Brain Abscess Caused by Nocardia Thailandica Infection in SLE Patient
Ryokichi Yagi*, Yukimasa Ooi, Takayasu Suzuka, Ryo Hiramatsu, Naokado Ikeda, Naosuke Nonoguchi, Motomasa Furuse, Akira Ukimura, Shinji Kawabata, Masahiko Wanibuchi
Department of Neurosurgery and Endovascular Therapy, Osaka Medical and Pharmaceutical University, Japan.
Department of infection control and prevention, Osaka Medical and Pharmaceutical University, Japan.
Department of Internal Medicine IV, Osaka Medical and Pharmaceutical University, Japan.
Department of Neurosurgery and Endovascular Therapy, Osaka Medical and Pharmaceutical University, Japan.
Department of Neurosurgery, Takeda General Hospital, Japan.
Department of Neurosurgery and Endovascular Therapy, Osaka Medical and Pharmaceutical University, Japan.
Department of infection control and prevention, Osaka Medical and Pharmaceutical University, Japan.
Department of Neurosurgery and Endovascular Therapy, Osaka Medical and Pharmaceutical University, Japan
Received Date: 29/11/2021; Published Date: 27/12/2021
*Corresponding author: Ryokichi Yagi M.D., Ph.D., Department of Neurosurgery and Endovascular Therapy, Osaka Medical and Pharmaceutical University, 2-7 Daigaku-machi, Takatsuki City, Osaka, Japan
Abstract
A brain abscess was found in a patient with systemic lupus erythematosus who had been receiving steroids for a long time. An actinomycete suspected to belong to the genus Nocardia was detected in the abscess, and a brain abscess caused by Nocardia thailandica (N. Thailandica) was diagnosed using matrix assisted laser desorption ionization time of flight mass spectrometry (MALDI-TOFMS). He died during the course of treatment and his organs were examined by autopsy. N. thailandica was not detected, so it was concluded that the bacterial death due to long-term administration of antibiotics was the cause of death. N. thailandica is a very rare bacterium belonging to Nocardia asteroids, and is said to easily form brain lesions. In immunocompromised patients, prophylaxis with antibiotics and detailed examination of lung lesions for surveillance were considered necessary. This paper is the first report of a brain abscess caused by Nocardia thailandica (N. thailandica), including a review of the literature.
Keywords: Brain abscess; Nocardia; Nocardia thailandica; Systemic Lupus Erythematosus (SLE)
Introduction
Opportunistic infections occur more frequently, or are more severe, in people with weakened immune systems (such as people with HIV); these can be life-threatening and cause severe complications in patients receiving long-term treatment with immunosuppressants and steroids. Nocardia, a naturally occurring actinomycete, cannot be detected by culture tests and, thus, requires genetic analysis. In human, almost 90% of Nocardia infections are caused by the Nocardia asteroides group. Nocardia thailandica (N. Thailandica) is an extremely rare bacterium related to Nocardia asteroids. Of note, N. thailandica’s drug sensitivity is relatively good, and its standard treatments are β-lactam antibiotics, Sulfamethoxazole/Trimethoprim (ST) combination, tetracycline, and macrolides. To the best of our knowledge, this is the first clinical report of an N. thailandica-associated brain abscess. In our case, after the diagnosis of an N. thailandica-associated brain abscess, the original disease was ameliorated by the administration of antibiotics; however, the patient died from microbial substitution caused by prolonged administration of antibiotics.
Case Report
A 69-year-old male with Systemic Lupus Erythematosus (SLE) presented with a chief complaint of nausea and gait disorder. The patient’s eldest daughter also had SLE. He had no smoking history, no drinking, no travel history, no outdoor activities, and no sexual activity.
The patient’s current medical history was as follows. The patient became aware of dyspnea and edema of the lower extremities during exercise; thus, he consulted a family doctor. The examination revealed hypertension, proteinuria, and hematuria. A chest X-ray revealed bilateral pleural effusion. Because of an increase in antinuclear antibodies (Anti-ds-DNA antibody 218.5) and a decline in complement (C3 51, C4 12.3), a connective tissue disease was suspected, and the patient was referred to our Department of Rheumatic Collagen Disease. After two months, he was hospitalized for examination and diagnosed with SLE because of (i) renal lesions, (ii) leukopenia, (iii) positive anti-ds-DNA antibody, and (iv) positive antinuclear antibody. Based on the renal biopsy results two months later, he was diagnosed with lupus nephritis class IV. Accordingly, steroid pulse therapy (methylprednisolone, 1000 mg) and tacrolimus (2 mg/day) were initiated intravenously. As SLE and lupus nephritis improved, the patient received prednisolone (25 mg/day) + tacrolimus (2 mg/day) + azathioprine (100 mg/day) orally and was discharged after six months. He returned for follow-up as an outpatient.
