STEMI and Silent Myocardial Ischemia: A Clinical Case Report and Literature Review
Larsen Clarck Moumpala Zingoula*, Alkory Ould Sidi M’hamed, Asmaa Ameur, Sanae ES Sebbani, Lassana Konate, Ponce Elisée Konan, Nadia Fellat, Rokya Fellat, Adil Bensouda
Department of Cardiology, National League for the Fight against Cardiovascular Diseases, Centre Atpitalier Universitaire Ibn Sina, RABAT
Mohammed V University of Rabat, Faculty of Medicine and Pharmacy, Rabat, Morocco
Received Date: 29/10/2021; Published Date: 23/11/2021
*Corresponding author: Larsen Clarck Moumpala Zingoula, Department of Cardiology, National League for the Fight against Cardiovascular Diseases, Ibn Sina University Hospital center, Mohammed V University of Rabat, Faculty of Medicine and Pharmacy, Rabat, Morocco
ORCID: Larsen Clarck MOUMPALA ZINGOULA - https://orcid.org/0000-0001-6582-7218
Abstract
Infarctoid chest pain remains the cardinal sign of SCA, in its absence it is frequently dyspnea that reveals a consummate infarction. However, it may be that both are missing, depending on the patient's history frequently in diabetics at the neuropathy stage, to be revealed only by atypical pain. The absence of both signs, with enzymatic movements, signs the silent infarction. It is therefore unprecedented to note in a patient, without diabetic neuropathy, to be a victim of silent myocardial ischemia revealed by a thromboembolic complication, hence the interest of our case report with his journey on his management.
Keywords: SETMI; Post-IDM; Silentmyocardial schemia; Coronarography; Viability; Angioplasty
Introduction
Acute Coronary Syndrome (ACS) is one of the most common cardiovascular diseases, a realpublic health problem withnearly 12 million deaths attributed per year worldwide and 2500 acute coronary syndromes per million inhabitants [1]. Divided into two, the SCA comprises two nosology among which Myocardial Infarction (MDI) with ST overshift ("STEMI", AngloSaxon acronym for "ST-segment elevation myocardial infarction") [2] whose chest pain is the cardinal clinical manifestation accompanied by electrical modification of the ST segment on theelectrocardiogram (ECG) with Q-wave monitoring and associated with an elevation or decrease of a biomarker of myocardial necrosis (troponin Tc or Ic, preferably ultrasensitive).
We report, the clinical course to the therapeutic of a patient subject to a silent myocardial ischemia revealed by a thromboembolic complication.
Clinical Case
This is a 57-year-old patient, non-diabetic, chronic smoker for 30 years to 1 pack of cigarettes per day in withdrawal for 2 months. He consults following the occurrence in family of a deviation of the mouth accompanied by hypotonia of the left hemibody with remission of signs in less than 1 hour on the way to the hospital where he benefits from an angio-cerebral CT without particularities, then referred to our department where the non-invasive exploration (ENI) cardiovascular motivates his hospitalization for his care.
It does not report any notion of typical or atypical chestpain, nor dyspnea in the previous months.
On clinical examination, it is eupneic, not suffering, good blood pressure figures at 134/88 mmHg, FC 104 bpm, cardiovascular and pleuropulmonary examination is normal, sur theelectrocardiogram at admission on objective a QS aspect in anteroseptoapical (ASA), a persistent ST shift in circumferential, without basal abnormality; then on other objective ECGs electrical changes in lower lateral (Figure 1,2) without cli nic manifestation. To biology marked by a troponin at 524 pg / ml in kinetics of decrease at 326 pg / ml, a casuelle blood glucose at 1 mg/dl, and a glyque hemoglobinat5.8%, Creatinine at 7.7 mg / l (GFR at 110 ml / min / 1.73m2).

Figure 1: 1st ECG: QS aspect in ASA and over persistent ASA shift, lateral and lower, soit a postIDM in circumferential (before diagnostic coronary angiography).

Figure 2: 2nd ECG: lower lateral modificationby QS aspect (before diagnostic coronary angiography).
Trans thoracic Doppler echocardiography (ETT) is objective a left ventricle of limit size, nothypertrophied, seat of an early apical aneurysm with Akinesiasin apical and adjacent segments, middle segments of the anteroseptal (AS), inferoseptal (IS) and inferior walls (Inf), as well asanapical thrombus of 7x 30 mm, with a frejection action severely altered in SBP (Figure 3).

Figure 3: Image of the ETT: cuts 2 cavities, with the presence of a thrombus of 7x30mm lining the apex (fat red arrow).
