Severe Postpartum Hemorrhage After a Vaginal Delivery: A Retrospective Study About 55 Cases
Dahmani Hela, Toumi Dhekra, Khouildi Ghada, Ouali Masarra, Hnain Asma, Zoukar Olfa, Hajji Ahmed, Felah Raja
Department of Gynecology and Obstetrics, Regional Hospital of Kasr Hlel, University of Monastir, Tunisia.
Maternal and Neonatal center of Monastir, University of Monastir, Tunisia.
Received Date: 14/11/2021; Published Date: 10/12/2021
*Corresponding author: Dahmani Hela, Department of Gynecology and Obstetrics - Hospital of Kasr Hlel, University of Monastir, Tunisia
Introduction
Postpartum Hemorrhage (PPH) is one of the most feared complications in obstetrics, it remains a major public health problem. It is the first cause of maternal mortality in the world, including in developed countries.
Objective
To identify the risk factors as well as the epidemiological profile of parturient who presented with PPH after vaginal delivery in order to reduce maternal morbidity and mortality from PPH.
Methods
This is a retrospective descriptive study. A 55 cases of parturient who presented a severe HPP after a vaginal delivery have been collected during a period of three years.
Results
The prevalence in our population was 0.44% and the median age was 30.07 ± 0.74 years.
A history of a cesarean section was found in 87% of cases. The estimated fetal weight (EWP) was greater than 4000g in 14.5℅ of our parturient and the average time of labor was 5.84 hours.
Uterine atony and cervicovaginal tears were the two most common etiologies found in our sample, knowing that a parturient can have one or more causes of PPH (Figure 1).
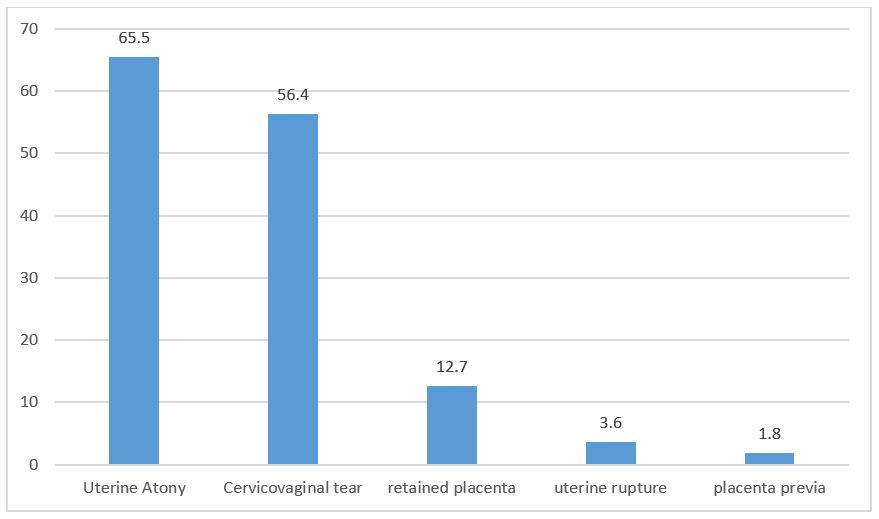
Figure 1: Etiologies of severe HPP.
The management of all our PPH cases was carried out in the operating room. All of our parturient had undergone uterine revision followed by uterine massage. Retained placenta and uterine rupture were revealed in 9 cases.
All included patients had undergone a birth canal examination, vascular filling, and a maximum dose of Syntocinon (40 IU). Sulprostone (Nalador) was administered to 69.1% of parturient.
Three parturient had received Misoprostol (Cytotec) at a dose of 4 tablets.
81.8% of parturient had received Tranexamic acid (Exacyl) and 60% had received fibrinogen.
When it comes to surgical procedure the triple vascular ligation was performed in 10.9% of parturient rarely the Hemostatic hysterectomy which was performed in only in 3.6% of patients.
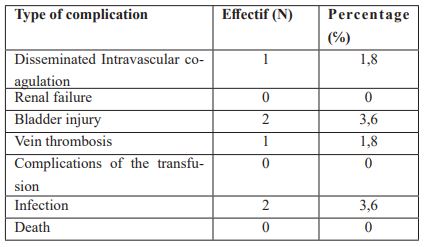
As a complication of the severe PPH, only one patient presented with disseminated intravenous coagulation (DIC). Two patients had an accidental bladder injury and were repaired. No case of maternal death was noted in our series (Table 1).
Table 1: Complications of severe HPP.
Discussion
Postpartum hemorrhage is defined by any bleeding from the genital tract greater than 500 ml or more within 24 hours of fetal expulsion, whether by vaginal or cesarean section [1].
In the most recent update of the WHO recommendations, the difference in blood loss thresholds between vaginal or c /section delivery is not mentioned, the PPH is defined globally for all type of deliveries [2,3].
The existence of different definitions of PPH and the subjective nature of assessing blood loss make it difficult to accurately estimate its frequency. This frequency remains high. In fact, in a meta-analysis carried out in 2009 [4], the frequency is 10.8%. In the United States, the frequency of PPH is 2.7% [5], in France 6.4% [3], in Tunisia, this frequency is 1.19% in a maternity hospital in Tunis [6] and 1.01% in our series (this frequency relates to PPH treated surgically in our country). The incidence of PPH in our public hospitals is between 0.25% and 1.22% of deliveries. In our series, the incidence of severe PPH was 0.44%. The incidence varies according to the characteristics of the maternity unit studied (regional hospital, reference university structure, etc.) [7]. The results of an online survey show that currently 23.9% of obstetricians manage one PPH per week and 25.2% one PPH per month.
