnosis of systemic sporotrichosis with cutaneous and pulmonary involvement was made.
He was started on intravenous amphotericin B deoxycholate 0.7mg/kg/day. Unfortunately, he developed acute renal failure and transaminitis, which resolved upon cessation of amphotericin B. Thereafter, he was prescribed with oral itraconazole 200 mg twice daily. He responded well to the treatment with regression of cutaneous nodules after a month of treatment and was planned for one year course of oral itrconazole. Unfortunately, he was lost to follow-up
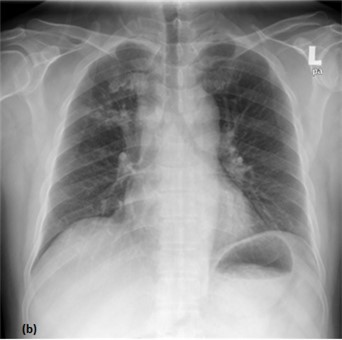
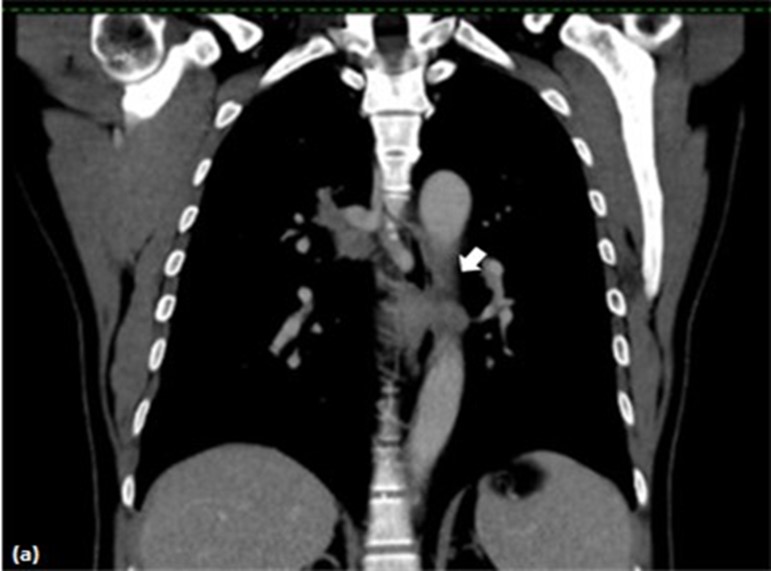
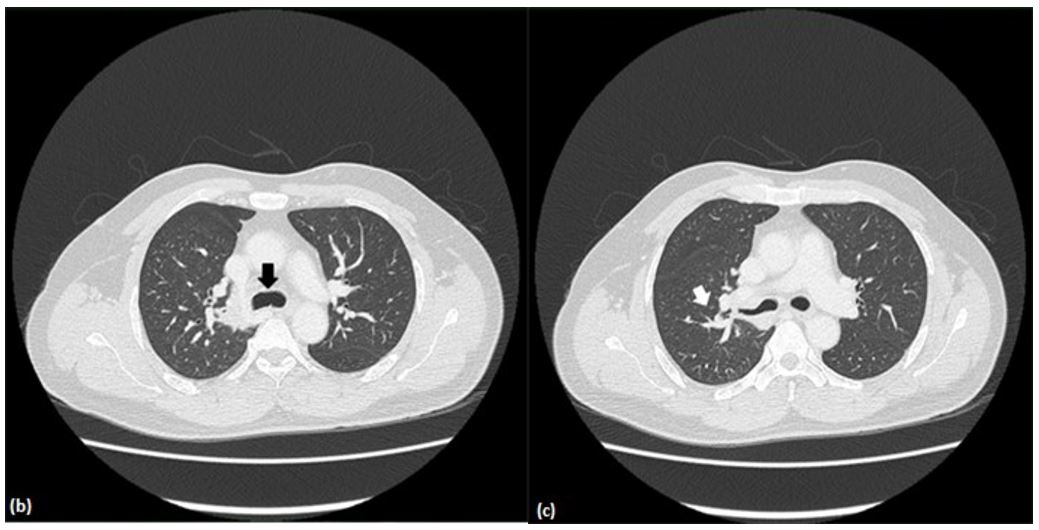
Figure 5: CT images (a) Consolidations over peribronchovascular right upper lobe (b) Irregularity of the apical branch of right upper lobe bronchus (c) Right hilar lymphadenopathy
Discussion
Sporotrichosis can be classified clinically into five forms, namely skin, mucous membrane, systemic, immunoreactive and spontaneous regression. Systemic sporotrichosis is further classified into pulmonary, cutaneous disseminated, osteoarticular, and neurological [6]. Systemic sporotrichosis in an immunocompetent individual is rare. It has been reported in literatures, however these cases involved cutaneous disseminated alone, or involved non-pulmonary sites such as osteoarticular, neurological and ocular [1-4]. To our knowledge, this is the first case reported of systemic sporotrichosis with cutaneous and pulmonary involvement in immunocompetent individual. Such systemic presentation more commonly occurs in the setting of immunosuppressive state such as uncontrolled diabetes mellitus, immunosuppressant use, HIV infection, malignancy and connective tissue disease [5].
