Myocardial Bridge and Coronary Syndrome: Clinical Case Report and Literature Review
Alkory Ould SIDI M’hamed, Larsen Clarck MOUMPALA ZINGOULA*, Houda Bellhoussine, Ahmed Djibril Ahmed, Nadia FELLAT, Rokya FELLAT
Cardiology Department, National League for the Fight against Cardiovascular Diseases.
Ibn Sina University Hospital Center, RABAT.
For our University: Mohammed V University of Rabat, Faculty of Medicine and Pharmacy
Received Date: 02/12/2021; Published Date: 28/12/2021
*Corresponding author: Larsen Clarck MOUMPALA ZINGOULA, Cardiology Department, National League for the Fight against Cardiovascular Diseases, Ibn Sina University Hospital Center, RABAT, Morocco.
Summary
The myocardial bridge is a fairly recently reported entity increasingly in young patients, and whose clinic is that of coronary syndrome. Defined as being an intramural segment of a coronary artery `` tunneled segment '' in the myocardium, the Myocardial Bridge achieves a Milking effect following systole compression of the artery, the most frequently involved in this anomaly is the interventricular earlier. The resulting complications are either mild or even significant. The diagnosis is most often post mortem at autopsy, although coronary angiography reports a few cases like our clinical case. This is a patient in whom the diagnosis was made during coronary angiography, and whose management was pharmacological with good progress.
Keywords: Myocardial ischemia; Myocardial bridge ; Milking effect ; Coronary angiography
Introduction