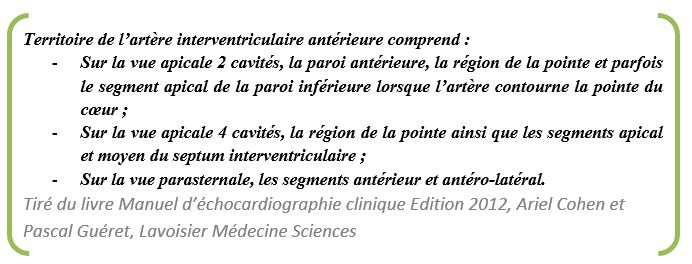
Coronary angiography objectifies a normal cal ibre network witha very tight lesion of the interventricular artery (IVA) medium (Figure 4).

Figure 4: Image of coronary angiography: very tight stenosis of the average IVA (double red arrow).
Magnetic resonance imaging (MRI) left ventricle (VG) dilated and spherized without true aneurysm; Anterior akinesia (apical, median and part of the basal segment), AS, IS and apical. Apical dyskinesia. Aminated apical wall (<4mm) in AS, anterior and apical. LVEF 27%.
1st passage of Gadolinium: defect of myocardial perfusion at the septoapical (SA) and anteroapical (AA) level in favor of no-reflow. Intra-VG infusion defectin connectionwith apical thrombus.
Late sequences:
- Late transmural elevation at the level of the wall Antérieure, AS, ISA, apical and apical segments of the wall IL and Inf. No-reflow at theapex;
- Late sub-endocardial enhancement (<50%) at the level of the ISM wall;
- Large flat thrombus lining the AS wall, a thrombus at the level of the anteroapical wall, a rounded thrombus gros of 39x23mm at the level of the ISA wall. (Figure 5).
Angioplasty: revascularization by placing an active Stent on the average IVA (Figure 6).
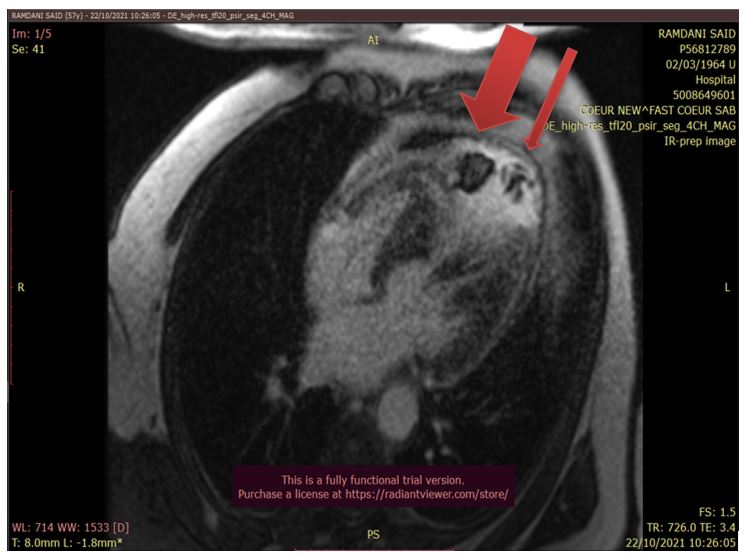
Figure 5: Cardiac MRI image for objectifying viability of intra-VG thrombi including a large thrombus (double red arrow).
