Von Recklinghausen’s Disease Revealed by Pulsatile Exophthalmos with Spheno-Orbital Agenesis
Soufiane Belabbes*, Taoufik Africha, Abdennasser El kharras, Brahim Zainoun
Department of Radiology, Moulay Ismail Military Teaching Hospital, Faculty of Medicine and Pharmacy, Sidi Mohammed ben Abdellah, Fes, Morocco.
Received Date: 03/11/2021; Published Date: 09/12/2021
*Corresponding author: Soufiane Belabbes, Department of Radiology, Moulay Ismail Military Teaching Hospital, Faculty of Medicine and Pharmacy, Sidi Mohammed ben Abdellah, Fes, Morocco
Abstract
Pulsatile exophthalmos secondary to spheno-orbital dysplasia is very rare, always described in Von Recklinghausen's disease. It represents a functional emergency requiring adequate management. Its diagnosis is based on the CT scan which assess bone lesions and the MRI which refines the diagnosis. This article describes the case of a young male with no medical history who presented with a rapid increase pulsatile exophthalmos for two years. we performed a cranial Ct-scan and brain MRI which has objectified a sphenoid agenesis (confirmed by CT scan) associated with a temporal meningocele. A more detailed clinical examination was carried out posteriori which revealed multiple café-au-lait spots, one neurofibroma in the right flank and many axillary freckles. All of these lesions suggestive of neurofibromatosis type 1 with spheno-orbital dysplasia and temporal meningocele.
Keywords: Sphenoid dysplasia; Neurofibromatosis; Pulsatile exophthalmos
Introduction
Orbital manifestations of neurofibromatosis type 1 (NF-1) reflect a mix of CNS, musculoskeletal and ocular disease. Pulsatile exophthalmos with spheno-orbital dysplasia is a rare ophthalmologic expression, often associated with plexiform neurofibroma of the eyelid. It can be revealing the pathology and constitutes a functional emergency. Its main differential diagnosis is carotid-cavernous fistula. CT scan makes bone lesion assessment, and the MRI refines the diagnosis.
Case Report
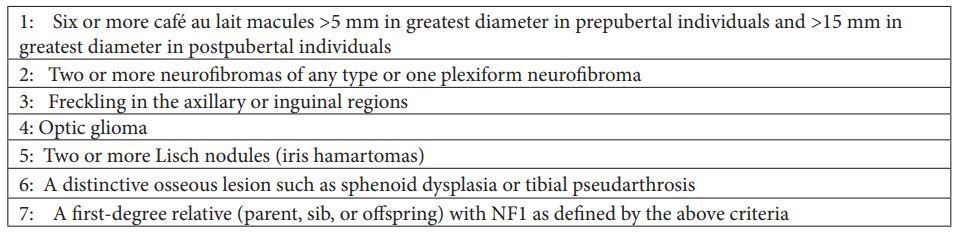
A 32-year-old man, second-born issue of a consanguineous marriage presented with a left eyeball protrusion since the age of 30 years. The patient noticed rapid increase in swelling size in the last 2 years with watering and redness of the left eye. No other medical history or similar family cases were reported. On ophthalmic examination, visual acuity was conserved with normal intraocular pressures in both eyes. The left eye showed pulsating exophthalmos, no Lisch nodules or abnormalities of eyelid were noted. Complete physical examination revealed seven café-au-lait spots with size ranging from 10 to 15 mm in the upper back, abdomen, and shoulders (Figure 1). One neurofibroma was found in the right flank (Figure 1) with many axillary freckles. Cranial CT-scan showed in bone-window a complete absence of the left greater sphenoid wing (Figure 2). Brain MRI revealed orbital meningocele causing grade 3 exophthalmos (Figure 3). The diagnosis of spheno-orbital dysplasia in Von Recklinghausen neurofibromatosis was made. The patient was referred to neurosurgery department for reconstruction of sphenoid defect.

Figure 1: Neurofibroma in the right flank (straight arrow), with café-au-lait spot (curved arrow) and many axillary freckles.