The Myocardial Bridge (MB) is defined, anatomically, as being a segment of coronary artery covered, in its epicardial path, by a band of myocardium, thus forming a `` bridge '' (bridge) over this vascular portion . It is a very common congenital coronary anomaly, the incidence of which is between 5 to 85% at autopsy and 0.5 to 2.5% on coronary angiography 1. Most often asymptomatic, otherwise manifest clinically following a Milking effect in systole heart disease, PM can cause ischemia and even myocardial infarction, left ventricular dysfunction, rhythmic complications and sudden death. Hence the interest we are paying to this subject by reporting the clinical case of our patient with acute coronary syndrome in an inter-hospital setting
Clinical Case
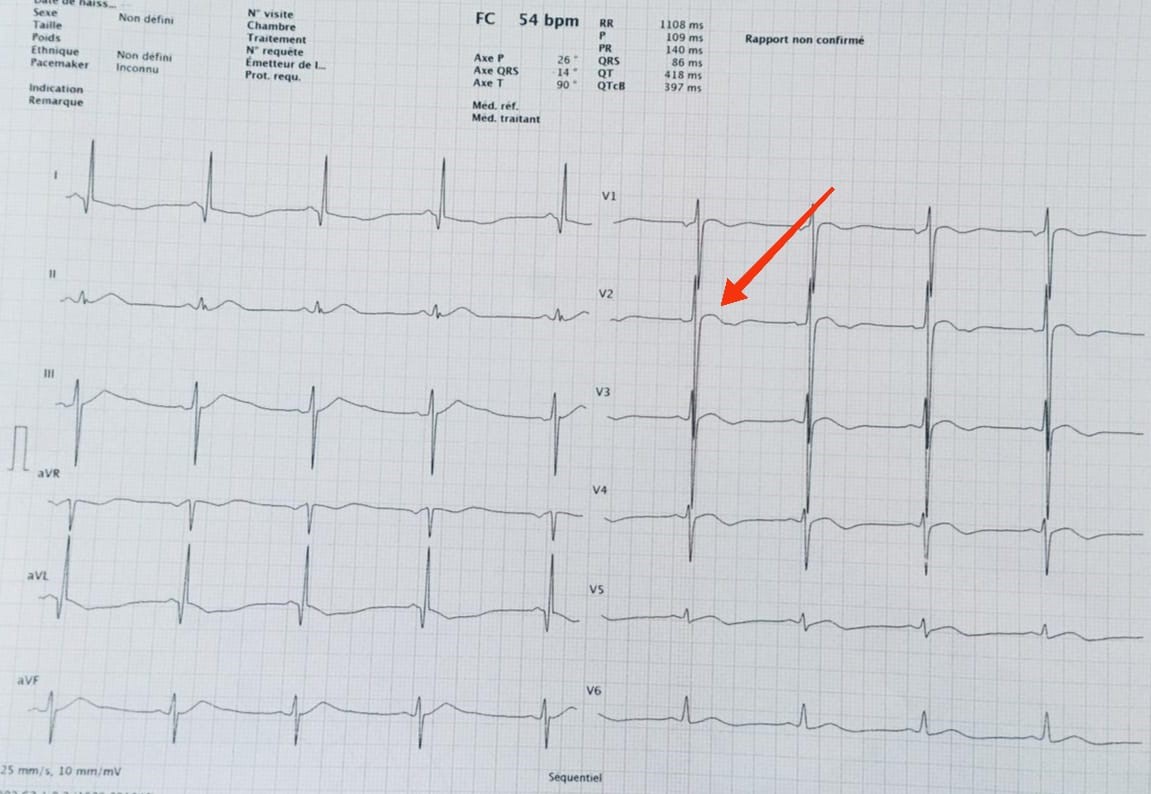
This is a 66-year-old patient with atypical chest pain associated with NYHA stage II dyspnea, followed for hypertension and dyslipidemia on treatment. Clinical examination revealed BP at 120/60 mmHg, HR at 72 bpm, on the twelve-lead ECG (1) noted a biphasic T wave at the antero-septo-apical level (V1-V4) with a fragmented QRS in leads, his admission laboratory results were unremarkable, and the echocardiography was normal. A stress echocardiogram revealed ischemia in the territory of the anterior interventricular artery.
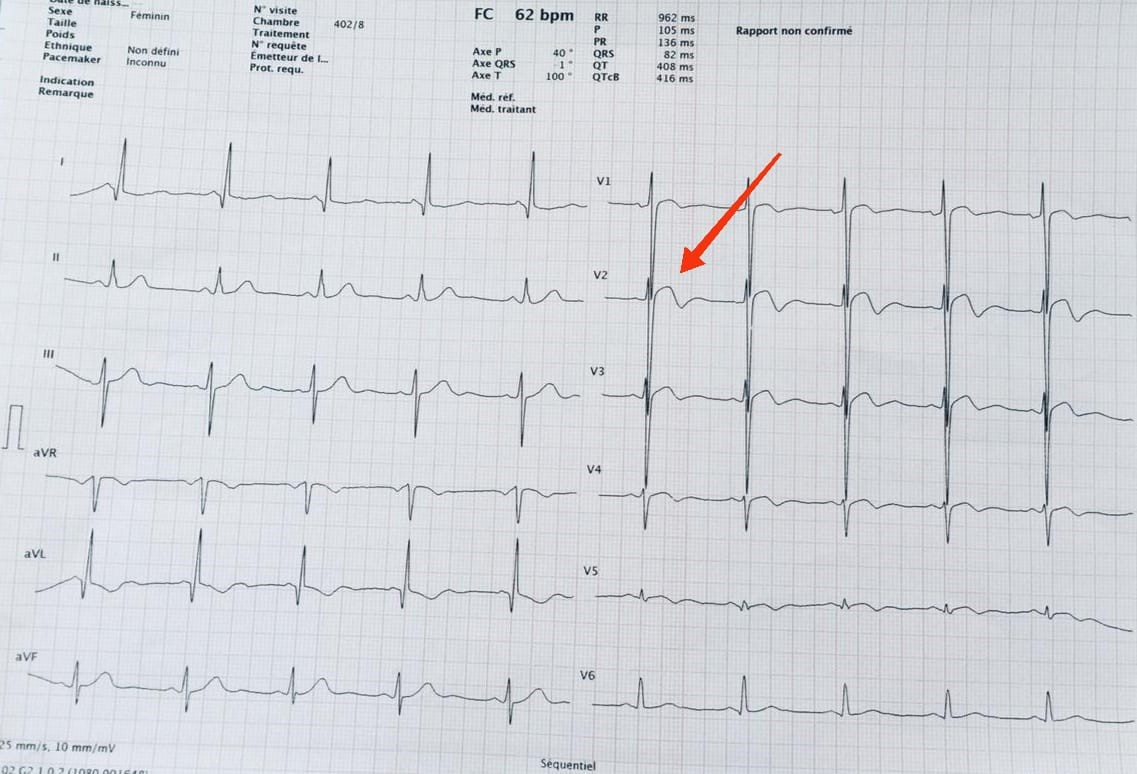
During her hospitalization, the patient presented with acute ischemic-like chest pain associated with nausea, lasting more than 20 minutes, the percritical electrocardiogram showed a transient elevation of the ST segment in the anteropeptal area with an inversion of the T wave in the anterior and lateral leads with a significant rise in troponins to 500 times normal.