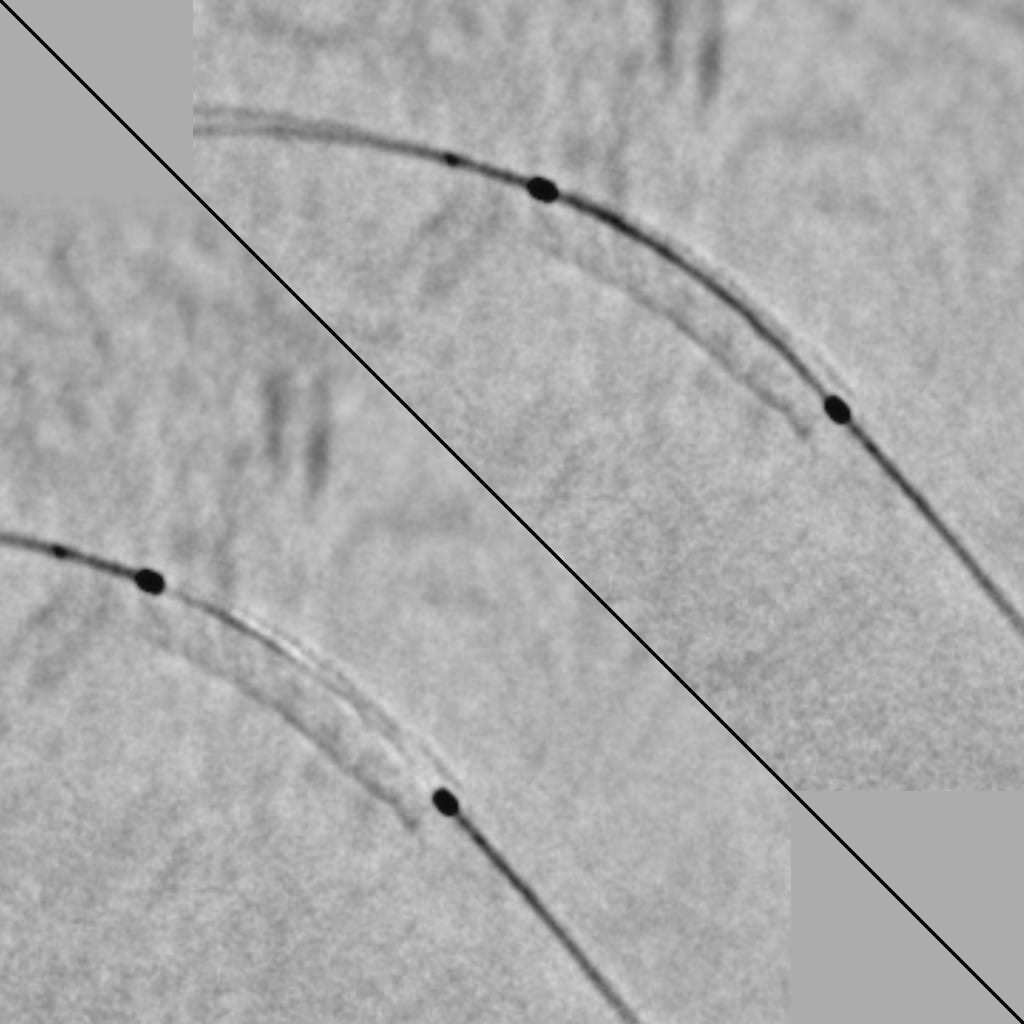
Figure 6: Image of the 2nd coronary angiography for angioplasty with the establishment of an active Stent.


Discussion
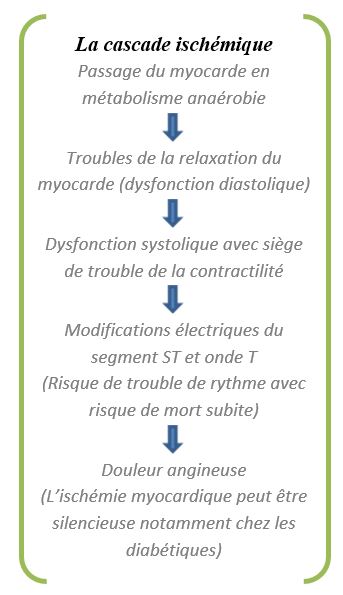
SCA means any chest pain of anginal appearance occurring de novo, prolonged or recently worsening in a patient with or without coronary history, most often accompanied byECGabnormalitieswith type of st+ segment overshift for STEMI, a fortiori if the ECG was performed in per-critical [3]. Among the SCAs, we have the STEMI to which our patientissubjected, in circumferential, following an attack of the guilty artery posing a problem of complete interruption of the blood flow resulting in a necrosis of the territory downstream. This will be followed by the ischemic cascade which will result in the clinical expression made of infarctoid chest pain (ITD) (which is only the immergée part of theiceberg): infarctoid chest pain is the master symptom of Myocardial Ischemia (MI).