After one year, the patient visited a family doctor for nausea and dizziness. A brain Computed Tomography (CT) revealed a multilocular cystic lesion with edema. Thus, he was referred to our department for neurosurgery.
On day 1 of admission, we suspected a cerebral abscess because a multilocular cystic lesion, which was imaged in a ring shape, was observed on the enhanced magnetic resonance imaging examination (Figure 1A and B). On day 10 of admission, the cranial brain abscess was excreted by burr hole surgery used by stereotactic Techniques, and intravenous meropenem (MEPM; 1 g TID) + vancomycin (0.5 g BID) was started postoperatively. Of note, Gram-positive bacilli, suspected to be actinomycetes, were detected in the puncture fluid collected intraoperatively. Since the culture specimen was positive for Kinyoun staining, Gram-positive bacilli were found to belong to the Nocardia genus (Figure 1C and D). On day 15 of admission, vancomycin was discontinued because it was later determined as N. thailandica based on the 16S rRNA sequence and matrix-assisted laser desorption ionization time-of-flight mass spectrometry (MALDI-TOFMS; Figure 2A and B). The change to an ST combination was considered, but the patient had an allergic function. Hence, intravenous MEPM (1 g TID) was continued. On day 20 of admission, a blood test revealed improved inflammatory response, but renal function had deteriorated, resulting in decreased MEPM (1 g BID).
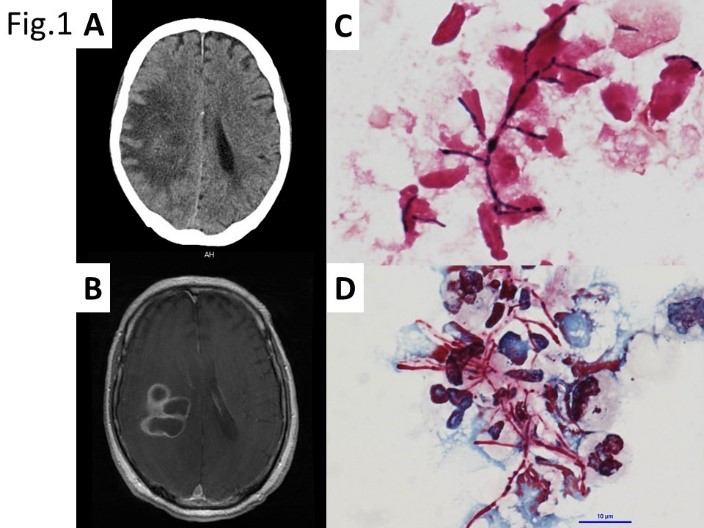
Figure 1:
A/B: Preoperative brain CT and MRI revealed that polycystic ring-enhancing lesions with surrounding vasogenic edema located in the right parietal lobe.
C: Gram stain for brain pus, showing Gram-positive actinomyces with beaded staining pattern.
D: Kinyoun smear stain, showing a cluster of filamentous branching rods that are partially acid fast, which is characteristic for Nocardia.
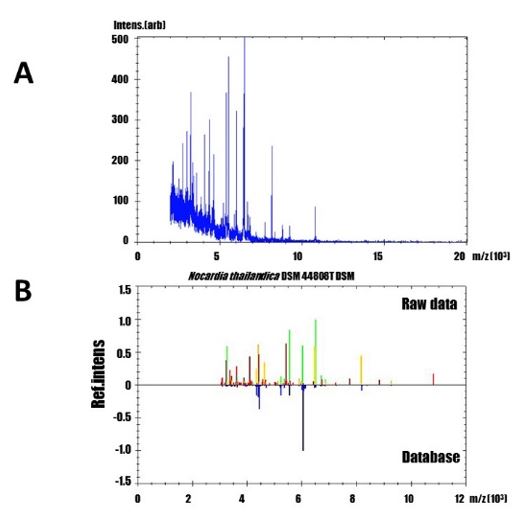
Figure 2:
A: MALDI-TOF mass spectra of the extract from a patient’s abscess
B: Nocardia thailandica (identification score: 1.731)
The comparison between the raw MALDI-TOF mass spectra and the most possibility reference mass spectra. Yellowish-green, yellowish and reddish spectra indicated as correct, possible and difference to the reference mass spectra of the database, respectively.