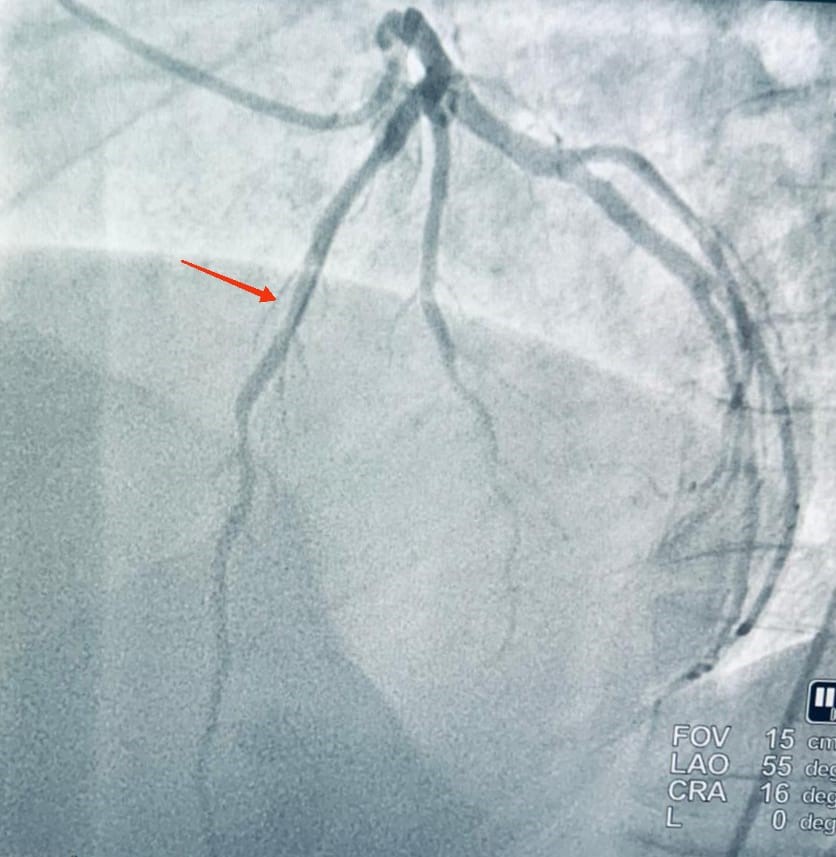
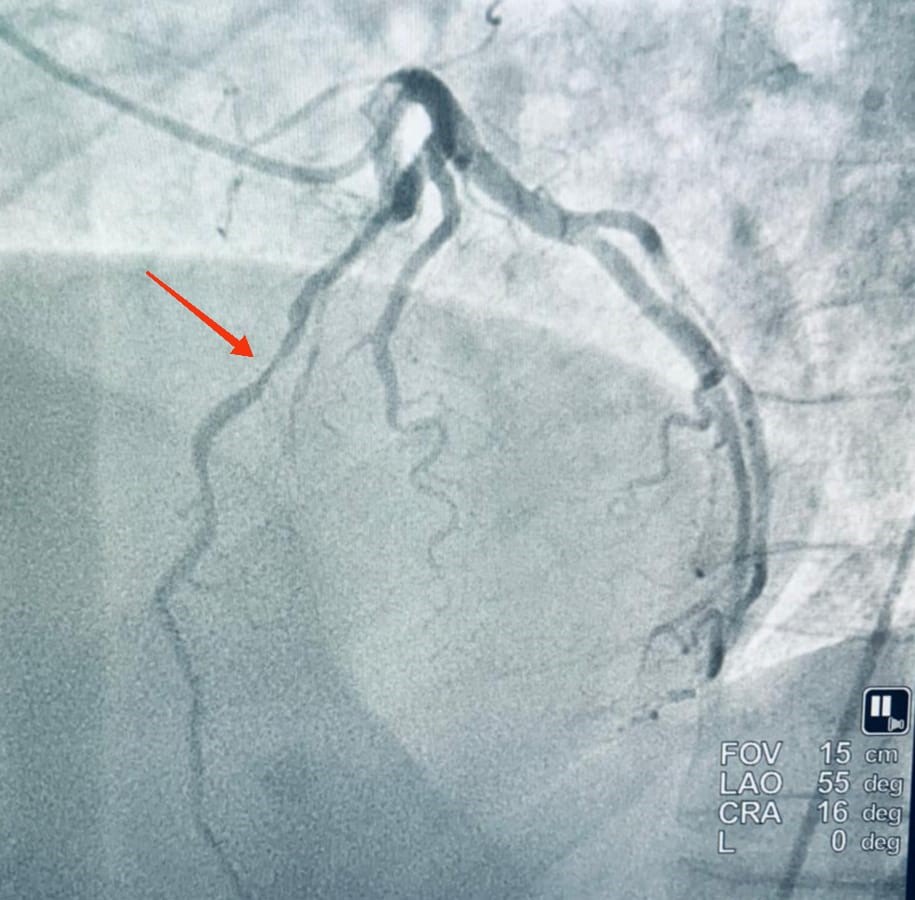
Coronary angiography showed severe systolic narrowing of the anterior interventricular artery in its distal segment.
She received medical treatment with a beta blocker with good clinical improvement.
Discussion
The coronary circulation is epicardial passing through the coronary furrows, this being the case, the arteries are unscathed during the contraction of the muscle during systole and fill during diastole. It turns out that some patients have path abnormalities in segments of one of the arteries, frequently VIA.
Thus the Myocardial Bridge is defined as being a segment of coronary artery covered, in its epicardial path, by a band of myocardium, thus forming a "bridge" (bridge) over this vascular portion. In clinical practice, this corresponds to a coronary artery entity characterized by systolic compression of the coronary heart: this is the milking effect [1].
The first anatomical description of myocardial bridges was made by Reyman in 1737 [2], then by then by Black in 1805. Finally. This description was subsequently reported during Geiringer's post-mortem examination in 1951 [3] and the first radiological description by Portsmann and Iwig in 1960 [1].
PM is a fairly common congenital anomaly of a coronary artery, the most affected of which is VIA.
PM appears to alter the hemodynamics of the coronary circulation in some people. The clinical expression of these abnormalities varies from patient to patient, and most patients are asymptomatic. However, cases of ischemia or myocardial infarction, or even sudden death, have been reported [4] such is the case of our patient who had acute coronary syndrome in hospital following the milking effect.
