Contraceptive Clotting in The Right Ventricle Treated with Rivaroxaban
Jihane Fagouri*, Hicham Faliouni, Meriem Boumaaz, Zakariae Laraichi, Jaouad Nguadi, Najat Mouine, Ilyas Asfalou, Aatif Benyass
Department of cardiology of the Mohamed V Military Training Hospital, Mohamed V University School of Medicine, Rabat, Morocco.
Received Date: 31/10/2021; Published Date: 02/12/2021
*Corresponding author: Jihane Fagouri, Department of cardiology of the Mohamed V Military Training Hospital, Mohamed V University School of Medicine, Rabat, Morocco.
ORCID: 0000-0001-8302-0469
Abstract
Background: Thromboembolic complications linked to hormonal contraception are well described in the literature, Deep vein thrombosis and pulmonary embolism are the most common presentations. Right ventricular clotting under hormonal treatment is rarely reported in literature, often treated with VKA.
Case presentation: a 50-year-old patient, who has in her medical history and ovarian cyst under hormonal treatment, in whom a cardiac thrombus was discovered fortuitously. The etiological research allowed us to identify a state of hypercoagulability due to hormonal treatment, the patient was put on association of rivaroxaban and aspirin with good progression.
Conclusion: Our observation elucidates one of the complications of hormonal contraception, the difficulties of managing thrombi of the cardiac cavities, the efficacy and the safety of DOAC in treating ventricular thrombosis
Keywords: Right ventricular thrombus; Rivaroxaban; Contraceptive clotting; DOAC; Ventricular thrombosis
Abbreviations: CT-scan: Computed Tomography – scan; CTA: Computerized Tomography Angiography; CT-TAP: Computed Tomography of Thorax Abdomen and Pelvis; DOAC: Direct Oral Anti-Coagulants; DVT: Deep Vein Thrombosis; LMWH: Low Molecular Weight Heparin; MRI: Magnetic Resonance Imaging; PE: Pulmonary Embolism; RA: Right Atrium; RV: Right Ventricle; VKAs: Vitamin K Antagonist; VT: Ventricular Thrombosis
Introduction
Thrombi of the right cavities are rare, and are associated with pulmonary embolism in 99% of cases [1,2]. Its presence is associated with high mortality, between 28-44% according to studies [1-3]. The incidence of right-sided floating thrombus in pulmonary embolism is estimated to be 4-8% according to the literature [4-6].
Transthoracic and transesophageal echocardiography play a major role in the detection and characterization of intracardiac masses, which may be thrombotic or tumor-like in nature, hence the interest of cardiac MRI for differential diagnosis.
In the absence of well-established recommendations, management depends on the characteristics of the thrombus, its complications, progression and the underlying pathology. Since 2010, DOAC emerged as an effective and safe alternative to VKA, they are increasingly used in treating ventricular thrombosis.
Case Report
A 50-year-old patient was admitted for the exploration of a fortuitously discovered right ventricular thrombus.
She was an obese patient with no personal or family history of thromboembolic disease, followed up for an ovarian cyst for which she was put on oral hormonal therapy.
Clinically, the patient was asymptomatic, physical examination was normal, including no signs of deep vein thrombosis.
After 3 months of hormonal treatment, the patient underwent a control abdominal-pelvic CT scan which showed the disappeanrance of the ovarian cyst, and the fortuitous discovery of an intracardiac mass.
In order to better characterize the mass, an echocardiographic complement was performed, having objectified the presence of an echogenic image at the septoapical level of the right ventricle, measuring 21mm, suggesting a thrombus.
The thrombotic nature of the mass was confirmed by cardiac MRI (Figure 1,2)
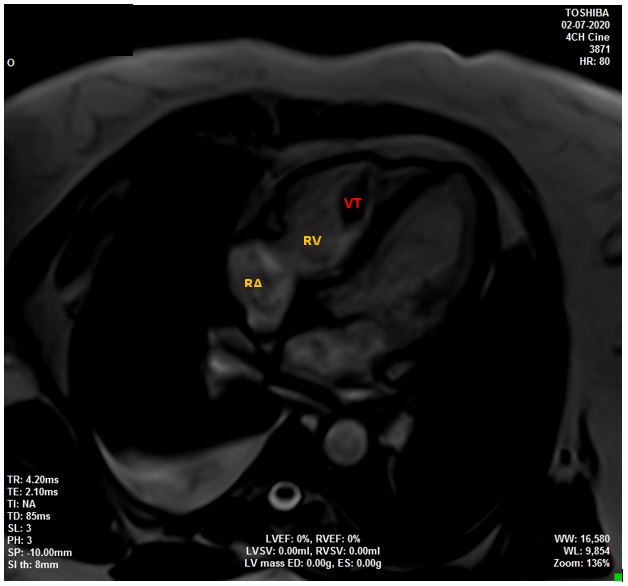
Figure 1: late gadolinium enhancement sequence of 4 chambres showing right ventricular thrombosis
RA: right atrium, RV: right ventricle, VT: ventricular thrombosis.