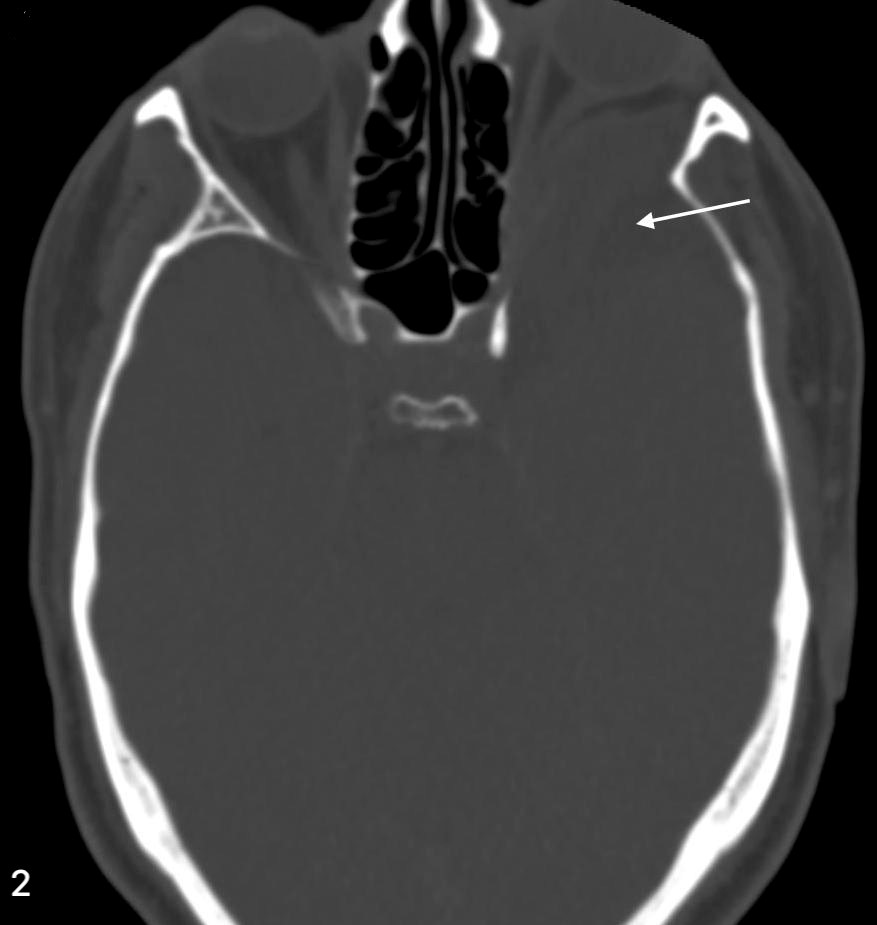
Figure 2: Cranial CT-scan in bone-window showing a complete absence of the left greater sphenoid wing (straight arrow)
Discussion
Pulsatile exophthalmos is a clinical symptom characterized by protrusion and pulsation of the eyeball that can occur due to various causes, dominated by vascular diseases like carotido-cavernous fistulas and arterio-venous malformation, but rarely occur in von Recklinghausen’s disease [1]. Neurofibromatosis type 1 (NF-1), also known as Von Recklinghausen’s disease, is a multisystem neurocutaneous disorder, an autosomal dominant disorder, and inherited tumor syndromes. Additionally, it’s the most common phakomatosis, and a RASopathy [2].
As is the case with many phakomatoses, NF-1 results in a variety of abnormalities of variable severity. It is characterized by a completely unpredictable evolution requiring a regular follow up. According to the National Institute of Health (NIH) Consensus Conference in 1987, a clinical diagnosis of NF-1 may be made if patients demonstrate at least two of the seven cardinal criteria (Table1) [3].
The orbital-palpebral region is the most predilection site of cephalic involvement in Von Recklinghausen’s disease, by the presence of plexiform neurofibroma of the upper eyelid which are pathognomonic of the disease, hypertrophy of the ipsilateral hemiface and spheno-orbital dysplasia [4]. However, complete dysgenesis of the sphenoid wing is very rare, causing slow expansion of the orbit and middle cranial fossa, ultimately with progressive herniation of the temporal lobe into the posterior orbit resulting in pulsatile proptosis [5].
Definite diagnosis of spheno-orbital dysplasia is made through imaging techniques. 3D CT imaging is the first step recommended for detection of the orbital bone defect to objectify a partial or total dysplasia or a simple thinning of the large wing of the sphenoid, and the enlargement of the middle cranial fossa.
