FAHR’S Syndrome: A Case Report from A Tertiary Care Hospital in Assam
Arindam Ganguly*, Mousumi Das
Department of Pediatrics, Fakhruddin Ali Ahmed Medical College & Hospital, Barpeta, Assam, India.
Received Date: 13/12/2021; Published Date: 29/12/2021
*Corresponding author: Dr. Arindam Ganguly, Department of Pediatrics, Fakhruddin Ali Ahmed Medical College & Hospital, India.
Abstract
Fahr’s Syndrome is a rare neurological disorder with varied clinical manifestations. It is characterized by abnormal calcified deposits in basal ganglia and cerebral cortex. Etiology of this syndrome does not identify a specific agent but associations with a number of conditions have been noted; most common of which are endocrine disorders, mitochondrial myopathies, dermatological abnormalities and infectious diseases. Fahr’s disease commonly affects young to middle aged adults. Here we present a case of Fahr’s syndrome in a 12-year-old female.
Keywords: Fahr’s syndrome, rare disease, abnormal calcification, basal ganglia
Introduction
Basal ganglia calcification is also known as Fahr’s disease or Fahr’s syndrome. German neurologist Karl Theodor Fahr was the first person to describe it in 1930 [1]. This disease is essentially characterized by abnormal deposition of calcium in areas of the brain that control movements including basal ganglia, thalamus, dentate nucleus, cerebral cortex, cerebellum, subcortical white matter, and hippocampus [2]. Extra pyramidal symptoms predominate in most cases, however, neuropsychiatric symptoms, dementia, speech difficulty and cerebellar dysfunction may be present [3]. It is a rare inherited or sporadic neurological disorder with a prevalence of <1/1,000,000 [4].
Case Report
A 12-year-old female reported to our department with complaints of multiple episodes of convulsions and intellectual disability. She has had seizures for last 3 years prior to seeking treatment. She had multiple hypo-pigmented macules over trunk and upper limbs. The lesions were gradually becoming scaly and itchy and scalp was involved. She had squint of the left eye, which according to the attendant, was gradually developing over the last 2 years. The child was having difficulty in continuing with her scholastic performance over the last 2 years. She has developed quasi purposeful movements while walking over the last 1 year. There is no history of fever or head trauma prior to the onset of symptoms. There is no family history of similar illness.
Examination findings and investigations
Child was alert, active, playful. She had choreo-athetoid movements. Her memory was intact, attention span was short. She had mild slurring of speech. Cranial nerves functioning, sensory and motor systems functioning were normal. She had normal dentition.
The child was examined for intellectual disability. Psychiatric assessment was done. Child had an IQ of 68 (Vineland Social Maturity Scale) indicating mild mental retardation in social adaptive functioning.
Dermatology opinion revealed the lesions to be of non-infectious in origin and ceramide lotion was advised.
An EEG was done which should bilateral centroparietal seizure foci. She was started on oral sodium valproate after which her seizures subsided.
A complete blood count, liver function test, renal function test, serum levels of glucose, calcium, magnesium revealed normal results.CSF analysis, thyroid profile study, blood and urine culture & sensitivity tests were negative. Fundoscopy and BERA revealed normal results.
CT Scan of Brain revealed extensive calcification in both basal ganglia regions, both cerebellum and in fronto-parietal regions. MRI brain was planned for further evaluation.
MRI Brain revealed bilateral symmetrical calcifications in basal ganglia, thalami, corona radiate, sub cortical white matter in bilateral fronto-parietal lobe, dentate nucleus and deep cerebellar nuclei.
Based on the examination findings, EEG and brain imaging the diagnosis of Fahr’s Syndrome was considered.

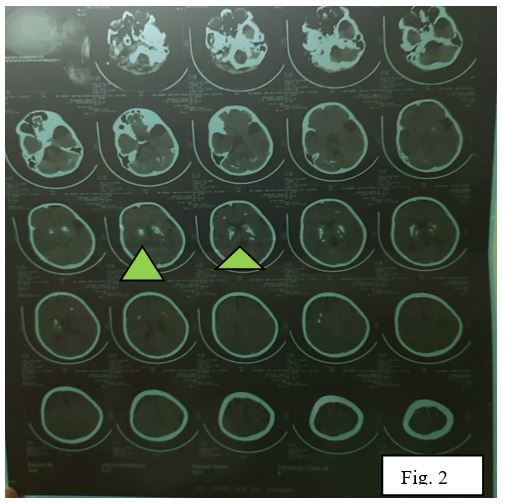
Figure 2: CT Brain revealed calcification in the basal ganglia, fronto-parietal and cerebellar regions (arrowhed).
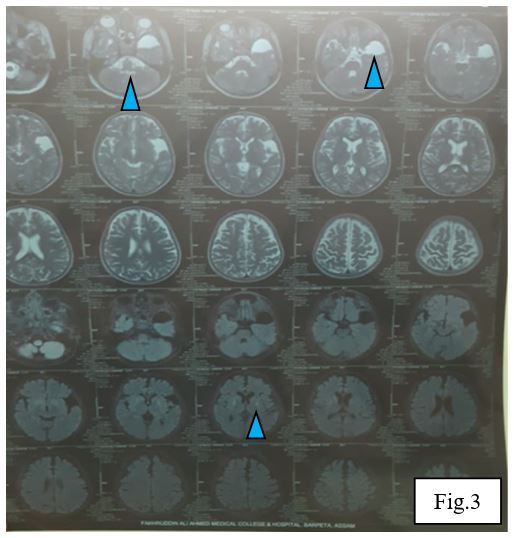
Figure 3: MRI Brain showing calcification in the basal ganglia, fronto parietal lobes, thalami and cerebellum (arrowhead).