The patient remained hospitalized for 30 days without further deterioration of renal function; however, consciousness disorder appeared because of deteriorating central nervous system lupus. Consequently, oral administration became difficult; thus, we switched to ceftriaxone (CTRX; 2 g BID) intravenously. A brain CT revealed that the brain abscess had decreased gradually. Treatment of the abscess and SLE was progressing smoothly. However, on day 77 of admission, the patient developed a catheter-associated urinary tract infection and catheter-associated bloodstream infection due to Corynebacterium striatum and extended spectrum β-lactamase (ESBLs) Escherichia coli. Gradually, the patient’s condition worsened, and he died 86 days after admission. After death, a pathological autopsy was performed with the approval of the patient’s family. We established the formation of microabscesses in the lungs, mitral valve, liver, and kidneys; however, no Gram-positive bacilli suspected of being Nocardia were detected in the brain or other organs. Since filamentous fungi, suspected of Aspergillus, and yeast-like fungi, suspected of Candida, were detected in the abscesses and blood vessels, the cause of death was established as aspergillosis and disseminated candidiasis due to bacterial replacement caused by the prolonged administration of antibiotics (Figures 1-3).
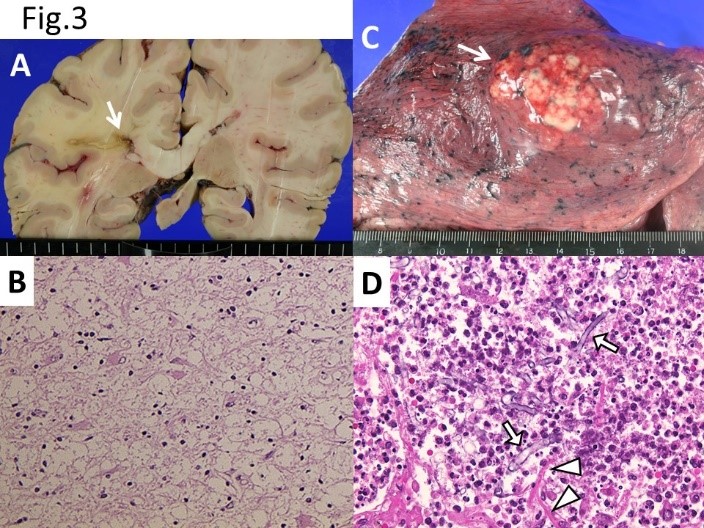
Figure 3:
Post-mortem specimens of the patient.
A: Gross brain section showing a collapsed abscess in right parietal lobe.
B: H.E. stain revealed that no viable bacteria was in and around the cerebral abscess.
C: Gross appearance of lung, showing an abscess occupying the right inferior lobe.
D: Aspergillus (arrow) and Candida (arrow head) genus were seen in the lung abscess stained with H.E. (×100)
Discussion
Nocardia is an aerobic gram-negative bacillus belonging to the order Actinomycetes and is found in soil, water, rotten plants, and animal excrement. Although infections in healthy individuals have been reported, more than 60% have some underlying diseases, and are said to be opportunistic infections that develop in an immunocompromised state with reduced cellular immunity [1]. There are more than 80 bacterial species in the genus Nocardia, N. thailandica was first clinically reported for ocular nocardiosis in 2004, and pulmonary Nocardia was clinically reported in 2014 [2,3]. The clinical infection route is classified into a skin type of wound infection and a visceral type of airway infection. Nocardia brain abscess is caused by blood flow dissemination from lung lesions [4]. Brain abscesses account for 15-44% of all Nocardia infections, and Nocardia brain abscesses are extremely rare, accounting for 2% of all brain abscesses [5]. Since the efficacy of ST combination therapy was reported, the first choice of antibiotic is ST combination with or without brain abscess; however, if it cannot be used because of side effects like liver damage, IPM, AMK, MINO, and CTRX could be used [6]. Visceral Nocardia is said to have a minimum of 6 months of antimicrobial administration, central Nocardia requires a minimum of 12 months of administration, and the period is further extended in patients who received steroids and immunosuppressants It is stated in the book that it is necessary [7]. Regarding the prognosis, the 6-month survival rate of 74% was favorable for all nocardiosis due to the use of ST combination [8]. The Nocardia brain abscess was 54% in a single case with 33% mortality, 38% in multiple cases with 66% mortality, which is inferior to other bacterial brain abscesses (10% mortality) [9].