MRI provides definite data about the localization of the bone defect, the content of the herniation and the continuity of the herniated tissue with brain [6]. In additionally, MRI examination is superior for detection of any accompanying anomalies especially nervous tumors, and the association of the herniation content with the vascular structures [7].
The management of NF-1 is a multidisciplinary approach involving the clinical geneticist, radiologist, neurologist and surgeon. The definite treatment method of spheno-orbital dysplasia is surgical intervention after determination of meningo-encephaloceles and assessment of their structure [6]. The whole herniation sac should be repaired in a multidisciplinary way with a reconstruction of the orbital apex using bone grafts.
Although prognosis is very variable, overall life expectancy is approximately half that of non-affected individuals. Tumors or cardiovascular complications are the most common causes of mortality [8]. Therefore, a monitoring of patients with this neurofibromatosis must be adapted to the patient's age to allow early management of complications.
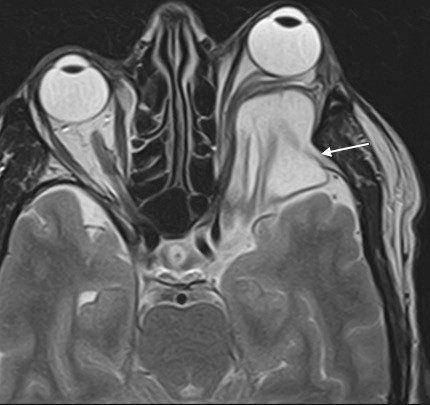
Figure 3: Brain MRI in axial T2-weighted image showing left orbital meningocele causing grade 3 exophthalmos.
Conclusion
Spheno-orbital dysplasia is a rare cause of pulsatile exophthalmos. Its finding must lead to a careful clinical and radiological examination to search a Von Recklinghausen neurofibromatosis. Conversely, in the case of known neurofibromatosis, the pulsatile nature of the exophthalmos must first suggest a spheno-orbital dysplasia.
Authors Contribution
Soufiane Belabbes (guarantor): acquisition, analysis and interpretation of data. Concept, design of study and drafting the article
Taoufik Africha: analysis and interpretation of data
Abdennasser El Kharras: revising the article critically
Brahim Zainoun: Final approval of the version to be published
Conflicts of interest: The Author(s) declare(s) that there is no conflict of interest.
Grant Information: The author(s) received no specific funding for this work.
References
- Rilliet B, Pittet B, Montandon D, Narata AP, de Ribaupierre S, Schils F, et al. Orbito-temporal facial involvement in type 1 neurofibromatosis (NF1). Neuro-Chirurgie. 2010; 56(2-3): 257-270.
- Menon AG, et al. Chromosome 17p deletions and p53 gene mutations associated with the formation of malignant neurofibrosarcomas in von Recklinghausen neurofibromatosis. Proc Natl Acad Sci USA. 1990; 87(14): 5435-5439.
- NIH Concensus Development Conference Neurofibromatosis. Conference statement. Arch Neurol 1988; 45: 575-578.
- Pinson S, Wolkenstein P. La neurofibromatose 1 (NF1) ou maladie de Von Recklinghausen. La revue de médecine interne 2005; 26: 196–215.
- Zachary D Zapatero, BS Christopher L Kalmar, Mychajlo S Kosyk, BA Anna R Carlson, MD Scott P Bartlett. Sphenoid Wing Dysplasia in the Absence of Neurofibromatosis: Diagnosis and Management of a Novel Phenotype. Plast Reconstr Surg Glob Open 2021; 9(3): e3483.
- Huang QB, Wang JG, Li XG, Zhou XD, Wang DH, Wang XY: Neurofibromatosis complicated with meningoencephalocele: one case report. Chin Med J (Engl) 120 : 2151-2152, 2007
- Alexander AA, Saettele MR, L’heureux D, Shah PA, Fickenscher KA: Rare combination of frontonasal and bilateral naso-orbital encephaloceles. J Radiol Case Rep 2011; 5: 1-7.
- Gupta N, Banerjee A, Haas-Kogan D. Pediatric CNS Tumors, Springer Verlag, 2010.

