A Rare Presentation of Extra-Articular Ganglion Cyst Formation Around the Knee
Julian Scherer*, Thomas Rauer
University Hospital of Zurich, Department of Traumatology, Raemistr. 100, 8091 Zürich, Switzerland.
Received Date: 22/11/2021; Published Date: 22/12/2021
*Corresponding author: Julian Scherer, Department of Traumatology, University Hospital of Zurich, Raemistr. 100, 8091 Zürich, Switzerland.
Abstract
Introduction: Extra-articular soft tissue ganglion cysts of the knee occur very rarely. We present a case of a lateral anteroinferior cystic ganglion system with communication to intra-articular in a 61-year-old female.
Presentation of Case: 61-year-old female with extra-articular cyst formation on the anterior inferolateral right knee. Open excision of the ganglion system as well as closure of the intra-articular portal has been performed in combination with diagnostic arthroscopy and resection of concomitant intra-articular pathologies. The patient recovered well, and no re-occurrence has been detected.
Discussion: MR-imaging remains the gold standard for diagnosing extra-articular ganglion cyst formations to detect intra-articular connection. Open surgical exploration, excision and closure of the intra-articular portal has been suggested in order to prevent reoccurrence. Concomitant intra-articular lesions should be addressed arthroscopically.
Conclusion: Adequate pre-operative imaging is of utmost importance. Extra-articular ganglion systems should be explored surgically and portal to intra-articular should be closed. To assess intra-articular pathologies, arthroscopy is suitable.
Keywords: Arthroscopy; Knee; Ganglion cyst; Case report
Introduction
Ganglion cysts around the knee joint can be classified into intra-articular, extra-articular, periosteal and intra-osseous lesions [1]. Extra-articular soft tissue ganglion cysts of the knee have only been reported rarely and seem to occur quite uncommonly [2]. MRI is the diagnostical gold standard for these lesions and extra-articular ganglion cysts can be easily mistaken for meniscal cysts or synovial cysts and are mostly reported in conjunction with peroneal nerve palsy and bony remodeling in arthrosis [3-5]. The most common extra-articular cysts around the knee joint are baker cysts and intra-articular communication has been reported in up to 65% of the cases [6]. We present a case of a lateral anteroinferior conglomerate of cystic ganglion lesions with communication to intra-articular in a 61-year-old female.
Case Report
We report on a 61-year-old female patient who was referred to our department of traumatology from the department of dermatology within the University Hospital of Zurich in August 2018. The patient described cystic changes of the right lateral proximal lower leg since approximately one year. Initially, according to the patient, there was one large cyst which burst and subsequently, multiple new smaller cysts occurred. These small cysts are intermittently progressive in size with independent regress. She did not report any impairment of every-day life, nor pain or gaiting problems but felt disturbed by means of cosmetics. On physical examination, there was no pain, full range of motion, no clinical signs of lesions to the menisci, no clinical signs of joint effusion, no axis deviation or pain in valgus or varus stress. Also, the cruciate ligaments were unobtrusive and clinically, no signs of inflammation were present. The only abnormality found in the clinical examination was multiple cystic soft tissue tumors located on the lateral proximal right lower leg. The previously performed MRA (Magnetic Resonance Angiography) revealed subcutaneous tubular cystic lesions in close proximity to the lateral joint space, consistent with a ganglion system originating from the lateral knee joint (Figure 1). We suggested arthroscopy of the right knee and complete resection of the cystic lesions. The patient agreed to the suggested procedure. Two months later, the preoperative follow-up did not reveal any clinical changes (Figure 2). We then performed a total open excision of the ganglion system under general anesthesia and preoperative antibiotic prophylaxis. We took tissue samples for histological work-up as well as bacteriological swabs for further testing. After closure of the ganglion neck which had a connection to intra-articular (Figure 3), the wound was closed in standard fashion. We then performed a diagnostic arthroscopy which revealed grade 2-3 chondromalacia according to Outerbridge [7] in the lateral and medial condyles of the femur and bilateral tibial plateau. Furthermore, degenerative changes of the posterior patella as well as moderately irritated mucous membranes of the recessus. We also found some scar tissue pulling from the lateral meniscus to the base of the anterior cruciate ligament which we carefully resected. Other than that, no pathologies were found in the arthroscopy. Histological work-up revealed a simple ganglion system without any malignancy. In the bacteriological testing, no aerobic or anaerobic growth and no microorganisms were detected. The patient was discharged 2 days after surgery in a good state with full weight bearing of her right leg. Three months after the initial operation, the patient presented at our outpatients` clinic because of a new non-fluctuating, small, non-painful swelling on the right proximal lower leg (Figure 4). No wound-healing problems, no impairment of work- or daily-life were present. Peripheral perfusion, sensory and motor functions were normal. Clinically, we suggested non-specific swelling but considered reoccurrence of the previously excised ganglion and treated it with local application of heparin-diclofenac-plaster. 4 weeks later, the patient was seen again, and the swelling appeared to be reduced, the patient had no complaints, and we closed the case.

