Multiple Cutaneous Hemangioma with Chronic Diffuse Intravascular Coagulation During Pregnancy: A Case Report and Literature Review
Fufen Yin, Junshu Xie, Xiuju Yin, Xiaohong Zhang*
Department of Obstetrics and Gynecology, Peking University People’s Hospital, China
Received Date: 19/10/2021; Published Date: 19/11/2021
*Corresponding author: Prof. Xiaohong Zhang, Department of Obstetrics and Gynecology, Peking University People’s Hospital, Xizhenmen South Street, Xicheng District, Beijing, China
Abstract
Pregnancy can increase the incidence of diffuse intravascular coagulation during hemangioma. In the present case a diagnosis of an adult multiple cutaneous hemangioma during pregnancy was made. We were not able to identify a similar case in the very sparse literature on this disease with chronic diffuse intravascular coagulation delivered by vaginal. Here, we report a patient who experienced chronic diffuse intravascular coagulation during pregnancy. A 27-year-old female 37 weeks pregnant, presented with a chronic DIC demonstrated by pregnancy tests. She was delivered by vaginal at 39 weeks of gestation. Hormonal and vascular changes of pregnancy may exacerbate multiple hemangiomas. Patients with multiple cutaneous hemangioma should be closely monitored during and after pregnancy as increased incidence of DIC during pregnancy. Hemangioma with chronic DIC is not an absolute indication of cesarean section. And the choice of delivery method for such patients is still controversial.
Keywords: Diffuse intravascular coagulation; Multiple hemangioma; Pregnancy
Introduction
Cutaneous hemangioma is one of the most common types of benign tumor. Pregnancy, because of the physiological changes, is a recognized risk factor coinciding with the development of a rapid onset of symptoms from these normally asymptomatic lesions. Local modifications in the angioma are suggestive signs preceding the onset of general thrombotic complications. So, closely monitor during and after pregnancy is essential in planning optimal therapy and preventing morbidity for both mother and fetus. We report a case of a multiple cutaneous hemangioma with chronic DIC (diffuse intravascular coagulation) during pregnancy that was delivered by vaginal and we also review the current literature on pregnancy- related hemangiomas.
Case Report
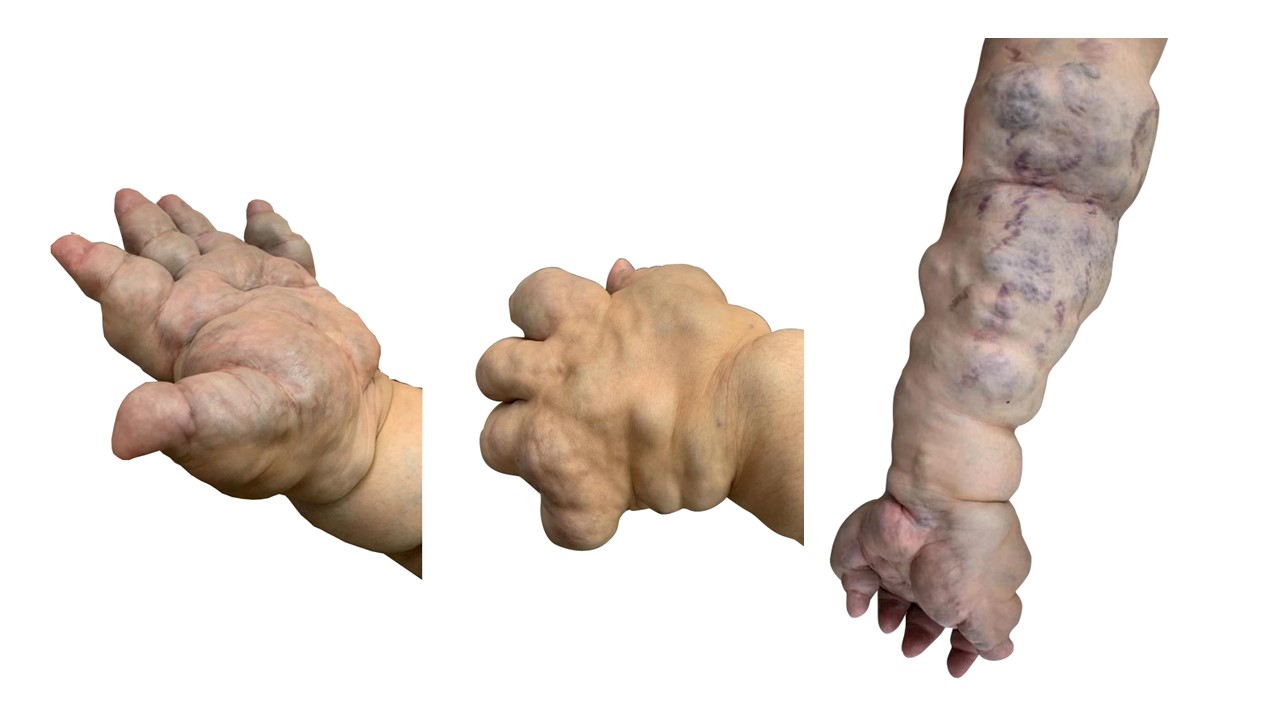