In particular, the absence of angina does not mean the absence of coronary artery disease. On the other hand, in proven coronary patients, the absence of angina does not necessarily imply a benign prognosis. Conversely, the severity of the symptomatology isnot correlated with the spread of coronary artery disease and even less with its severity. Asymptomatic or silent myocardial ischemia (IMS) is defined by the presence of a subshift of the ST segment without contemporary pain [4]. On the other hand, Dr COHN, one of the first researchers onmyocardial disease, deended the IMS as follows: Evidence (especially by various laboratory means) of myocardial ischeddisease or its complications, myocardial infarction, heart failure, ristheusand sudden death, without chest pain or other evalent anginal symptoms (e.g., dyspnea). I1 has developed an IMS classification, dividing patients into three types. Type 1 who is the patient totally asymptomatic, the one who has never had chest pain, nor dyspnee with documented coronary artery disease e. Next, we note type 2, which is the asymptomatic post-infarction patient. I1 is a patient who could have had angina before the infarction and at the time of his infarction but who subsequently became asymptomatic even with an electedro cardiographic evidence (or by other laboratory means) of myocardial ischemia. Finally, there is the patient with angina and pisodes of myocardial ischesilencieuse [5]. By its definition, we attach IMS to the context of our patient who, without having suffered from any form of clinical expression of ischemia, makes a STEMI revealed at the post-IDM stage by an event of thromboembolic complications. In reference to his troponin level at admission with a decrease in kinetics, and an aspect of necrosis consumed at the ECG, let's classify our patient in the type 1, a STEMI in asymptomatic circumferential, passed unnoticed, despite the electrical changes during the same day of his admission. On this, Dr BEAUDRY, puts forward three possible causes of IMS: a) an adéquat insufflating stimulus; b) a defect in the peripheral perception of pain (by exemple: diabetic neuropathy) and c) a defect in the central transmission in the painful sensation. The third possibility applies specially to type 1, to the patient who has never had angina or dyspnea as a symptom related to myocardial ischemia [6]. It was later shown that mental stress or cigarette consumption led to episodes of IMS. The circadian rhythm is also involved by a significant increase in heart rate and systolic blood pressure may precede the onset of IMS episodes of daily life. And the threshold of ischemia depends on the duration of the increase in heart rate [4]. Our patient is not diabetic, so he would not suffer from diabetic neuropathy, moreover, he is inveterate smoker.
As for the endocavitic thrombus, its formation is classically favored by the elements of the Virchow triad: blood stasis, endothelial lesion and hypercoagulability. These three elements are present during the acute phase of infarction. That is an estimated 12.2% of patients with previous STEMI have an endocavitic thrombus 7.
"On MRI, gadolinium does not penetrate the thrombus, late enhancement sequences show necrosis in hypersignal and thrombus in frank hyposignal" [7] (Figure 5).
These thrombi are mainly located next to the tip of the VG, concern anterior IDMs, with extensive infarction and only revascularization seems to limit the frequency of thrombi [7].
Support
During his hospitalization, we objectified kinetic disorders such as dyskinesia and akinesia as well as intra VG thrombus apical to ETT.
The question of myocardial viability arises in case of akinesia of segmental contraction in the infarcted area in connection with stenosis or coronary occlusion. The aim is to determine whether or not coronary revascularization could restore contractile function. In addition, the assessment of the size of the IDM is essential in the acute phase, as it conditions ventricular remodeling and clinical prognosis [7]. Ifa myocardial segment of the same territory of the guilty artery was viable, the patient underwisted a revascularization by angioplasty with the establishment of an active Stent on the average IVA.
Oral anticoagulation was indicated over the long term for up to six (6) months, during which time it would be assessed by a repeat of imagingexaminations. As for the rest of its therapeutic management, it has been in line with the latest recommendations of the European Society of Oncologyon IDMs with over-lag of the ST 8segment.
Conclusion
Silent myocardial ischemia is common but not often reported, according to the case of our patient. How many patients do not consult at the stage of complications of an IDM consumed that has gone unnoticed? It remains to prove the causes in a patient without diabetic neuropathy, as well as to make the link between silent ischemia and smoking. The fact remains that silent myocardial ischemia is a silent killer that is not sufficiently denounced.
References
- Artigou JY, Monsuez JJ, et al. Cardiology and Vascular Diseases. French Society of Cardiology. Premium offer. 2020 Edition, Elsevier Masson SAS.
- Vincent REYT. Crohn's disease. Prescription analysis, gastroenterology, Elsevier Masson 2018.
- Attias D, Lellouche N, et al. Vascular cardiology. The iKBReference. 8th EDITION – 2018. VG Editions.
- Helft G, Metzger JP. Silent myocardial ischemia. Encyl Méd Chir (Editions Scientifiques et Médicales Elsevier SAS, Paris, tous droits réervés), Cardiologie, 11-030-C-10, 2003; 8 p.
- Cohn PF. The concept and pathogenesis of active but asymptomatic coronary artery disease. Circulation 1987; Suppl.1175: 2.
- Beaudry RP. Silent myocardial ischemia. The Canadian Family Physician 1991; 37.
- Laissy JP, Furber A, et al. Cardiac imaging. Imaging in sections: computed tomography, MRI. French Society of Cardiology. Edition 2021, Elsevier Masson SAS.
- Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J, 2017.