Since intestinal mucosal disorders occur in patients treated with steroids and antitumor drugs, it has been reported that Candida, which is a resident bacterium of the digestive tract, invades the body due to microbial substitution disease due to long-term antimicrobial administration [10]. This case was treated with N. thailandica for 10 weeks or longer by long-term administration of antibacterial drugs. N. thailandica was not detected by autopsy, and abscess formation due to Candida and Aspergirus was observed. Therefore, it was strongly suspected that multiple organ infection due to the bacterial replacement phenomenon occurred.
Opportunistic infections such as Nocardia are a serious complication for immunocompromised patients. In addition, long-term administration of antibacterial drugs in patients who need to continue administration of steroids and immunosuppressive drugs may cause other infections due to bacterial replacement phenomenon. Although it is of course possible to prevent opportunistic infections, early detection is important. We think that it is necessary to perform CT examinations regularly instead of simple X-ray examinations so as not to miss microscopic lesions4. If any infection is suspected, antibiotics should be started early and, if possible, temporary discontinuation of steroids and immunosuppressants should be considered.
This case developed a brain abscess due to an opportunistic infection with N. thailandica during long-term steroid administration to SLE. This is the first case of a brain abscess of N. Thailandica because we were able to identify N. Thailandica using genetic analysis of the isolate. Although the patient was lost due to the bacterial replacement phenomenon associated with treatment, it is a valuable case to report.
Conflicts of Interest: The authors declare no conflicts of interest associated with this manuscript.
Grant Information: The authors received no specific funding for this work.
Acknowledgements: We are grateful to Dr. *** for helpful discussions ...
References
- Edwards U, Rogall T, Blocker H, Emde M, Bottger EC. Isolation and direct complete nucleotide determination of entire genes. Characterization of a gene coding for 16S ribosomal RNA. Nucleic acids research, 1989; 17(19): 7843-7853.
- Kageyama A, Yazawa K, Ishikawa J, Hotta K, Nishimura K, Mikami Y. Nocardial infections in Japan from 1992 to 2001, including the first report of infection by Nocardia transvalensis. European journal of epidemiology, 2004; 19(4): 383-389.
- Kageyama A, Yazawa K, Nishimura K, Mikami Y. Nocardia testaceus sp. nov. and Nocardia senatus sp. nov., isolated from patients in Japan. Microbiology and immunology, 2004; 48(4): 271-276.
- Beaman BL, Burnside J, Edwards B, Causey W. Nocardial infections in the United States, 1972-1974. The Journal of infectious diseases, 1976; 134(3): 286-289.
- Malincarne L, Marroni M, Farina C, et al. Primary brain abscess with Nocardia farcinica in an immunocompetent patient. Clinical neurology and neurosurgery, 2002; 104(2): 132-135.
- Jodlowski TZ, Melnychuk I, Conry J. Linezolid for the treatment of Nocardia spp. infections. The Annals of pharmacotherapy, 2007; 41(10): 1694-1699.
- McBride WJH. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases, 7th edition. Sex Health. 2010; 7(2): 218-218.
- Kurahara Y, Tachibana K, Tsuyuguchi K, Akira M, Suzuki K, Hayashi S. Pulmonary nocardiosis: a clinical analysis of 59 cases. Respiratory investigation, 2014; 52(3): 160-166.
- Mamelak AN, Obana WG, Flaherty JF, Rosenblum ML. Nocardial brain abscess: treatment strategies and factors influencing outcome. Neurosurgery, 1994; 35(4): 622-631.
- Torack RM. Fungus infections associated with antibiotic and steroid therapy. The American journal of medicine, 1957; 22(6): 872-882.