Although PPH most often occurs unpredictably, some situations have been identified as being at high risk for bleeding. It is also fundamental to remember that these risk factors are often entangled. The main factors to look for are: low socioeconomic level, multiparity, scarred uterus, history of bleeding, fetal macrosomia and poorly monitored pregnancies. In our study, the mean parity was 2.22 ± 1.18 with extremes ranging from 1 to 5, the history of a scarred uterus was found in 13% of cases and operative delivery was performed in 14, 5% of parturients.
The main etiologies are often classified into four broad categories summarized by the mnemonic of the four T's: Tonus, Trauma, Tissue and Thrombin. It should be noted that uterine atony is the most common cause and that together with retained placenta tissue and lesions of the genital tract, they account for 95% of the causes of PPH. Bleeding disorders are rarely a primary cause (<1%) but often the consequence of a severe PPH of another origin which aggravates the latter [8]. In our series, uterine atony was the most common etiology of PPH (65.5% of patients), genital tract lesions were noted in 56.4% of cases and uterine rupture was noted in 3.6. %.
The initial stage involves early detection of the bleeding. The diagnosis is facilitated by the placement of collection bags placed after fetal expulsion. From the diagnosis, communication of the latter must be immediate to all potential contributors (obstetricians, midwives, anesthesia team), the optimal management being multidisciplinary [9].
Surgical treatment is performed by senior gynecological surgeons. Different techniques can be performed and the choice of technique, the order of performance and the combination of surgical techniques varies according to the etiology of the bleeding, the hemodynamic state of the patient, her parity and finally the surgeon's habits.
“Success” is defined as the cessation of bleeding with survival of the patient and “failure” by the persistence of bleeding and the need for another technique or the loss of the patient.
A hemostatic hysterectomy is the last resort if obstetric treatments, ligation or padding have failed. It can be total or subtotal. The incidence of hysterectomy varies in the literature from 0.24% o to 1.25% of deliveries. It is particularly high in underdeveloped countries compared to that of developed countries [10]. In our series, hemostatic hysterectomy was performed in 3.6% of parturients.
PPH, a preventable cause, remains the leading cause of maternal mortality in the world (140,000 deaths per year or one woman every 4 minutes): 33.9% of maternal deaths in Africa, 30.8% in Asia and 20.8 % in Latin American countries [11]. Maternal mortality from PPH varies in Tunisia, from 27.6% to 50% of maternal deaths. In our series, no case of maternal death was noted.
Maternal mortality is indeed an important indicator of maternal health, reflecting both access to and the quality of prenatal and obstetric care [12].
Primary prevention of PPH involves prenatal screening for risk factors, correction of anemia, pregnancy monitoring and good monitoring of labor and last the immediate postpartum period. Secondary prevention involves early diagnosis and prompt and adequate management to prevent worsening and maternal death.
Conclusion
In addition to the direct consequences of acute hypovolemia, the PPH exposes the woman to complications following the transfusion, resuscitation, and infertility in cases of hemostatic hysterectomy. The prevention involves raising awareness among the population as well as continuing training for professionals involved in childbirth.
References
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin: Clinical Management Guidelines for Obstetrician-Gynecologists Number 76, October 2006: postpartum hemorrhage. Obstet Gynecol, 2006; 108(4): 1039‑1047.
- Haute Autorité de Santé - Hémorragies du post-partum immédiat, 2020.
- Deneux-Tharaux C, Dupont C, Colin C, Rabilloud M, Touzet S, Lansac J, et al. Multifaceted intervention to decrease the rate of severe postpartum haemorrhage: the PITHAGORE6 cluster-randomised controlled trial. BJOG, 2010; 117(10): 1278‑1287.
- Identifying Regional Variation in the Prevalence of Postpartum Haemorrhage: A Systematic Review and Meta-Analysis, 2020.
- Williams Gynecology, Fourth Edition: 9781260456868: Medicine & Health Science Books, 2020.
- Profil bibliométrique et devenir des thèses soutenues à la faculté de médecine de Monastir (Tunisie), 2020.
- Rafla TD, Souha B, Fayçal BS, Nadia BM, Ahlem G, Ibtissem G, et al. l’enquête nationale tunisienne sur la mortalité maternelle de 2010 : a propos des données de tunis. LA TUNISIE MEDICALE. 2014; 92: 7.
- Netgen. Prise en charge multidisciplinaire des hémorragies du post-partum : nouvelles stratégies [Internet]. Revue Médicale Suisse, 2020.
- Kehila M, Derouich S, Chelli D, Touhami O, Marzouk SB, Khedher SB, et al. Quelle stratégie chirurgicale adopter devant une hémorragie du post-partum et comment améliorer les résultats de la ligature des artères hypogastriques? Pan Afr Med J, 2020.
- Obiechina NJA, Eleje GU, Ezebialu IU, Okeke C a F, Mbamara SU. Emergency peripartum hysterectomy in Nnewi, Nigeria: A 10-year review. Nigerian Journal of Clinical Practice. 2012; 15(2): 168.
- Khouadja H, Rouissi W, Mahjoub M, Sakhri J, Beletaifa D, Jazia KB. Stratégies transfusionnelle des hemorragies graves du post-partum : A tude retrospective propos de 47 cas. The Pan African. Medical Journal 2020; 25(169).
- Ronsmans C, Graham WJ. Lancet Maternal Survival Series steering group. Maternal mortality: who, when, where, and why. Lancet, 2006; 368(9542): 1189‑1200.