The patient was born with multiple hemangiomas of the left upper limb and chest, and hemangioma increases with age. An otherwise healthy, non-obese 26-year-old woman (gravida 1, para 0), at 14 weeks gestation was admitted to Peking Union Medical College Hospital’s department of obstetrics and gynecology as she felt a swelling in her left upper limb and the hemangioma in pregnancy was significantly larger than before. Multiple cutaneous hemangiomas on the left upper limb, left underarm and left chest were detected by clinical examination, which revealed no other notable findings except for her pregnant status (Figure 1). Routine biochemistry was normal, and D- dimer (79.37mg/L), fibrinogen (FIB-C=1.12g/L), considering chronic DIC, subcutaneous injection of tachypline 0.4qd was started at 15 weeks gestation. D-dimer was regularly monitored with a downward trend, and fibrinogen was normal. D-dimer was 41.7mg/L at 27 weeks gestation, and subcutaneous injection of tetrapulin 0.4 bid was used instead. D-dimer was monitored with a gradual decline, and D-dimer 1966ng/mL was re-examined 37 weeks gestation. Fetal ultrasound (US) examination at 23 weeks of PLA general hospital suggested that a hyperechoic mass with a size of about 2.1*3.2*1.9cm could be seen below the left diaphragm and behind the gastric alveoli, indicating that the isolated lung was not excluded. The patient was regularly reviewed with ultrasound. Fetal US at 34+4 weeks of gestation suggested medium to high echo below the left diaphragm, with a size of about 4.2*2.1*2.4cm. Physical examination on admission: Body temperature: 36.3℃, pulse: 82 beats/min, respiration: 18 beats/min, blood pressure: 123/74mmhg. Multiple cutaneous hemangiomas on the left upper limb, left underarm and left chest. Cardiopulmonary auscultation showed no abnormality, no abdominal tenderness and rebound pain. Specialist examination: Uterine height: 31cm, abdominal circumference: 97cm, fetal head position, fetal heart 145 times/min. Posterior position of the cervix, in the medium, 80% of the uterus was eliminated, the uterine mouth was not opened, S-0.5, the fetal membrane was not broken, it was estimated that the fetus was 3200g. Pelvic measurement: DC>11.5cm, TO=9cm, middle arc of sacrum, no cohesion in lateral wall, interischial spine diameter 10cm. Irregular contractions. On examination she was pregnant with uterine height corresponding to gestational age and a positive fetal cardiac activity. Relevant factors when considering delivery way included the presence of increasing clinical symptoms in a pregnant woman. In accordance with the patient’s preferences, Vaginal delivery was recommended and a full-term mature male live baby was delivered in ROA position at 39+3 weeks of gestation. The newborn had no abnormal appearance and the APGAR score was 10 at 1 minute, 5 minutes and 10 minutes. After delivery, the placenta and fetal membranes were intact and the appearance was normal.