Discussion
Fahr’s disease, Fahr’s syndrome or striopallidodentate calcinosis are all pathological terms for the idiopathic nonarteriosclerotic cerebral calcification of the striopallidodentate system. The syndrome, which is either familial or sporadic, shows a wide range of clinical signs with progressive mental deterioration of pyramidal, extra-pyramidal and cerebellar signs [5,6].
A locus at 14q48 (IBGC1) has been suggested to be involved commonly. A second locus has been identified on chromosome 8 and a third on chromosome 2q37 [7,8]. A loss of function mutation in the gene encoding type III sodium dependent phosphate transporter 2 (SLC20A2) located on chromosome 8 has also been reported as the molecular level to form the genetic basis for the pathophysiology of this disease [9].
At the molecular level, calcification generally develops within the vessel wall and in the perivascular space, ultimately extending to the neuron. Due to defective iron transport and free radical production, tissue damage occurs which leads to the initiation of calcification. Progressive basal ganglia mineralization tends to compress the vessel lumen, thus initiating a cycle of impaired blood flow, neural tissue injury and mineral deposition. Basal ganglia concretions are recognized as basophilic globules tracking the vessels of arteries, veins and capillaries. Microscopy reveals perivascular granules lying in the region above midbrain [10,11].
Diagnostic criteria of Fahr’s syndrome have been derived from Moskowitz et al. 1971, Ellie et al. 1989, Manyam 2005 [12-14] and it can be stated as follows:
- Bilateral calcification of the basal ganglia visualized on neuroimaging. Other brain regions may also be observed.
- Progressive neurologic dysfunction, which generally includes a movement disorder and/or neuropsychiatric manifestations.
- Age of onset is typically in the fourth or fifth decade, although this dysfunction may also present in childhood.
- Absence of biochemical abnormalities and somatic features suggestive of a mitochondrial or metabolic disease or other systemic disorder.
- Absence of an infectious, toxic, or traumatic cause.
- Family history consistent with autosomal dominant inheritance.
Management strategies and treatment mainly focus on symptomatic relief and are strictly related to the clinical features. Since selective removal of deposited calcium from the brain without effecting calcium from bone and other tissues appears to be an impossible task13, pharmacological treatment should be used to improve neurological and/or psychiatric symptoms and to try to remove underlying cause15. Appropriate antiepileptic drugs for seizures should be used. Patients who develop psychiatric features should be treated with mood stabilizer or antipsychotic drugs. Neuroleptic medication should be used cautiously, since they may exacerbate extrapyramidal symptoms.
References
- Fahr T. Idiopathische verkalkung der hirngefässe. Zentrabl Allg Pathol, 1930; 50: 129-133.
- Ahad MA, Bala C, Karim S. Fahr’s syndrome. Bangladesh Medical Journal Khulna 2013; 45(1–2): 33–35.
- Chiu H, Lam L, Shum P, Li K. Idiopathic calcification of the basal ganglia. Postgraduate medical journal 1993; 69(807): 68–70.
- Manyam BV, Walters AS, Narla KR. Bilateral striopallidodentate calcinosis: clinical characteristics of patients seen in a registry. Movement disorders: official journal of the Movement Disorder Society 2001; 16(2): 258–264.
- Chalkias SM, Magnaldi S, Cova MA, Longo R, Pozzi-Muccui RS. Fahr disease: significance and predictive value of CT and MRI findings. Eur Radiol, 1992; 2: 570–575.
- Khammabi M, Christi J, Mohsen D, Abdelhedi H, Tougorti MN, Hamza M. Fahr’s syndrome: two case reports. Rev Neurol, 2010; 166: 446–450.
- Geschwind DH, Loginov M, Stern JM. Identification of a locus on chromosome 14q for idiopathic basal ganglia calcification (Fahr disease). Am J Hum Genet 1999; 65(3): 764–772.
- Dai X, Gao Y, Xu Z, Cui X, Liu J, Li Y, et al. Identification of a novel genetic locus on chromosome 8p21. 1–q11. 23 for idiopathic basal ganglia calcification. Am J Med Genet B Neuropsychiatr Genet 2010; 153(7): 1305–1310.
- Wang C, Li Y, Shi L, Ren J, Patti M, Wang T, et al. Mutations in SLC20A2 link familial idiopathic basal ganglia calcification with phosphate homeostasis. Nature genetics 2012; 44(3): 254–256.
- Kazis A: Contribution of CT scan to the diagnosis of Fahr’s syndrome. Acta Neurol Scand, 1985; 71(3): 206–211.
- Adachi M, Wellmann KF, Volk BW. Histochemical studies on the pathogenesis of idiopathic non-arteriosclerotic cerebral calcification. Journal of Neuropathology & Experimental Neurology, 1968; 27(3): 483–499.
- Moskowitz MA, Winickoff RN, Heinz ER: Familial calcification of the basal ganglions: a metabolic and genetic study. N Engl J Med 1971; 285(2): 72–77.
- Manyam BV. What is and what is not ‘Fahr’s disease’. Parkinsonism Relat Disord, 2005; 11(2): 73–80.
- Ellie E, Julien J, Ferrer X. Familial idiopathic striopallidodentate calcifications. Neurology 1989; 39(3): 381–385.
- Sobrido MJ, Coppola G, Oliveira J, Hopfer S, Geschwind DH. (1993–2014) Primary familial brain calcification. In: Pagon RA, Adam MP, Ardinger HH, Bird TD, Dolan CR, Fong CT et al (eds) GeneReviews™. University of Washington.