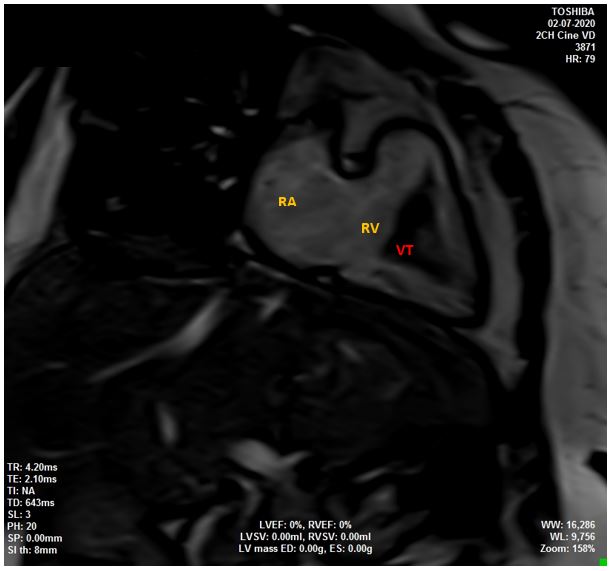
Figure 2: late gadolinium enhancement sequence of right heart 2 chambres: right ventricular thrombosis
RA: right atrium, RV: right ventricular, VT: ventricular thrombosis.
Lower limbs Doppler ultrasound was performed in search of deep vein thrombosis, which could be the cause of the thrombus, as well as a thoracic CTA in search of complications, particularly pulmonary embolism, which turned out to be unremarkable.
The biological assessment is normal, apart from an inflammatory syndrome with no associated stigma of infection.
Etiologic exploration for tumor cause, autoimmune disease, antiphospholipid syndrome, thrombophilia, or nephrotic syndrome is normal. Thus, we carried out a thoraco-abdominopelvic CT (CT-TAP) that was normal. Further biological tests were carried out such as an immunological assessment, the assay of tumor markers, 24-hour proteinuria, the assay of protein C and S and the search for resistance to activated protein C, it was without particularities.
Therapeutically speaking, hormonal treatment was suspended, the patient was put on LMWH at a curative dose for 3 weeks.
The first echocardiographic check-up did not show any decrease in thrombus size. The patient was transitioned to the combination of NOAC (rivaroxaban) and aspirin with a good progression.
Discussion
Right ventricular thrombus is an uncommon pathology, increasingly detected since the advent and development of echocardiography. The diagnosis of right ventricular thrombi before the imaging era was autopsy [5].
Multimodal cardiovascular imaging has become a mainstay in the diagnosis of intracardiac masses. Transthoracic echocardiography, a non-invasive, rapidly achievable examination, available at the patient's bedside in intensive care units, is the first-line examination for the detection of intracardiac thrombosis with a sensitivity of 50-60% [2].
There are 3 types of right cavity thrombus [7,8]: Type A: serpentine shape, very mobile, often associated with DVT and PE. This suggests that this type of thrombus is always in transit in the RV from a DVT. Type B: Non-mobile, builds up in situ, often on a pathological heart. Type C: rare, myxoma-like appearance, very mobile.
Transoesophageal echocardiography has the advantage of being more sensitive and more precise for estimating the size of right cavities thrombus [2]. Cardiac MRI, due to its high signal resolution, allows a better characterization of intracardiac masses and their mobility [9].
Thrombi of the right ventricle are seldom reported in the literature. For our patient, and after exhaustive etiological research, the etiology retained is oral contraception. A hormonal origin has also been implicated in a young man [10] candidate for sexual reassignment surgery under testosterone. And in 2 young patients on oral contraception, in whom the etiological assessment led to the respective diagnosis of an antiphospholipid syndrome [11] and a post-traumatic myocardial contusion [12]. Right ventricular thrombi have also been reported in the setting of myocardial infarction extended to the right ventricle [13], progressive neoplasia, nephrotic syndrome [14], hypereosinophilic syndrome [15], and in Behçet's disease [16].
The management of right cavity thrombi remains controversial in the absence of well-codified studies and recommendations. It usually involves anticoagulant treatment combined with specific treatment of the underlying pathology. The use of heparin or other anticoagulants may be considered in patients with a poorly mobile thrombus, as it is the case with our patient, she was treated with association of rivaroxaban and aspirine. According to a meta-analysis, there is no significant differences in the efficacy and the safety of use of NAOC compared to VKA [17]. However, curative anticoagulation for type A thrombi should be carried out carefully, given the slow duration of action, and the unpredictable evolution with a risk of massive pulmonary embolism [5]. Surgery remains the choice if there are difficulties in establishing the differential diagnosis with a tumour mass, particularly myxomas, or if anticoagulant treatment fails.