Discussion
Hemangiomas are benign tumors of thinwalled blood vessels, they are common in infants, and commonly present on the face and scalp, usually spontaneously egressing, and in the adult, they can occur anywhere on the skin. Research has suggested a possible role for estrogen as a mediator for vascular proliferation and hemangioma formation. According to estrogen and progesterone are significantly elevated during pregnancy, this may potentially explain the rapid growth of this lady’s hemangioma and the chronic DIC during her pregnancy. As for this patient, the enlarged hemangioma during pregnancy than before may due to the hormonal changes. So, for patient with hemangiomas, closely monitor during and after pregnancy is essential in planning optimal therapy and preventing morbidity for both mother and fetus.
Disseminated Intravascular Coagulation (DIC) is a condition characterized by the systemic intravascular activation of blood coagulation. Intravascular fibrin clots are formed, leading to the thrombotic obstruction of small- and midsized vessels. Furthermore, DIC can result in compromised blood supplies to organs and can contribute to multiple organ failure. DIC is divided into acute type and chronic type. There is no clear classification standard between them. DIC are classified as chronic if their performance is prolonged for more than a week or even several months. According to the laboratory examination, the acute type usually presents typical wasting coagulation disorder with obvious bleeding symptoms. However, the chronic type often had no consumption signs, but increased coagulation factors. The pathological process of DIC has been estimated to occur in up to 30% to 50% of cases of severe sepsis, which is the most common cause of DIC. Up to 20% of patients with metastasized adenocarcinoma or lymphoproliferative disease also suffer from DIC. The third cause of DIC is trauma, pancreatitis, malignancy, liver disease, giant hemangioma. Due to a large amount of blood congestion, blood stasis in hemangioma patients, primary DIC could be induced. In this case of the patients, she felt a swelling in her left upper limb and the hemangioma in pregnancy was significantly larger than before, without ecchymosis and bleeding tendency. Hormonal and vascular changes of pregnancy may exacerbate hemangiomas and coagulation function change. Patients with multiple cutaneous hemangioma should be closely monitored during and after pregnancy as increased incidence of DIC during pregnancy.
To the best of our knowledge, we could not find any other similar cases in the literature. In this case, although the hemangioma was large, it was confirmed after delivery that no fetal growth restriction, fetal malformation and other complications were caused after active anticoagulant treatment. It can be seen that hemangioma with DIC is not an absolute indication of cesarean section. Once hemangioma complicated with DIC was found, active anticoagulation should be carried out under close monitoring. If the mother and child were in good condition, pregnancy can be continued under close observation. But The choice of delivery method for such patients is still controversial.
References
- Beerepoot S, van Dooren S, Salomons GS, Boelens JJ, Jacobs EH, van der Knaap MS, et al. Metachromatic leukodystrophy genotypes in The Netherlands reveal novel pathogenic ARSA variants in non-Caucasian patients. Neurogenetics, 2020; 21(4): 289-299.
- Shaimardanova AA, Chulpanova DS, Solovyeva VV, Mullagulova AI, Kitaeva KV, Allegrucci C, et al. Metachromatic Leukodystrophy: Diagnosis, Modeling, and Treatment Approaches. Frontiers in medicine, 2020; 7: 576221
- Alfadhel M, Almuqbil M, Al Mutairi F, et al. The Leukodystrophy Spectrum in Saudi Arabia: Epidemiological, Clinical, Radiological, and Genetic Data. Front Pediatr. 2021; 9: 633385.
- Harrington M, Whalley D, Twiss J, et al. Insights into the natural history of metachromatic leukodystrophy from interviews with caregivers. Orphanet J Rare Dis. 2019; 14(1): 89.
- Narayanan DL, Matta D, Gupta N, et al. Spectrum of ARSA variations in Asian Indian patients with Arylsulfatase A deficient metachromatic leukodystrophy. J Hum Genet. 2019; 64.
- Richards S, Aziz N, Bale S, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015; 17.
- Dehghan Manshadi M, Kamalidehghan B, Aryani O, Khalili E, Dadgar S, Tondar M, et al. Four novel ARSA gene mutations with pathogenic impacts on metachromatic leukodystrophy: a bioinformatics approach to predict pathogenic mutations. Ther Clin Risk Manag, 2017.