Sporotrichosis is caused by thermodimorphic fungi of the genus Sporothrix. Sporothrix comprises of 51 taxons, in which only four taxons are known to be pathogenic in human, namely S. Brasiliensis, S. Schenckii, S. globose and S. luriei [6]. S. Schenckii, which is the organism identified in our patient, is the most common causative agent for sporotrichosis in Malaysia [4]. It is usually found in contaminated plants or in the mouth, nasal cavity, nails and feces of infected cats [4]. Cutaneous sporotrichosis is usually caused by direct inoculation of organism into the skin by trauma. Unfortunately, only 10-62% of patients were able to recall this information [7]. Systemic sporotrichosis is believed to be transmitted either via inhalation of Sporothrix propagules or via hematogenous spread and the latter mode of spread typically occurs in immunosuppressed patients [6]. We postulated that our patient may have contracted the infection through a missed trauma during gardening or via inhalation of the fungal propagules during contact with cats’ feces.
Cutaneous lesions typically present as papules or nodules which may ulcerate or fistulize draining a purulent discharge. 80% of cutaneous cases present as lymphocutaneous form, in which the lesions were distributed along the lymphatic drainage [6]. However, in disseminated cutaneous sporotrichosis, the lesions may be generalized with no specific distribution as seen in our patient. Pulmonary sporotrichosis typically presents with cough, hemoptysis, anorexia and fever [5-7]. Nevertheless, 14.1% may not have any respiratory symptoms (Aung K et al) as demonstrated in our case [5].
Cutaneous manifestation of sporotrichosis can mimic other infectious diseases namely tuberculosis and non-tuberculous mycobacterium, nocardiasis, chromomycosis and leishmaniasis. It may also imitate non-infectious diseases such as pyoderma gangrenosum, primary cutaneous tumors and even cutaneous metastases [6]. Skin biopsy is warranted to rule out these differential diagnoses. Typical histopathological findings are diffuse chronic granulomatous inflammation with a central abscess. The fungal structures, which are highlighted by PAS and GMS, is seen in 18 to 35.3% of cases [6]. Pulmonary involvement can display two different patterns on radiology, depending on the transmission route. Hematogenous route leads to predominantly diffuse or bibasal reticulonodular infiltrate pattern. On the contrary, inhalation route frequently results in upper lobe involvement. Chronic inflammatory response is then ensued, leading to breakdown of necrotic lung tissue and upper lobe cavity formation. These group of patients may be asymptomatic initially until large cavities are formed [5]. These findings further supported the hypothesis that our patient might have contracted the fungal agent through inhalation based on the upper lobe radiological findings and relatively free of pulmonary symptoms. Culture and isolation of S. schenckii from biopsy samples remains the gold standard to diagnose sporotrichosis [5-7]. Depending on the species of Sporothrix, it usually takes 4 to 6 days to isolate Sporothrix spp. for samples collected from skin lesions, and 10-19 days from extracutaneous lesions [6].
Treatment of sporotrichosis depends on the clinical presentation. In lymphocutaneous or osteoarticular manifestation, oral itraconazole 200mg per day is the preferred treatment [6,8]. However, for systemic sporotrichosis, recommended treatment is amphotericin B, given as a lipid formulation at 3-5 mg/kg daily or amphotericin B deoxycholate, administered at 0.7-1.0 mg/kg daily. Treatment is continued until a favorable response has been achieved, after which the therapy is changed to oral itraconazole 200mg BD for at least 1 year [8]. Other than the commonly reported side effects such as nephrotoxicity, amphotericin B can also cause hepatotoxicity. The incidence of increased transaminases and bilirubin due to amphotericin B had been reported at approximately 20% [9]. We hypothesize that our patient’s underlying hepatic disease might have predisposed him to develop raised transaminases upon exposure to amphotericin B.
The response of patients to treatment varies. Uncomplicated skin or mucosal manifestation in immunocompetent patients, usually heal with fibrous scar. However, untreated sporotrichosis can disseminate to other organ systems and may be fatal [6].
Conclusions
This case report highlights the rare presentation of systemic sporotrichosis with disseminated cutaneous and pulmonary involvement. It emphasizes the importance to have a high index of suspicion of the possibility of subcutaneous fungal infection in a patient who presents with suppurative skin nodules unresponsive to antibiotic therapy despite of their immune status. Failure to diagnose or delay in diagnosis may cause a prolonged morbidity or even mortality in patients.
References
- Yap FB. Disseminated cutaneous sporotrichosis in an immunocompetent individual. Int J Infect Dis, 2011; 15(10): e727-9.
- Medeiros KB, Landeiro LG, Diniz LM, Falqueto A. Disseminated cutaneous sporotrichosis associated with ocular lesion in an immunocompetent patient. A Bras Dermatol, 2016; 91(4): 537-539.
- Hassan K, Turker T, Zangeneh T. Disseminated sporotrichosis in an immunocompetent patient. Case Reports Plast Surg Hand Surg, 2016; 3(1): 44-47.
- Tang MM, Tang JJ, Gill P, Chang CC, Baba R. Cutaneous sporotrichosis: a six-year review of 19 cases in a tertiary referral center in Malaysia. Int J Dermatol, 2012; 51(6): 702-708.
- Aung AK, Teh BM, McGrath C, Thompson PJ. Pulmonary sporotrichosis: case series and systematic analysis of literature on clinico-radiological patterns and management outcomes. Med Mycol. 2013;51(5):534-44.
- Orofino-Costa R, Macedo PM, Rodrigues AM, Bernardes-Engemann AR. Sporotrichosis: an update on epidemiology, etiopathogenesis, laboratory and clinical therapeutics. A Bras Dermatol, 2017; 92(5): 606-620.
- Morris-Jones R. Sporotrichosis. Clin Exp Dermatol, 2002; 27(6): 427-431.
- Mahajan VK. Sporotrichosis: An Overview and Therapeutic Options. Dermatology Research and Practice. 2014.
- Inselmann G, Inselmann U, Heidemann HT. Amphotericin B and liver function. Eur J Intern Med, 2002; 13(5): 288-292.