Figure 1: Pre-operative MRI (axial) from proximal (A) to distal (I), arrow = intra-articular portal.
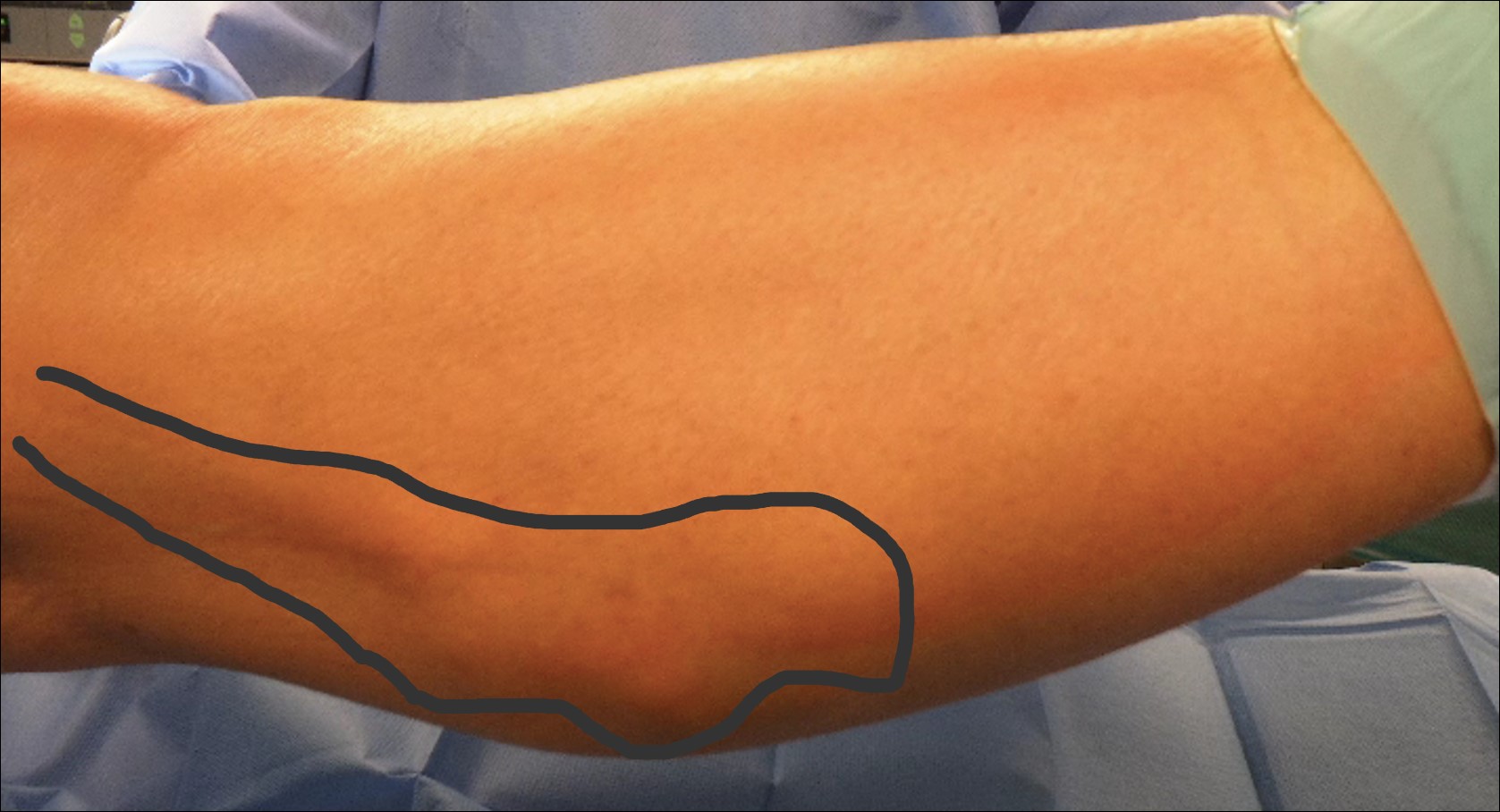

Figure 3: Intra-operative photograph.