Gould et al. [5] classified the myocardial bridge into two categories: the superficial bridge, with a depth of 1 to 2 mm, and the deep bridge, with a depth greater than 2mm in the myocardium. Another classification of myocardial bridges is based on the orientation of the myocardial fibers on the segment of the bridge.
As for Loukas et al. [6] and Ferreira et al. [7] described the superficial myocardial bridge as myocardial fibers crossing the IVA transversely at an acute angle or perpendicularly and the deep bridges as fibers crossing and surrounding the IVA.
Moreover Corban et al. [8]: The myocardial bridge is complete when the VIA is completely covered with myocardial tissue, and incomplete when the bridge segment is covered only with a thin layer of connective tissue and fatty tissue.
The clinical manifestation is according to the anatomy of the segment concerned, as well as by the concomitant atheromatous changes and a possible myocardial ischemia that the authors Ferreira AG, Ge J et al [7,9] report in their articles as the contraction of the overlying myocardium compresses the artery; this compression may persist in diastole, when the majority of coronary blood flow occurs. Increased heart rate, short diastolic infusion time, increased myocardial contractility and blood flow rate, as well as exercise-induced coronary spasm can all cause ischemia in patients. with PM. This explains the chest pain reported by our patient in connection with ischemia in the territory of the VIA whose bypass segment underwent a milking effect, like the case reported by A.R Zeina in their article [10].