Our case has shown the interest of imaging in the diagnosis of intracardiac masses. The risk-benefit balance must be assessed before any prescription of oral contraception, given its potentially fatal complications. Etiological research must be broad. The use of DOAC is promising, it seems safe and does not require biological monitoring. A prospective, randomised study is crucial to better guide the management of these patients.
Conclusion
The presence of thrombus in the right cavities is an infrequent entity, threatening in particular to highly mobile thrombi, and associated with pulmonary embolism in 99% of cases.
Transthoracic and transesophageal echocardiography are mainstays for positive diagnosis, and cardiac MRI is important for confirmation and for differential diagnosis with cardiac tumors.
There are no recommendations for establishing a good therapeutic strategy. Large scale randomized studies are needed to better stratify the management of these patients, and to evaluate the efficacy and the safety of using DAOC for ventricular thrombosis
- F and H.F wrote the manuscript with input from all the authors, M.B, J.N and Z.L helped in collecting data, N.M analysed the data, I.A performed MRI and helped choosing figures, A.B supervised the findings of this work
- All authors contributed to the design and implementation of the research, to the analysis of the results, and have approved the submitted version
Competing interests: The authors declare that they have no competing interests
Grant information: The author(s) received no specific funding for this work
Acknowledgement:
Department of cardiology of the Mohamed V Military Training Hospital, Mohamed V University School of Medicine, Rabat, Morroco.
References
- de Vrey EA, Bax JJ, Poldermans D, van der Wall EE, Holman ER. Mobile right heart thrombus and massive pulmonary embolism. Eur J Echocardiogr. 1 juin, 2007; 8(3): 229‑231.
- Rose PS, Punjabi NM, Pearse DB. Treatment of right heart thromboemboli. Chest. Mars 2002; 121(3): 806‑814.
- Chartier L, Béra J, Delomez M, Asseman P, Beregi JP, Bauchart JJ, et al. Free-floating thrombi in the right heart: diagnosis, management, and prognostic indexes in 38 consecutive patients. Circulation. 1999; 99(21): 2779‑2783.
- Ferrari E, Benhamou M, Berthier F, Baudouy M. Mobile thrombi of the right heart in pulmonary embolism: delayed disappearance after thrombolytic treatment. Chest. 2005; 127(3): 1051‑1053.
- Pierre-Justin G, Pierard LA. Management of mobile right heart thrombi: a prospective series. Int J Cardiol, 2005; 99(3): 381‑388.
- Torbicki A, Galié N, Covezzoli A, Rossi E, De Rosa M, Goldhaber SZ, et al. Right heart thrombi in pulmonary embolism: results from the International Cooperative Pulmonary Embolism Registry. J Am Coll Cardiol. 2003; 41(12):2245‑2251.
- Ruiz-Bailén M, López-Caler C, Castillo-Rivera A, Rucabado-Aguilar L, Ramos Cuadra JA, Lara Toral J, et al. Giant right atrial thrombi treated with thrombolysis. Can J Cardiol, 2008; 24(4): 312‑314.
- Naeem K. Floating thrombus in the right heart associated with pulmonary embolism: The role of echocardiography. Pak J Med Sci, 2015; 31(1): 233‑235.
- Masse et thrombus cardiaques en imagerie en coupe - ScienceDirect [Internet]. 2020.
- Mamdani N, Krell M, Polomsky M, Horgan S. Right Ventricular Thrombus: A Complication of Gender Reassignment Therapy. J Am Coll Cardiol. 2018; 71(11 Supplement): A2472.
- Right atrial thrombus masquerading as a myxoma. Synergistic effects of hormonal contraceptives and anti-phospholipid antibodies | JACC: Journal of the American College of Cardiology [Internet]. 2020.
- Masson E. Calcified right ventricular mass and pulmonary embolism in a previously healthy young woman [Internet]. EM-Consulte. 2020.
- Tsang BK-T, Platts DG, Javorsky G, Brown MR. Right ventricular thrombus detection and multimodality imaging using contrast echocardiography and cardiac magnetic resonance imaging. Heart Lung Circ. 2012; 21(3): 185‑188.
- Lempp S, Schwenger V. Isolated right ventricular thrombus in an adult patient with nephrotic syndrome: a case report. J Med Case Rep [Internet]. 2017 [cité 19 sept 2020];11.
- From an isolated right ventricular thrombus to the diagnosis of the hypereosinophilic syndrome [Internet]. [cité 19 sept 2020].
- Mendes LA, Magraw LL, Aldea GS, Davidoff R. Right Ventricular Thrombus: An Unusual Manifestation of Behçet’s Disease. Journal of the American Society of Echocardiography. 1994; 7(4): 438‑440.
- YANG Q, He L, Liang Y. Effectiveness and Safety of Non-Vitamin K Antagonist Oral Anticoagulants Compared to Vitamin K Antagonists for the Treatment of Ventricular Thrombus: A Systematic Review and Meta-analysis of Observational Studies [Internet]. In Review; 2020 déc [cité 1 juin 2021].