A: In toto excision of the ganglion system; B: Closure of the intra-articular portal

Discussion
We presented a case of spontaneous subcutaneous ganglion cyst-formation of the right proximal lower leg with connection to the knee joint. Except for Baker`s cysts, extra-articular ganglion lesions around the knee are a rare entity and clinical studies are lacking [1]. Popliteal cysts show a high incidence of intra-articular communication and also a high incidence of intra-articular lesions [6, 8, 9]. A study, assessing extra-articular ganglion cysts around the knee joint found that also these lesions have a high incidence of intra-articular pathologies (69.6%) and that only 43% of the extra-articular ganglion cysts showed connections to intra-articular, which shows the rare character of this pathology [1]. MRI of the knee is of utmost importance in order to detect the extent of the lesions as well as communication to intra-articular as failure to remove the intra-articular connection surgically can lead to reoccurrence [10-12]. The presented case showed a multilocular ganglion cyst system around the right knee-joint and MRI revealed connection to intra-articular. We were able to excise the lesion in open surgery and ligate the stalk of the cystic formation. Afterwards, arthroscopy was performed to assess and address concomitant intra-articular lesions and the patient did not show any reoccurrence. Arthroscopy following open excision or vice versa has been proposed by other authors and we believe that this mode of procedures should be performed to avoid recurrent lesions in the long run [1].
Conclusion
The reported case emphasizes the importance of adequate preoperative imaging as well as the importance of surgical exploration with closure of the cyst portal to intra-articular. Furthermore, intra-articular pathologies resulting in chronic irritation should be addressed arthroscopically in order to prevent reoccurrence.
Conflict of Interest
No conflict of interest is reported by the authors.
Funding
No funding has been received.
Ethical approval
Not applicable.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Author contributions
Julian Scherer: conceptualization, drafted and wrote the manuscript
Thomas Rauer: operated the patient, took the photographs, substantial contributions to the conception of the work, reviewed the manuscript
References
- Park SE, et al. Extra-Articular Ganglion Cysts around the Knee Joint. Knee Surg Relat Res, 2015; 27(4): p. 255-262.
- Bui-Mansfield LT, Youngberg RA. Intraarticular ganglia of the knee: prevalence, presentation, etiology, and management. AJR Am J Roentgenol, 1997; 168(1): p. 123-127.
- Butler MG, Fuchigami KD, Chako A. MRI of posterior knee masses. Skeletal Radiol, 1996; 25(4): p. 309-317.
- Larbi A, et al. Imaging of tumors and tumor-like lesions of the knee. Diagn Interv Imaging, 2016; 97(7-8): p. 767-777.
- Desy NM, et al. Intraneural ganglion cysts: a systematic review and reinterpretation of the world's literature. J Neurosurg, 2016; 125(3): p. 615-630.
- Bickel WH, Burleson RJ, Dahlin DC. Popliteal cyst; a clinicopathological survey. J Bone Joint Surg Am, 1956; 38-A (6): p. 1265-1274.
- Outerbridge RE. The etiology of chondromalacia patellae. J Bone Joint Surg Br, 1961. 43-b: p. 752-757.
- Fielding JR, Franklin PD, Kustan J. Popliteal cysts: a reassessment using magnetic resonance imaging. Skeletal Radiol, 1991; 20(6): p. 433-435.
- Miller TT, et al. MR imaging of Baker cysts: association with internal derangement, effusion, and degenerative arthropathy. Radiology, 1996; 201(1): p. 247-2 50.
- Kim JY, et al. Extra-articular soft tissue ganglion cyst around the knee: focus on the associated findings. Eur Radiol, 2004; 14(1): p. 106-111.
- Burk DL Jr, et al. Meniscal and ganglion cysts of the knee: MR evaluation. AJR Am J Roentgenol, 1988; 150(2): p. 331-336.
- Malghem J, et al. Ganglion cysts of the knee: articular communication revealed by delayed radiography and CT after arthrography. AJR Am J Roentgenol, 1998; 170(6): p. 1579-1583.