Our patient was treated medically depending on whether the management of PM falls under either pharmacology, or catheterization by endovascular treatment or by vascular surgery. The pharmacology is made of b-blockers and calcium channel blockers. Indeed, their negative inotropic properties explain the decrease in systolic coronary compression induced by PM. Nitrates are strictly prohibited because they induce tachycardia, an inotropic response and they increase the angiographic degree of the systolic stricture where the symptoms worsen [1,10].
As for endovascular treatment, the placement of a Multilink type stent (chosen for their ability to resist external compression) [11,12] is even better than pharmacological one. By default of the availability of the Multilink stent, we then opted to put our patient on beta-blocker.
Surgical treatment, by dissection of the overlying myocardium or by coronary artery bypass grafting, is recommended for patients with recurrent and severe symptoms that persist despite medical treatment 10.
Conclusion
Under regular sub-extreme exposure of the organism to psychoactive substance, the mechanism of "advanced excitation" allows to maintain the activity of the sympathetic VNS, leads to hypertrophy of the adrenal cortex.
Under regular sub-extreme exposure to psychoactive substance, adaptive maintenance of sympathetic VNS activity and adaptive hypertrophic changes in the endocrine system lead to an increase in the tolerance of the body.
In psychoactive substances dependence, due to the adaptive activity of the sympathetic VNS, adaptive hypertrophy and hyperproductivity of the endocrine system, potentially extreme doses have a nonpathogenic sub-extreme effect on the human organism.
Dependence of the body on psychoactive substances due to the increased tolerance of the organism and the transformation of the effect of potentially extreme doses into the sub-extreme effect is the adaptation process.
Recommendations
It is necessary to validate the dependence of the body on psychoactive substances not as a disease, but as a state of progredient adaptation.
References
- Rousseau AF, Mievis E. Image of the month: under the myocardial bridge flows the coronary artery. Rev Med Liege, 2003; 58: 10: 601-604.
- Alegria JR, Herrmann J, Holmes DR, et al. Myocardial bridg- ing. Eur Heart J, 2005; 26 (12): 1159-1168.
- Geiringer E. The mural coronary. Am Heart J, 1951; 41(3): 359-368.
- Bourassa MG, Butnaru A, Lesperance J, Tardif JC. Symptomatic myocardial bridges: overview of ischemic mechanisms and current diagnostic and treatment strategies. J Am Coll Cardiol, 2003; 41: 351-359.
- Gould KL, Johnson NP. Myocardial bridges: lessons in clin- ical coronary pathophysiology. JACC Cardiovasc Imaging. 2015; 8(6): 705-709.
- Loukas M, Curry B, Bowers M, et al. The relationship of myocardial bridges to coronary artery dominance in the adult human heart. J Anat, 2006; 209(1): 43-50.
- Ferreira AG, Trotter SE, König B, et al. Myocardial bridges: morphological and functional aspects. Br Heart J. 1991; 66(5): 364-367.
- Corban MT, Hung OY, Eshtehardi P, et al. Myocardial bridging: contemporary understanding of pathophysiology with implications for diagnostic and therapeutic strategies. J Am Coll Cardiol, 2014; 63(22): 2346-2355.
- Ge J, Jeremias A, Rupp A, Abels M, Baumgart D, Liu F, et al. New signs characteristic of myocardial bridging demonstrated by intracoronary ultrasound and Doppler. Eur Heart J 1999; 20: 1707-1716.
- Zeina AR, et al. Acute myocardial infarction in a young woman with normal coronary arteries and myocardial bridging. The British Journal of Radiology, 81 (2008), e141 – e144.
- Bayes A, Marti V, Augé JM. Coronary stenting for symptomatic myocardial bridging. Heart, 1998; 80: 102-103.
- Prendergast BD, Kerr F, Starkey IR. Normalization of abnormal coronary fractional flow reserve associated with myocardial bridging using an intracoronary stent. Heart, 2000; 83: 705-707.

